![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
55 Cards in this Set
- Front
- Back
|
What rate does the SA node fire at if there is no influence from the ANS? |
90-100 beats per minute. |
|
|
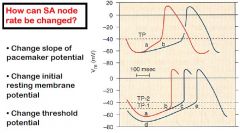
What two mechanisms can the ANS use to change the rate of the SA node? |
|
|
|
What is the mechanism that increases the conduction of the SA node by the SNS (neurotransmitters and receptors)? |
When Norepi or epi bind to Beta 1 receptors (G coupled protein) second messangers transmit signal ultimately increasing influx of Na & Ca into cells causing depolarization. |
|
|
What is the mechanism that decreases the conduction of the SA node by the PNS (neurotransmitters and receptors)?
|
When Acetylcholine binds to muscarinic receptors (G coupled Protein) on the pacemaker cells triggers the opening of chemically gated K+ ion channels triggering the outward flow causing the membrane to hyperpolarize. The slope of depolarization also decreases. |
|
|
Does the SNS or PNS affect a more rapid change in HR and why? |
The PNS- The second messanger system for the PNS is shorter and faster (activates faster), and the deactivation is caused by the breakdown of acetylcholine by plasma cholinesterase. SNS requires re-uptake of norepi. Beta receptors use cAMP which has multiple steps. |
|
|
What happens when you give atropine to a heart transplant patient? |
Nothing, the transplanted heart does not have parasympathetic innervation. |
|
|
What happens if you give atropine to a patient with a heart rate of 110 beats per minute? |
Nothing, there is no PNS stimulation when HR is above 100. |
|
|
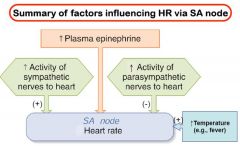
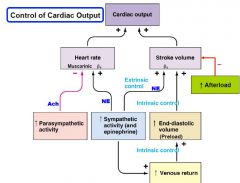
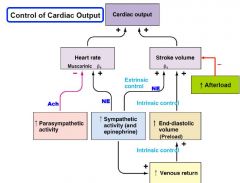
What are the factors that can affect HR via the SA node? |
|
|
|
What controls the ANS stimulation of the heart? |
The ANS receives input from the Cardiovascular Control Center (in the Medula). |
|
|
Where does the Cardiovascular Control center receive input from? |
-Nuclei of the hypothalamus(emotional, thermoregulation) -Baroreceptors -Atrial stretch receptors -Other Parts of the Brain |
|
|
What is the Bainbridge Reflex? |
Atrial stretch receptors send impulse to the CV Control center with an increase in venous return stimulating an increase in the HR. (example is with respiration) Is most apparent with slower heart rates. |
|
|
How does the Bainbridge reflex work regarding the PNS (Vagus nerve stimulation) with respiration? |
WIth inspiration (more negative chest cavity) increases venous return leads to decreased vagal activity (increased HR) WIth expiration (more positive chest cavity) decreased venous return leads to increased vagal activity (decreased HR) |
|
|
What are the two mechanisms the heart has to increase the force of contraction ( thus SV)? |
Frank-Starling Mechanism (preload gives more stretch to line-up crossbridge sites) Increase Contractility via Sympathetic stimulation (more Ca++ to activate crossbridges) |
|
|
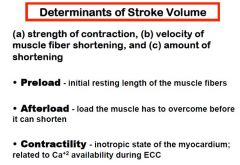
What are the three determinants of stroke volume? |
|
|
|
|
|
|
