![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
Pericardium
|
encloses the heart and root of the great vessels
|
|
|
2 layers of pericardium
|
-fibrous pericardium (outer tough fibrous tissue)
-serous pericardium (inner smooth layer) |
|
|
serous pericardium composed of a parietal and visceral layer, space between two layers contains what?
|
A thin layer of lubricating fluid called pericardial fluid
-about 30cc |
|
|
True or False: the Apex is formed by the tip of the left ventricle of the heart.
|
True
|
|
|
Four boarders of the Heart
|
~Right border: right atrium and in line with the superior and inferior vena cavae
~Inferior border is almost horizontal and formed by the Rt Ventricle, small part of Lt Ventricle at Apex. ~Lt border , Lt Ventricle and part Lt Atrium ~Superior border made of both Atria. |
|
|
Three layers of heart
|
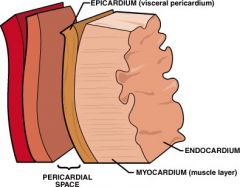
Endocardium, Myocardium, Epicardium
|
|
|
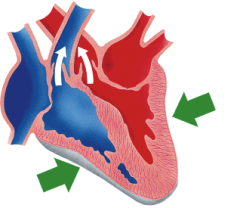
Flow of Blood through heart
|
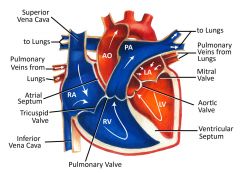
|
|
|
Two main arteries that supply the heart
|
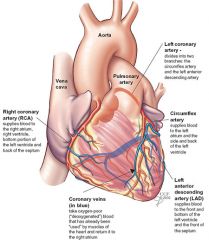
~Left Main Coronary Artery- LCA
~Right Coronary Artery- RCA |
|
|
LCA gives rise to...
|
Left Anterior Descending- LAD and Left Circumflex-LCX
|
|
|
RCA gives rise to...
|
Posterior Descending Artery PDA
|
|
|
Variances in coronary artery anatomy
|
85% are RCA dominant
8% Circumflex is dominant 7% both RCA and Circumflex give rise to posterior descending branches. |
|
|
what makes skeletal muscle cells different then cardiac muscle cells
|
Cardiac cells only have one or two nuclei, skeletal cells have many nuclei.
|
|
|
what does the myocardial cell membrane contain that establishes electrical continuity within the myocardium
|
Intercalated disk
|
|
|
The Basic unit of electrical stimulation
|
Action Potential, ion fluxes through specific ion channels create depolarization, the trigger for muscular contraction.
|
|
|
Myocardium contains 3 types of electrophysiologic types:
|
pacemaker cells: SA and AV nodal cells
Specialized rapidly conducting tissues: Purkinje fibers Cardiac muscle cells themselves |
|
|
The Heart is innervated (the distribution or supply of nerve fibers or nerve impulses to a body part) by both...
|
Sympathetic and Parasympathetic nervous system
|
|
|
Systole is...
|
Ventricular contraction, when the ventricles push blood out into the pulmonary and systemic circulation
|
|
|
Diastole is...
|
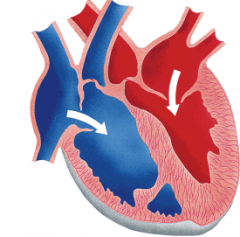
Ventricular relaxation, when the ventricles are filling up with blood again.
|
|
|
First heart sound, S1, caused by...
|
nearly simultaneous closure of the tricuspid and mitral valves, preventing backflow of blood into the atria.
|
|
|
second Heart sound S2.
|
After blood has ejected, the aortic and pulmonic valves close.
|
|
|
Period from S1-S2
Period from S2 to the next S1 |
Systole
Diastole |
|
|
Cardiac Auscultation
|
Listening to the sounds of the heart
|
|
|
Electrocardiogram-ECG
|
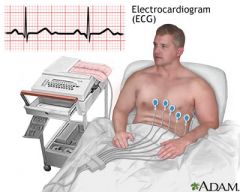
Diagnostic method to record the heart's electrical activity. Surface representation of myocardial depolarization and re-polarization.
