![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
84 Cards in this Set
- Front
- Back
|
pediatric with holosystolic mumur LL sternal border and rumbling diastolic murmur or cardiac apex. Sx: failure to thrive, easy fatigability and and heart failure. Think? Dx how?
|
most common congenital heart malformation. ventricular septal defect with left to right shunt. Diastolic murmur is due to increased flow across the mitral valve
* echocardiogram with bubble study |
|
|
most common congenital heart malformation.
|
ventricular septal defect
|
|
|
atrial fibrillation. How do you choose anti coag choice
|
CHADS2:
* CHF * HTN *Age >75 *DM *stroke = 2 pts 0pts -> aspirin >3pts->warfarin 1-2 - either is ok |
|
|
pt with arrythmia on long term amiodarone treatment presenting chronic interstitial pneumonitis (nonproductive cough, fever, pleuritic chest pain, weight loss, dyspnea on exerticion and focal or diffuse intersitial opacity on CXR, organizing pneumonia, ARDS, or solitary pulmonary mass. Dx? tx?
|
amiodarone toxicity
- stop amiodarone |
|
|
palpitations w/ regular, Narrow QRS, tachycardia (150-200). Think? Dx how?
1. tx if unstable? 2. tx stable 1st line? 3. ***if this fails? 4. best long term management? |
supraventricular tachycardia (SVT)
dx: EKG, holter monitor 1. tx if unstable: synchronized cardioversion 2. incrase vagal tone 3. IV adenosine. Both allow the rhythm to slow so that it can be recognized. 4. radiofrequency ablation |
|
|
recurrence of chest pain 1-4 days after MI, which gets worse with position changes and deep inspiration. Pericardial friction rub (scratchy sound that is more pronounced when the patient leans over). EKG: sinus tach, diffus ST segment elevations with PR segment depressions "q waves)" Think? Dx how? tx?
|
infarction paricarditis
- clinical - high dose aspirin as it manages the pain . Other NSAIDs may increase the risk of myocaridial rupture after transmural MI |
|
|
depressed pt with hypotension, anticholinergic effects, change in mental status, EKG with widened QRS and sinus tachy. Think? Tx
|
TCA overdose and TCA induced ventricular arrhythmia
- 1. sodium bicard counters the TCA cardio toxic effect. 2. lidocaine is the best drug for TCA ventricular arrhythmias |
|
|
cardiotoxic chemo agents like doxorubicin. How monitor
|
radionuclide vetriculography
|
|
|
smoking cessation: buproprion or nicotine
|
nicotine
nicotine patch is preferred to buproprion in the early statges of nicotine cessations |
|

|
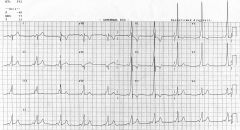
Afib
|
|

|
atrial flutter
*slow down with cardizem and call cards |
|

|
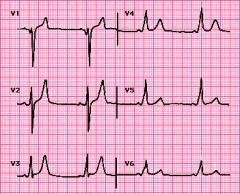
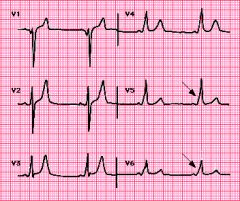
![left bundle branch block
The QRS duration must be ≥ 120 ms[2]
There should be a QS or rS complex in lead V1
There should be a RsR' wave in lead V6.](https://images.cram.com/images/upload-flashcards/50/84/54/2508454_m.png)
left bundle branch block
The QRS duration must be ≥ 120 ms[2] There should be a QS or rS complex in lead V1 There should be a RsR' wave in lead V6. |
|
|
cocaine induced myocardial ischemia. Tx?
|
benzo for sedation and nitro and calcium channel blockers for pain relief
* beta blockers: avoid due to unopposed alpha stimulation |
|
It worsens after dilt or digoxin.
1. dx? 2. sequelae? 3. best initial tx? 4. best long term therapy |
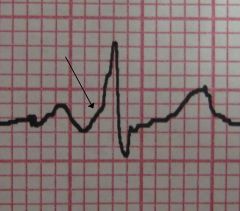
1. wolf parkinson white syndrome
- caused by an accessory pathway that connects atria to ventricles bypassing the av node - has a short PR interval with a DELTA wave (P-R gradual up slope before the spike), and a wide >0.12s QRS complex 2. can deveolop tachyarrhythmias 3. procainamide 4. catherter ablation if they have symptomatic arrhythmias or |
|
|
patient with 3 vessel disease or left main disease. Tx
|
CABG
|
|
|
what drugs do they use for a pharmacologic stress test?
|
adenosine myocardial perfusion imaging
|
|
|
bradycardia in anterior wall MI. Tx symptomatic? asymptomatic
|
if symptomatic: IV atropine sulfate
if asymp: no tx, usually transient |
|
|
artery that supplies the lateral wall of left ventricle
|
left circufelx
|
|
|
artery that supplies the right ventricle and infereoposterior wall of left ventricle
|
right coronary
|
|
|
artery that supplies the left ventricle anterior wall
|
left anterior descending
|
|
|
comorbidity that is the single poorest predictor of future CV outcomes
|
DM
|
|
|
cocaine induced transmural MI not improved with drugs. Next step
|
coronary angiography to look for coronary thrombus
|
|
|
on digoxin and has nausea, vomiting, anorexia, fatigue, confusion, visual disturbances, and cardiac problems. ? antiarrythmic Drugs responsible
|
dig toxicity:
amiodarone verapamil quinadine |
|