What determines the preload of the heart? |
The End Diastolic Volume. |
|
|
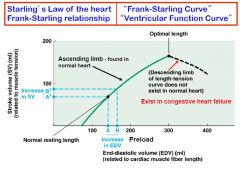
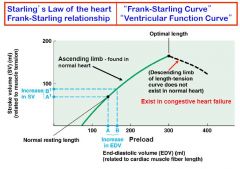
What does the Frank-Starling relationship say? |
Over a wide range of preloads the ventricles will respond to increased preload by increasing its force of contraction generating a greater SV. |
|
|
Why does the health heart never reach the descending portion of the Frank-Starling Curve (three reasons)? |
The normal heart will automatically increase SV whenever venous return increases. Cardiac muscle is stiffer than Skeletal muscle (more resistant to overstretch) Pericardium resists acute overfilling. |
|
|
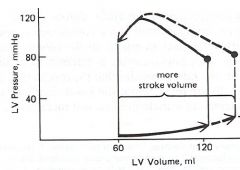
Increased Preload Pressure Volume Curve |
|
|
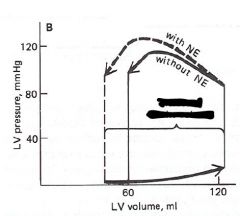
Increased Contractility Pressure Volume Curve |
|
|
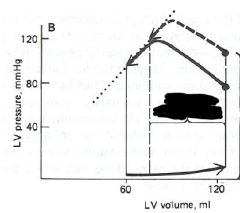
Increased Afterload Pressure Volume Curve |
|
|
Why is contraction of the cardiac muscle not maximal when there is no sympathetic stimulation? |
Without the SNS there is not enough Ca++ to activate all the crossbridge binding sites during Excitation-Coupling Contraction (ECC). |
|
|
How does SNS stimulate stronger contractions? |
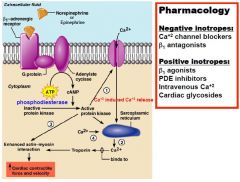
|
|
|
What is protein Kinase? |
PK is an intracellular enzyme that phosphorylates one or more intracellular proteins, changing their activity. |
|
|
How do Phosphodiesterase Inhibitors (PDEs) increase contractility? |
Terminate cAMP activity preventing the activation of Protein Kinase which increases the reabsorption of Ca++ into the SR. |
|
|
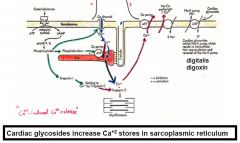
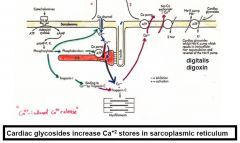
How do Cardiac Glycosides increase contractility? |
They decrease the activity of the Na+/K+ pump increasing Intracellular Na+ levels. This impares the secondary active transport of Ca++ out of the cell in exchange for Na+ The extra intracellular Ca++ is then absorbed into the Sarcoplasmic Reticulum. |
|
|
|
|
|
Do Beta 1 Blockers affect contractility at rest? |
Not much, Beta 1 blockers affect on contractility is a function of how much sympathetic stimulus there is to block and at rest there is not much SNS stimulation. |
|
|
What would happen to the position of the Ventricular Function Curve (Frank-starling Curve) if a Ca++ channel blocker is given? |
At any given preload there would be a weaker contraction, SV would go down The curve would shift down and to the right |
|
|
What happens to the VFC with sympathetic stimulation? |
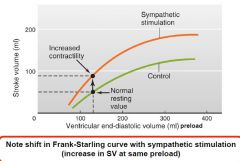
|
|
|
What is afterload? |
The amount of pressure the Ventricles must overcome before they can push open the semilunar valves & eject blood. |
|
|
What happens to the isometric phase of contraction as afterload increases? |
It becomes longer as well. |
|
|
|
|
|
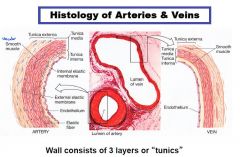
Describe the Histology of arteries and veins. |
|
|
|
What type of innervation do vascular smooth muscle (VSM) receive? |
Most receive only SNS stimulation, relatively few VSM receive dual innervation. |
|
|
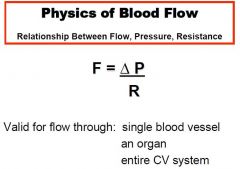