12 lead ECG is standard, placed at different angles |
|
|
disorders ECG can identify
|
-conduction abnormalities
-cardiac dysrhythmias -cardiac hypertrophy -pericarditis -electrolyte imbalances -myocardial ischemia -myocardial infarction (MI) and extent of recovery from MI |
|
|
Most Common Heart Disease
|
Ischemic Heart Disease
|
|
|
Insufficient myocardial perfusion (blood flow) that causes 600,000 deaths per year.
|
Ischemic Heart Disease!
|
|
|
Patients with Ischemic Heart Disease present with...
|
Angina ( cardiac chest pain)
Myocardial infarction Congestive heart failure Sudden death |
|
|
Decreased blood flow to tissue resulting in decreased tissue oxygen and increased build-up of tissue metabolites that are harmful
|
Ischemia
|
|
|
Infarction
|
decreased blood flow to a tissue to such and extent that tissue death occurs
|
|
|
Slowly progressive disease that affects the arteries, in which fatty deposits and fibrous tissue occlude the lumen, and cause of angina pectoris.
|
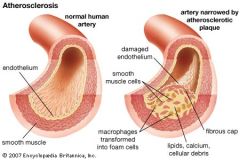
Atherosclerosis
|
|
|
Thrombosis
|
Clotted blood and involves platelets, and fibrin produced from the blood coagulation system.
|
|
|
Embolus
|

Any substance that circulates in the bloodstream and becomes lodged with in a vessel lumen resulting in occlusion
|
|
|
Two most common lesions of atherosclerosis
|
Fatty streak and fibrous plaque
|
|
|
Fatty lesions
|
-most have them by age 20
-yellow discoloration on the inner surface of the artery -precursor lesion that develops into fibrous plaque |
|
|
Fibrous Lesion
|
Fibrous Plaques are the pathologic lesions that caus the morbidity and mortality of atherosclerosis.
-most common in the aorta, then coronary arteries, popliteal, descending thoracic aorta, internal carotid, and cerebral vascular arteries |
|
|
Risks for developing atherosclerosis
|
modifiable risk:
Hyperlipidemia, hypertension, cigarettes, and diabetes non-modifiable risk: Men, age, and family history of coronary disease minor risk: obesity, sedentary lifestyle, and stressful behavior |
|
|
Angina Pectoris (cardiac chest pain) results from...
|
Imbalance between myocardial oxygen supply and demand
|
|
|
most common cause of angina pectoris
|
inability of atherosclerotic coronary arteries to supply heart with oxygen-rich blood, in conditions of demand.
can also occur with valvular disease, hypertension, and coronary artery vasospam. |
|
|
Pain of angina described as...
|

Pressure, heaviness, or squeezing sensation
|
|
|
Pain location in substernal area, percorium, or epigastrium with pain radiating to what areas?
|
Left arm, jaw, and neck.
usually only lasting a few minutes |
|
|
Angina may be provoked by
|
Exterion, emotion, cold weather, and eating or smoking.
|
|
|
Relive angina by
|
resting, remove provoking factors, or the drug nitroglycerin.
|
|
|
Acute Myocardial Infarction (AMI)
|
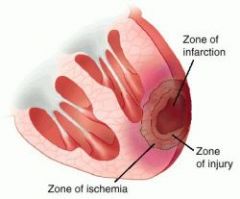
result of prolonged ischemia that has led to irreversible necrosis of the myocardial tissue.
|
|
|
85% of AMI cases is associated with
|
occluded coronary artery, mainly atherosclerosis
|
|
|
how many people in US suffer from MI each year, and what is the hospital mortality rate?
|
over 1.5 million people and around 15%
|
|
|
which area of the heart is most commonly affected by MI?