P waves of different morphology and tachycardia, variable RR and PR segments. Think? Caused by?
|
multifocal atrial tachycardia:
1. hypoxia 2. COPD … check arterial blood gas |
|
|
hemoptysis with low pitched rumbling diastolic murmur, with prominent pulmonary arteries at the hilum, elevation of the left mainstem bronchus, left arterial enlargement with flattening of the left heart border
|
mitral stenosis usually 2/2 rhumatic fever
|
|
|
AAA what's more important, better control of DM or smoking cessation?
|
smoking cessation
|
|
|
code: fast and wide, regular w/ pulse. Dx? tx
|
V-tach
- Amiodarone 150mg IV |
|
|
code: fast and wide, regular w/ no pulse. Dx? tx
|
pulseless V-tach
shock CPR |
|
|
fast and wide, irregular w/o pulse. Dx? tx
|
V-fib
shock CPR |
|
|
fast and narrow w/o pulse
|
PEA
CPR |
|
|
code: no waveform
|
asystole
|
|
|
EKG: sinus brady. what next?
|
check leads II and V1 for P waves
* medication likely cuase tx: non-symptomatic -> bening - if elderly w/ enlarged ventricles, investigate further |
|

px w/ palpitations, syncope, chest pain, or sudden death.
1. dx 2. hemodynamically stable tx? 3. hemodynamically UNstable tx? |
1. Vtach
2. stabilize with lidocaine, amiodarone, procainamide, or mag 3. Synchornized cardioversion (premedicate with benzo) |
|

|
Vtach
* stabilize with lidocaine * premedicate with benzo * Synchornized cardioversion |
|
|
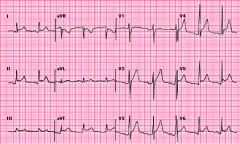
pericarditis
Electrocardiogram in acute pericarditis showing diffuse upsloping ST segment elevations seen best here in leads II, III, aVF, and V3 to V6. There is also subtle PR segment deviation (positive in aVR, negative in most other leads). ST segment elevation is due to a ventricular current of injury associated with epicardial inflammation; similarly, the PR segment changes are due to an atrial current of injury which, in pericarditis, typically displaces the PR segment upward in lead aVR and downward in most other leads. |
|

|
Electrocardiogram in typical complete LBBB. The asynchronous activation of the two ventricles increases the QRS duration (0.14 sec). The abnormal initial vector results in loss of normal septal forces as manifested by absence of physiologic q waves in leads I, aVL, and V6. The late activation of the left ventricle prolongs the dominant leftward progression of the middle and later depolarization forces, leading to a positive and widened R wave in the lateral leads. Both the ST segment and T wave vectors are opposite in direction from the QRS, a "secondary" repolarization abnormality.
|
|

