![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Cardiac Electrical Conduction |
Deals with the electrical impulses of the heart that make it move |
Pathway |
|
|
Cardiac Waves |
P Wave PR Interval QRS Complex T Wave QT Interval ST Segment |
Atrial and Ventricular |
|
|
P Wave represents |
Atrial Depolarization |
SA Node firing. |
|
|
PR Interval measurement |
0.12-0.20 seconds |
Normal PR Interval |
|
|
QRS Represents |
Ventricular Depolarization |
Contracting |
|
|
QRS Complex Measurement |
0.12 or less |
Normal QRS Complex |
|
|
T Wave Represents |
Ventricular Repolarization |
Resting |
|
|
QT Interval |
Prolonged= risk for V-Tach or V-Fib. Should be less than 1/2 the R-R time |
|
|
|
ST Segment |
Elevated > 1mm is significant for ischemia or infarct Depressed is significant for ischemia, hypokalemia, or dig toxicity. |
An ST elevated MI is indicative of cardiac cell death |
|
|
Two Stage of Repolarization (Resting) |
Absolute Refractory Period Relative Refractory Period |
|
|
|
Absolute Refractory Period |
Cardiac cells are unable to respond to new electrical stimulus and can not spontaneously depolarize |
Beginning of QRS Complex to middle of the T Wave |
|
|
Relative Refractory Period |
Repolarization is almost complete, and cardiac cells can be stimulated to contract prematurely if stimulus is stronger than normal |
Middle of T Wave until the end of the T Wave |
|
|
Three Major Electrolytes Affecting Cardiac Function |
Potassium K+ Sodium Na+ Calcium Ca+ |
|
|
|
How Potassium Affects Cardiac Function |
Performs major function in cardiac depolarization and repolarization. Without it, the heart can not function |
|
|
|
How Sodium Affects Cardiac Function |
Performs a vital part in depolarization of the myocardium |
|
|
|
How Calcium affects Cardiac Function |
Important function in depolarization and myocardial contraction Pump and power of the heart |
Without Calcium your muscles don't contract |
|
|
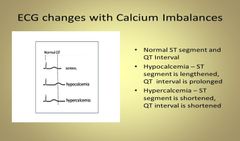
Hypocalcemia And EKG Changes |
Causes Prolonged ST and QT Intervals |
|
|
|
Hypercalcemia and EKG Changes |
Shortened ST Segment with Widened T Wave |
|
|
|
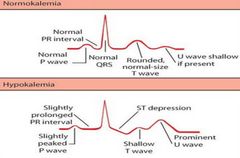
Hypokalemia and EKG Changes |
ST depression with shallow, flat, and inverted T Waves and Prominent U Waves. Indicative of Dialysis, Diuretic Use, or Dehydration |
|
|
|
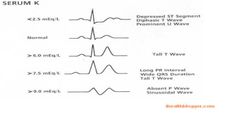
Hyperkalemia and EKG Changes |
Tall peaked T Waves with flat P Waves, Widened QRS Complex, and Prolonged PR Intervals Indicative of Renal Failure Caused by too much Potassium intake |
|
|
|
SA Node Rate of Conduction |
60-100bpm |
|
|
|
AV Junction Rate of Conduction |
40-60bpm |
|
|
|
Ventricles Rate of Conduction |
20-40bpm Patient will need to be paced due to low Cardiac Output |
|
|
|
Normal Sinus Rhythm |
Implies normal sequence of conduction, originating in the sinus node and proceeding to the ventricles via the AV Node and HIS-Purkinje System. |
|
|
|
Normal Sinus Rhythm EKG Characteristics |
-Regular, Narrow-complex rhythm with a rate of 60-100bpm -Each QRS Complex is proceeded by a P Wave -P Wave is upright in lead II and down going into lead aVR |
|
|
|
Sinus Arrhythmia EKG Characteristics |
-Heart is not in total rhythm -Variations in the cycle lengths between P Waves and QRS Complexes -Will often sound irregular on exam -Normal P Waves, PR Interval, and narrowed QRS Complexes -Usually Respiratory- Increase in heart rate during inspiration -Exaggerated in children, young adults, and athletes and decreases with age -Usually asymptomatic; no treatment or referral needed -Can be nonrespiratory and is sometimes seen in dig toxicity |
|
|
|
Sinus Bradycardia |
-HR is <60bpm -Every QRS Complex is narrowed and preceded by a P Wave -This is normal for patients who are in great physical fitness -When seen in elderly patients, first check medication list for any drugs that may contribute to the low HR. |
|
|
|
Causes of Sinus Bradycardia |
-Some with aging -Sleep -15-25% are due to acute MI, especially affecting inferior wall -Hypothyroidism, hypothermia, hypokalemia, or hypoglycemia -Situational: Vagal Response -Drugs: Beta Blockers, Digitalis, Calcium Channel Blockers, Amiodarone, Cimetidine, Lithium. |
|
|
|
Symptoms of Sinus Bradycardia |
-Symptoms include: Chest Pain (from coronary hypoperfusion), SOB, Syncope, Dizziness, Unusual Fatigue |
|
|
|
Treatment of Sinus Bradycardia |