|
the left ventricle
|
|
|
Clinical presentation for MI
|
-Pale
-Diaphoretic(sweaty) -Anxious maybe increased heart rate, respiration, and blood pressure. |
|
|
what are the 2 main diagnostic test used for diagnosing MI
|
ECG: serial ECG tracings to show evolution of myocardial damage. "Q-waves" develop with infarction and necrosis. can locate area of damage
Cardiac serum protein markers: proteins presented in blood for a defined period of time after injury and during injury. |
|
|
a protein and enzyme that show up in blood after a few hours of injury
|
Myoglobin: muscle protein, dissipates within a day
Creatine Kinase: enzyme last for 3 days in blood |
|
|
Troponin
|
Early and late marker: Cardiac muscle enzyme released 6 hours after injury, stays elevated for about a week
|
|
|
Stable Angina
|
occurs with exertion, rest can help heal
|
|
|
Unstable Angina
|
Pain at rest and/or at night, more dangerous, bad prognosis, and usually 3 months.
|
|
|
If blood flow to heart does not get better in 6 hours...
|
Necrosis of heart tissue that can not be reversed
|
|
|
complications of AMI
|
-Arrhythmias
-Rupture of the Lt Ventricle wall -Aneurysm |
|
|
Arrthyhmia
|
-occur due to interruption of the blood supply to the pacemaker cells
-extremely common and major cause of mortality. |
|
|
Rupture of Lt Ventricular wall
|
-result from the necrotic heart tissue tearing
-hemorrhage occurs in the pericardial space -deadly and often occurs within the first 2 weeks after a MI. -survival rate low |
|
|
Aneurysm
|
-Late complication of Mi, 2 weeks to months after MI
-develops as the ventricular wall is weakend from clean up of tissue by phagocytic cells - localized outward bulge |
|
|
Treatments
|
-aspirin, to decrease clot formation
-beta-blockers, to reduce the work the heart has to do, decreasing demand for oxygen -nitroglycerin, to improve oxygen -morphine, calm the patient |
|
|
Thrombolytic therapy
|
reoxygenate the heart, break down throbus lodged in the artery by intravenous enzymes, TPA and Streptokinase. Given within the first 6 hours
|
|
|
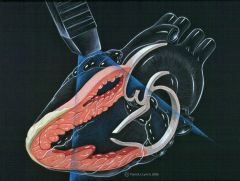
Primary coronary angioplasty
|
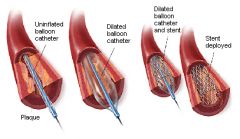
-improves coronary blood flow by enlarging the disease artery's lumen
-pressurized balloon is inflated in the vessel to open obstruction |
|
|
Define Stenosis
|
narrowing of the valvular opening, usually due to valvular tissue thickening that prevents it from opening properly
|
|
|
insufficiency and regurgitation mean the same thing.
T or F? |
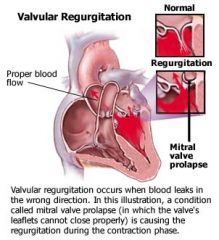
True: valvular incompetence that prevents complete valve closure, allowing blood to flow back up into previous chamber
|
|
|
Valvular Heart Disease affects how many valves?
|
one or all the valves
|
|
|
consequences of valvular heart disease are
|
- arrhythmias
- heart failure - pulmonary congestion - dyspnea (trouble breathing) - synocpe (fanting) |
|
|
Heart Failure
|
When heart is unable to pump blood forward at a rate to meet the body's metabolic demands or when the heart can only meet the demands if the filling pressure are abnormally high, or both.
|
|
|
Cardiac auscultation can reveal...
|
abnormal murmurs and or particular sounds indicative of valvular disease.
|
|
|
Mitral valve prolapse
|
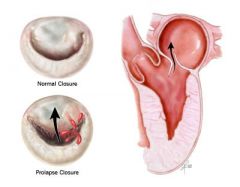
when the leaflet is floppy and enlarged and protrudes into the left atrium.
|
|
|
what is the major diagnostic tool for valvular heart disease
|
Echocardiography
|
|
|
Chest radiograph
|
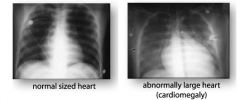
in which cardiac enlargement, valvular calcification and interstitial edema in the lungs can appear
|
|
|
treatment for valvular heart disease is
|
usually valve replacement
|
|
|
Acute Rheumatic Fever - ARF
|
-Inflammatory condition that involves the skin, heart, and connective tissues.
