![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
47 Cards in this Set
- Front
- Back
|
normal PR interval
|
3-5 small box (120-200 msec)
|
|
|
normal QRS
|
2-3 small box (80-120 msec)
|
|
|
normal QTc
|
9-11 small box (360-440 msec)
|
|
|
1 mm (small box) = ?
|
0.04 sec or 40 msec
|
|
|
to check p-wave, look at lead ___.
|
II (mainly), III, aVF
|
|
|
normal PR interval
|
3-5 small box (120-200 msec)
|
|
|
normal QRS
|
2-3 small box (80-120 msec)
|
|
|
normal QTc
|
9-11 small box (360-440 msec)
|
|
|
1 mm (small box) = ?
|
0.04 sec or 40 msec
|
|
|
to check p-wave, look at lead ___.
|
II (mainly), III, aVF
|
|
|
atrial fibrillation will show up as what ekg?
|
no p-wave with QRS complex irregular spacing (this is most common arrhythmia)
|
|
|
what's the HR jingle that Dubin taught you?
|
300, 150, 100...75, 60, 50 (from thick line to thick line)
|
|
|
bifid or notched p-wave in lead II shows ____ ____ _________.
|
left atrial enlargement.
|
|
|
what will you look for in right atrial enlargement?
|
tall p wave > 2.5 mm (small boxes) in lead II
|
|
|
what would you look for on ekg:
- left atrial enlargment - right atrial enlargement - AV block |
- bifid P in lead II
- tall P wave > 2.5 - prolonged PR interval (> 5 boxes or 0.20 sec) |
|
|
name some reversible causes of P-R prolongation (AV node block)
|
-drugs (beta blockers, ca channel blockers, digoxin)
-acute ischemia or infarction |
|
|
what is an irreversible cause of PR prolongation?
|
degenerative or calcific dz of the conduction system (Lev's dz)
|
|
|
name the triad caused on the ekg by wolff-parkinson-white (WPW)
|
short PR (<120 msec)
wide QRS (>3 blocks) delta wave (slurring at initial rise of R wave) |
|
|
what does delta wave ALWAYS mean?
|
that the conduction is anterograde depolarization down the accessory pathway, bypassing the AV node (this is less common - 20% - and is more dangerous)
|
|
|
what happens to QRS complex in BBB?
also, differentiate b/w RBBB and LBBB |
ventricle with BBB is depolarized late, so that you have an R(prime) for the later ventricle
you'll have: - wider QRS (3+ boxes) - for RBBB: look in V1 and V2 for "rabbit ears" - for LBBB: look in V5 and V6 (not rabbit ears) |
|
|
causes of BBB
|
- ischemia/infarct of BB
- eccentric hypertrophy of that ventricle (will take longer to depolarize causing wider QRS and RSR') |
|
|
most common congenital dz presenting in adulthood
|
ASD (atrial septal defect) = shows up as R BBB/R eccentric hypertrophy (blood shunts from left to right atrium, filling RV with more blood)
|
|
|
what is the normal QTc? how do you calculate it?
|
360-440 msec
QT divided by square root of R-R interval |
|
|
complication of long QT interval
|
Torsades de Pointes (poly morphic ventricular tachycardia)
|
|
|
causes of prolonged QT interval
|
- drugs (anti-arrythmics, anti-psychotics, TCAs)
- electrolyte abnormalites (low K, low Mg or low Ca) |
|
|
what is the most common electrolyte abnormality leading to prolonged QT interval?
|
low K
|
|
|
name the drugs that prolong PR (block AV node)
|
beta blockers, Ca channel blockers, digoxin, amiodarone, clonidine
|
|
|
what do you look for on an ekg if it's volume overload (eccentric hypertrophy)?
|
LBBB or RBBB
|
|
|
what do you look for on an ekg if it's pressure overload (concentric hypertrophy)?
|
RVH, LVH
|
|
|
what is the voltage criteria for LVH and RVH?
|
LVH: R (V5 or V6) + S (V1 or V2) > 35 mm
RVH: Tall R > 5 mm or R>S in V1 or V2 |
|
|
what's the axis criteria for LVH and RVH?
|
LAD in LVH and RAD in RVH: “Overall QRS axis shifts to the hypertrophied ventricle”
|
|
|
name the 11 steps in ekg reading
|
-rhythm
-rate -P wave morphology -QRS axis -PR interval -QRS interval -QT interval -Chamber enlargement: LVH, RVH -pathologic Q waves -ST and T wave changes -Precordial R wave progression |
|
|
What are the 3 criteria for pathologic Q waves?
|
1. negative initial QRS
2. WIDER than 0.04 sec (40 msec) - one small box 3. deeper than 1/3 of subsequent R wave in same QRS |
|
|
what are the 3 hallmarks of an evolving MI?
|
pathologic Q wave
ST elevation inverted T waves |
|
|
1)ST elevation =
2)ST elevation AND path Q waves = 3)path Q waves ONLY = |
acute MI
evolving MI old MI |
|
|
ST depression signals _____ ____.
ST elevation signals _____. |
1) subendocardial ischemia (this is the first part to have ischemia - since it's in the area that's farthest from coronary arteries) --> you'll see this before elevation
2) acute MI |
|
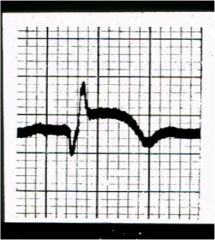
what are the 3 things you see wrong in this ekg?
|
pathologic Q waves
ST elevation inverted T waves this is an evolving MI!! |
|
|
The ST segment depression that is most characteristic of ischemia is:
a. downsloping b. upsloping c. horizontal d. A and C |
D. downsloping and horizontal
upsloping ST segment depression can occur in nl person during stress test |
|
|
The most life-threatening cause of ST segment elevation is:
a. Acute Myocardial Infarction b. Acute Pericarditis c. Coronary vasospasm (Prinzmetal’s angina) d. Early Repolarization |
a. AMI
|
|
|
differentiate acute MI vs. pericarditis in terms of 1) ekg lead, 2) presence of pathologic Q waves, 3) PR morphology
|
acute MI = localized ST elevation (think only one artery/branch involved), path Q wave, NO PR depression
acute pericarditis = diffuse ST elevation, no path Q waves, depressed PR |
|
|
what are the 3 things ST elevation could be?
|
-AMI
-pericarditis -coronary vasospasm (Prinzmetal's angina) |
|
|
if you see tall ST segment elevations in leads I, aVL and V2-V6, dx?
|
massive acute MI
|
|
|
three things to spot for evolving MI
|
pathologic Q wave
ST elevation inverted T wave |
|
|
what can a peaked/tall T wave (>10mm) mean?
|
high potassium (mainly!)
AMI ischemia |
|
|
what if you only see ST elevation?
|
acute MI!!
|
|
|
what could a tall R in V1/V2 indicate (precordial R wave progression)?
|
old posterior MI
RVH RBBB WPW |
|
|
by itself, what are pathologic Q waves indicative of?
|
an old myocardial infarction
|