What is the formula for flow? |
|
|
|
What three factors affect resistance to flow and which is the most important? |
Viscosity of blood-Hematocrit Vessel length Radius of the vessel-Greatest effect R=1/r to the Fourth power |
|
|
What is Vascular Compliance? |
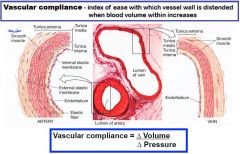
|
|
|
How does SNS affect vascular compliance? |
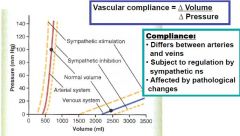
|
|
|
How is total blood volume (TBV) distributed at rest? |
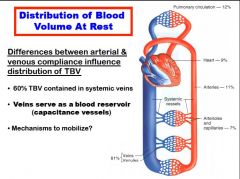
|
|
|
Which part of the vascular system offers the largest pressure drop? |
Arterioles, they are the main contributor to SVR. |
|
|
How does the vascular system optimize gas exchange in the capillaries? |
They have the largest cross-sectional area which causes the blood to have the slowest velocity allowing more time for gas exchange. |
|
|
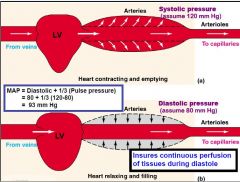
What are the two primary functions of the systemic arteries? |
Provide rapid transit, low resistance passageway from the heart to the tissue Serve as a pressure reservoirs to ensure continuous perfusion throughout the cardiac cycle. |
|
|
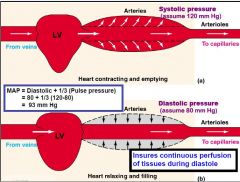
|
|
|
Why not just average systolic and diastolic pressures when calculating MAP instead of the formula? MAP= DBP+1/3(SBP-DBP) |
More time is spent in diastole than systole. |
|
|
Where does the arteries branch into arterioles? |
within an organ. |
|
|
What is the function of arterioles? |
to function as a stopcock, regulating tissue blood flow and also SVR. |
|
|
What are some chemicals that affect arteriole smooth muscle? |
Norepinephrine Epinephrine Vasopressin Angiotensin II
Nitric Oxide and ANP |
|
|
What controls Arteriolar smooth muscle? |
1. Local metabolic factors to match blood flow to metabolic needs (produces vasodilation) 2. Extrinsic Factors-SNS and hormones (Mostly Vasoconstriction) 3. Inflammatory/tissue damage factors (mostly Vasodilators) |
|
|
What is active Hyperemia? |
Increased blood flow related to metabolic needs. Allows the tissue to auto-regulate blood flow according to needs |
|
|
What local metabolic ISF levels would cause vasodilation? |
Decreased Oxygen Increased Carbon Dioxide Increased Hydrogen ions Increased Potassium Increased Osmolarity Increased Adenosine Increased Temperature |
|
|
What is pressure/flow auto-regulation? |
With an increased perfusion pressure there is a big increase in flow (independent of metabolic changes) Eventually flow decreases back to control value Believed to be a myogenic response (passive stretch) |
|
|
What factors affect Extrinsic Control of arteriolar radius? |
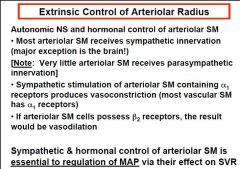
|
|
|
When local factors are conflicting with sympathetic or hormonal factors which one has a greater effect? |
Coronary and skeletal muscle vessels- local overrides extrinsic Everywhere else-Extrinsic overrides local |
|
|
Where do the preganglionic sympathetic neurons originate from? |
Lateral horn of the spinal cord gray matter from T1-upper lumbar segments. Inputs to the CV control center come from the cortex, thermoregulatory center of the hypothalamus, and baroreceptors. |