-significant cause of valvular lesions, in mostly developing countries, due to lack of antibiotics. -usually in childhood |
|
|
what is the bacteria that causes ARF?
|
Group A Streptococci, causing streptococcus pharyngitis (strep throat)
|
|
|
why is it important to get on antibiotics if you have strep throat?
|
Because 3% of people with strep will develop ARF 2-3 weeks after
|
|
|
what parts of the heart does ARF affect?
|
can affect all 3 layers of heart
valves become inflamed, and one or more valve can be permanently distorted and thickened. |
|
|
when do symptoms of valvular dysfunction from ARF occur?
|
may not be until 10-30 years after ARF
-40% develop mitral stenosis -25% develop aortic regurgitation or stenosis |
|
|
Mitral valve stenosis- MVS
|
Fibrous thickening of the valve leaflets, fusion of the commissures and leaflets calcification due to inflamation.
Photograph of a short-axis section from the base of the heart of a 44-year-old woman with rheumatic mitral stenosis shows diffuse fibrous leaflet thickening (arrow) and commissural fusion (arrowhead) that cause the valve to resemble a fish mouth. A large anteroseptal myocardial infarction with associated mural attenuation also is depicted. (Courtesy of William D. Edwards, MD, Department of Pathology, Mayo Clinic, Rochester, Minn.) |
|
|
What is MVS almost always caused by?
|
Acute Rheumatic Fever
|
|
|
when mitral valve becomes stiff and hard to push through Lt atrium and the pressure decreases. T or F ?
|
False: Increases pressure to push through the stenotic valve.
|
|
|
The increase pressure from MVS is transferred back to the lungs causing what?
|
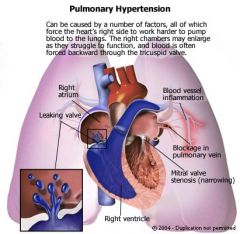
Pulmonary congestion, and after time Pulmonary Arteriolar Hypertension
|
|
|
Which side of the heart becomes hypertrophied (enlarged) due to MVS and pulmonary congestion?
|
Right side, because of lungs congestion, there is greater pressure to push against and right side then has to work harder.
|
|
|
MVS leads then to right- heart failure T or F ?
|
True, eventually right side gives up
|
|
|
Due to Right heart failure, what other conditions with the patient have?
|
-Liver congested and enlarged
-Ascites and edema in lower extremities -trouble breathing -reduced exercise capacity |
|
|
Mitral Regurgitation
|
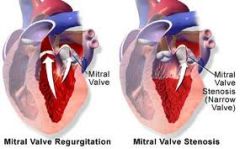
Leaflets of mitral valve do not close properly, back flow of blood into the left atrium.
|
|
|
Proper closure of mitral valve depends on what 3 structures?
|
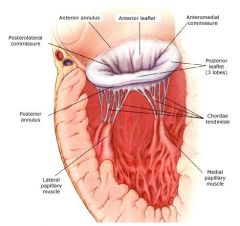
chordae tendineae, papillary muscles, and a tight mitral annulus (ring)
|
|
|
what causes the components of mitral valve to malfunction?
|
Acute myocardial infarct could damage papillary mucsle or ARF could calcify the annulus
|
|
|
because of blood regurgitation into the left atrium and the pressure due to extra volume, what happens to the left side of the heart?
|
Both the atrium and ventricle can become dilated to compensate for the greater stroke volume... eventually resulting to left ventricular failure.