what electrolyte abnormality?
|
Prolonged QT interval due to hypocalcemia
The QT interval in this case is quite prolonged (0.50 sec) at a heart rate of 55 beats/min. The rate corrected QT (QTc) interval can be calculated from: QT interval ÷ sqrt (RR interval). The RR interval is 1.05 sec leading to a QTc of 0.48 sec which is longer than the normal value of ≤0.44 sec. A long QT interval with a "stretched out" ST segment and normal T wave is most consistent with hypocalcemia. In contrast, hypercalcemia shortens the QT, hyponatremia usually has no effect on the ECG, and hypokalemia prolongs repolarization with flattened or broad T waves and prominent U waves. |
|
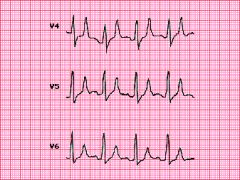
What is the cause of the wide QRS complex?
|
Wolff-Parkinson-White pattern
Precordial leads in a patient with preexcitation due to the WPW syndrome. The three characteristic findings are the short PR interval (0.09 sec in this case), the wide QRS, and the delta wave (slurring of the QRS upstroke) that is best seen in leads V5 and V6 (arrows). |
|

chronic lung disease
|
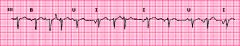
Multifocal atrial tachycardia
* Electrocardiogram showing multifocal atrial tachycardia in a woman with severe pulmonary disease. The diagnostic criteria include an average atrial rate above 100 beats/min and at least three different consecutive non-sinus P waves in the same lead. Note the multiple P wave morphologies - inverted (I), upright (U), and biphasic (B) |
|
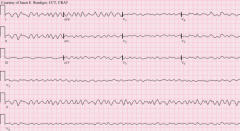
electrolyte abnormalities
|
hyperkalemia
Lateral precordial leads showing peaked, narrow (tented) T waves and prolongation of the QRS complex (0.14 to 0.16 seconds) associated with moderate to severe hyperkalemia. |
|

|

Atrial flutter with 2:1 block
Typical atrial flutter with 2:1 atrioventricular block. The flutter rate is approximately 300/min with a ventricular rate of 150/min. The flutter waves are best seen in leads II, III, and V1 (arrows). This patient also has low QRS voltage in the limb leads, a non-specific finding. |
|

|
Hypercalcemia
Shortened QT interval in hypercalcemia that results from shortening of the duration of the ventricular action potential. (Hypocalcemia has the opposite effect.) Note how the T waves appear to take off directly from the end of the QRS due to abbreviation of the ST segment. The slight J point elevation in leads V1 to V3 may also be seen with hypercalcemia in the absence of ischemia. |
|