|
|
|
Mitral Valve Prolapse - MVP
|
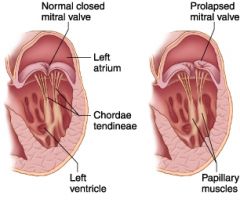
mitral valves flop into the left atrium during left ventricular systole (contraction)
mid-systolic click can be heard during auscultation Flippy floppy |
|
|
MVP affects what % of normal population?
|
About 7% and slightly more common in women
common and usually asymptomatic |
|
|
definitive diagnosis of MVP made with?
|

Echocardiography :)
|
|
|
MVP puts patients at more risk for?
|
infective endocarditis(one reason why people take prophylactic antibiotics), arrhythmias, and mitaral insufficiency
|
|
|
Aortic Stenosis
|
Calcified and harden aortic valve
|
|
|
What are the 3 pathways to aortic stenosis?
|
1.Rheumatic heart disease
2.Congenitally deformed valve (bicuspid): leads to abnormal blood flow, calcium deposits, and hardens valve. 3. Senile: wear and tear with old age |
|
|
most common cause of aortic stenosis?
|
Senile
|
|
|
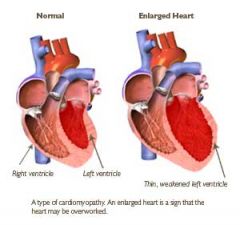
what happens to the Lt ventricle when it struggles against the stiff AO valve?
|
Hypertrophy of Lt ventricle, which leads to Lt ventricle becoming stiff as well
|
|
|
with AO valve stenosis the Lt ventricle works harder and then doesn't fill as easy because it is becoming stiff, what happens to the Lt Atrium?
|
Also becomes hypertrophied
|
|
|
Aortic Insufficiency (AI)
|

Occurs from abnormalities of the valve leaflets or dilation of the aortic root which stretches leaflets and prevents form closing tightly, creating backflow to Lt ventricle during diastole
|
|
|
Acute AI
|
left ventricle can't handle increasing volume and high pressure goes to left artrium and pulmonary tree.
|
|
|
Acute AI results in...
|
Severe Dyspnea (difficultly breathing) , and usually is a surgical emergency
|
|
|
Chronic AI
|
Left ventricle compensates by dilation and hypertrophy
can last many years with out problems, but eventually will need intervention to prevent heart failure. |
|
|
Infectious Ednocarditis (IE)
|
-One of the most serious infections
-acute and chronic types -colonization and invasion of heart valves by bacteria |
|
|
what does IE look like?
|
Vegetation of bacteria on heart valves
|
|
|
What is the best way to diagnose IE
|

Ultrasound and Blood work
|
|
|
IE is life threatening and results in death up to 60%. T or F?
|
True
|
|
|
Why is IE so deadly?
|
The bacteria grow and erode valve surface, exposing underlying collagen. Platelets bind to the damage and envelop the organisms into a vegetation. Which then protects the organisms from antibodies and antibiotics.
|
|
|
Acute IE
|
-organisms with high virulence ( high ability to cause disease) enter the blood stream and circulate the heart valves.(such as Staphylococcus aureus)
-Causing scaring, valve proforation, perivalvular abcesses -life threatening and aggressive medical treatment needed. |
|
|
major risk factor for Acute IE?
|
IV drug abusers
|
|
|
Acute IE vegetations occur mostly where?
|
Tricuspid and pulmonic valves
|
|
|
Chronic IE
|
-Low virulence organisms get into blood stream
-require previously damaged valve to attach -rheumatic heart disease -MVP -prosthetic heart valves |
|
|
what should patients with increase of IE take ?
|
Prophylactic Antibiotics
|
|
|
Chronic IE is a slower progressing disease and more likely to kill the patient. T or F ?
|
False: least likely to kill them
|
|
|
Both chronic and acute IE are dangerous because?
|
vegetation can break off and embolize to other organs, causeing ishecmic damage.
|
|
|
most common organs affect by vegetation embolus
|
Lungs, Brain, Spleen, Kidneys
|
|
|
IE treatment of choice?
|
Valve replacement
|