hx of syncope
|
Sick sinus syndrome and atrial fibrillation
Rhythm strip showing sick sinus syndrome. The initial part of the tracing reveals coarse fibrillation with a slow ventricular response in the absence of drugs that slow AV nodal conduction. The atrial fibrillation breaks and is followed by a sinus escape beat with a long escape inverval of nearly four seconds and then another escape beat at a similar interval (not shown). |
|
|
pt has an MI. what do your order a few days latter if he has new chest pain?
|
CK-MB. Troponins will stay elevated for a couple of weeks.
|
|
|
Which cardiac enzyme rises first?
|
myoglobin rises in 1-4 hours. Troponins rise in 3-6 hours
|
|
|
ACS initial tx. What reduces mortality? if acute MI?
|
1. ASA - reduces mortality
2. morphine and nitrates do not reduce mortality 3. O2 if hypoxic 4. clopidogrel (plavix) or prasugrel if acute MI |
|
|
STEMI. What reduces mortality? <90min? >90min>
|
1. thrombolytics if >90 min
2. primary angioplasty (a type of percutaneous coronary intervention) - perform w/in 90 minutes benefit decreases as time increases |
|
|
stable angina tx
|
asa, beta blocker, and statin
angioplasty does not improve mortality beyond this |
|
|
ACS tx after initial tx? decrease mortality and under what conditions?
|
1. beta blockers decrease mortality and are not time sensitive
2. ACE I/ARB. Lower mortality ONLY IF left ventricular dysfunction or systolic dysfunction 3. Statin if LDL >100. Lower mortality |
|
|
post MI discharge meds
|
ASA
clopidogrel metoprolol, carvedilol, or bisoprolol statin, ACEI/ARB |
|
|
How does NSTEMI management differ from STEMI? Coagulation?
|
No thrombolytic use
- LMWH - lowers mortality - Glycoprotein IIb/IIIa inhibitors lower mortalitiy - PCI also used |
|
|
stable angina tx
|
- ASA and metoprolol lower mortality
- nitrates - do not lower mortality - coronary angiography to see if they are a CABG candidate |
|
|
what vessel should be used for CABG
|
internal mammary artery remains open for 10 years
saphenous vein remains open for 5 years |
|
|
indications for CABG: number of vessels? % stenosis
|
-3 vessel dz and >70% stenosis
OR left MAIN coronary w/ >70% stenosis |
|
|
LDL goal for pt w/ CAD and DM
|
<70
|
|
|
MI risk factors: BP, cholesterol, fam hx, age
|
- tobacco
- HDL<40 - primary fam hx of CAD F<65 or M<55 - age: M>=45 and F>=55 |
|
|
60F w/ acute severe dyspnea, rales, S3 gallop, and orthopnea. dx? tx? work up?
|
- CHF w/ acute pulmonary edema
- tx w/ O2, furosemide, nitrates, morphine - CXR, EKG, oximeter, echo - admit to ICU |
|
|
pulmonary edema; gave O2, furosemide, nitrates, morphine. Now pt still dyspneic. tx?
|
positive ionotrope: dobutamine,
2nd line: amirone, milrinone |
|
|
rales
|
crackles
|
|
|
Rhonchi
|
coarse rattling sound somewhat like snoring, usually caused by secretion in bronchial airways
|
|
|
pulm edema w/ vtach, afib, a flutter, or SVT. tx?
|
synchronized cardioversion
|
|
|
what does a normal BNP mean?
|
CHF is ruled out
|
|
|
Digoxin benefits for CHF
|
- decreases symptoms if EF reduced as has inotropic effects
- decreases frequency of hospitalizations - DOES NOT decrease mortality |
|
|
Which bb have been shown to reduce mortality for CHF?
|
carvedilol and metoprolol
|
|
|
systolic CHF - what medications? which ones lower mortality?
|
1. ACEI/ARB - lower mortality
2. metoprolol or carvedilol: lower mortality 3. Spironolactone - use if px EF<35%. lower mortality 4. digoxin if symptomatic - lower symptoms and hospitalizations. 5. diuretics - do not lower mortality |
|
|
diastolic CHF tx? which ones should not be used
|
BB and lasix (or other diuretics)
ACE I - unsure if it helps Digoxin and spironolactone do NOT help |
|
|
Most common cause of death in CHF? What can you do to prevent this?
|
* sudden death from arrhythmia
* ACEI, BB, spironolactone. * if EF<35% -> cardioverter/defibulator |
|
|
which mumurs increase with inspiration? expiration?
|
R
Inspiration g H T L Expiration F T |
|
|
which murmurs increase w/ valsalva
|
HOCM, and MVP
|
|
|
2nd RUS border systolic crescendo decrescendo murmur
|
aortic stenosis
|
|
|
2nd LUS border systolic murmur
|
pulmonic valve
|
|
|
LLS border systolic murmur
|
aortic regurg
tricuspid murmur VSD |
|
|
murmur workup
|
1. echo (TTE. if not diagnostic, then order TEE), ecg, and CXR
- left heart catheterization is most accurate |
|
|
valsalva effect on heart
|
decreases preload
|
|
|
handgrip effect on heart
|
increases afterload
|
|
|
ACEI effect on heart?
|
decreases afterload
|
|
|
tx of regurg lesions (handgrip makes it worse; amyl nitrate improves it)
|
1. vasodilator therapy (ACEI/ARB or nifedipine) - It decreases afterload which decreases regurgitation.
2. if regurg progresses -> valve replacement |
|
|
diastolic murmurs are most commonly?
|
aortic regurg or mitral stenosis
|
|
|
stenotic valvular lesion tx
|
anatomic repair
- mitral ballon valvuloplasty - aortic stenosis: valve replacement |
|
|
diuretic effects on heart
|
decrease preload
|
|
|
murmur w/ valvular disease; valsalva improves murmur. tx
|
diuretic as it decreases preload
|
|
|
murmur w/ valvular disease: amyl nitrate improves murmur or hand grip makes it worse
|
ACE I
|
|
no pulse
1. dx? 2. tx? |
1. v-fib
2. UNsynchronized cardioversion |
|
|
syncope w/ sudden loss of consciousness. etiology (2)
|
neurologic (seizures)
cardiac etiology? |