-No treatment is needed if patient is asymptomatic -Elevated Medication regimen: Stop all drugs that may cause bradycardia. -Bradycardia associated with MI will often resolve as MI is resolving; will not be the sole symptom of MI -ER: Atropine 0.5mg if hemodynamic compromise (perfusion failure or low BP), syncope, or chest pain persists (May give at least 2X) -Pacing: temporary vs permanent. |
|
|
|
Sinus Tachycardia |
-HR > 100bpm - Regular Rhythm -Often difficult to distinguish P Waves and T Waves |
|
|
|
Causes of Sinus Tachycardia |
-Fever -Hyperthyroidism -Dehydration -Anxiety -Sepsis -Anemia -Stimulants (Nicotine, Caffeine) or illicit drugs -Hypotension and Shock -Pulmonary Embolism -Acute Coronary Ischemia and MI -Heart Failure -Chronic Pulmonary Disease -Hypoxia |
|
|
|
Symptoms of Sinus Tachycardia |
-Dizziness -Lightheadedness -Syncope -SOB -Sweating -Anxiety -Hypotension -Palpitations |
|
|
|
Treatment for Sinus Tachycardia |
Evaluate and treat potential causes: -Check TSH -Check CBC -Optimize CHF -COPD Regimen -Evaluate recent OTC meds Verify it is sinus rhythm -if no cause is found and is bothersome to patient, we can treat with beta blockers such as atenolol or metoprolol or rate lowering calcium channel blocker such as Diltiazem. |
|
|
|
Sick Sinus Syndrome |
-Often a result of Tachy-Brady Syndrome. Rate varies from fast to slow and back again -May manifest syncope -Occurs as a result of disease in the SA Node -Burst of atrial tachycardia such as in A-fib and is then followed by a long symptomatic sinus pause/arrest. -Usually seen when patient has a pacemaker or syncopal episode |
|
|
|
Treatment of Sick Sinus Syndrome |
-Address and treat cardiac conditions -Review medication list -Check TSH -Pacemaker for most is required |
|
|
|
PAC- Premature Aterial Contraction |
-P Wave from another ectopic Atrial focus -Occurs earlier in the cycle -Different morphology of P Wave -Benign, common cause of perceived irregular rhythm -Can cause symptoms: "Skipping" a beat, palpitations -With symptoms: may advise to stop smoking, decrease caffeine and ETOH, stress, and disrupted sleep cycle -Potentially check electrolytes and thyroid panel -Can use beta blockers to reduce frequency if problematic to patient -If patient has a history of MI, check for heart damage |
|
|
|
Paroxysmal Supraventricular Tachycardia |
-Refers to Supraventricular Tachycardia other than A-fib and A-flutter -Usually due to reentry from AV Node -HR is 150-200bpm, usually regular, P Waves are hidden in the T Waves, and QRS is narrow. |
|
|
|
Initial Evaluation for SVT |
-Is the patient stable? -Is this Sinus Tachycardia |
|
|
|
Symptoms of instability in SVT |
-Chest Pain -Decreased Consciousness -SOB -Shock Hypotension |
|
|
|
In SVT: If stable: Determine whether there is: |
A regular rhythm (Sinus or SVT) vs irregular rhythm (A-fib or A-flutter) |
|
|
|
Regular rhythm (Sinus or SVT) Determine whether P Waves are present or not |
-If you can't see, administer Adenosine (6mg, 12mg, 20mg) for chemical cardioversion, or carotid sinus massage or other vagal maneuvers. -Adenosine shocks the heart back into sinus rhythm by stopping and restarting the heart. -Give very fast followed by normal saline -Patient has to be on a defibrillator -ALWAYS DO NONINVASIVE TREATMENTS FIRST. -Counsel to avoid triggers, caffeine, ETOH, pseudoephedrine, or stress. -Ablation treatment |
|
|
|
Atrial Fibrillation |
-Irregularly irregular rhythm -Absence of definite P Waves -Narrow QRS Complexes -Can be accompanied by RVR -SA Node not firing properly -Not getting signal to conduct the atrium. |
|
|
|
-A-fib with Rapid Ventricular Response (RVR) |
-Heart is not putting out enough cardiac output because the ventricles are working faster |
|
|
|
Causes and Association of A-Fib |
-Hypertension -CHF (10-30%) -CAD -Cardiomyopathy -Mitral and Tricuspid Valve Disease -Pericarditis -Post Cardiac Surgery -Congenital (Born with it) -Hypo/Hyperthyroidism -COPD -OSA (Obstructive Sleep Apnea) -Alcoholism -Caffeine -Electrolyte Disturbances |
|
|
|
Classifications of A-Fib |
-Paroxysmal: sudden onset and sudden conversion back to sinus rhythm. *This is the most dangerous classification with high risk of pulmonary embolism* -Persistent: Greater than 7 days. -Permanent |
|
|
|
Assessment of A-Fib |
-H&P: assess heart rate, symptoms of SOB, Chest Pain, Edema (signs of heart failure and instability). -If unstable, may need to cardiovert immediately, but typically utilize medical management first. *Symptoms: Low blood pressure, unconsciousness* -Echocardiogram to evaluate valvular and overall function -Check TSH -Assess onset of symptoms: in the last 48 hours? sudden onset? or no symptoms at all? *Do we cardiovert or give anticoagulation therapy? |
|
|
|
Goals of Treatment for A-Fib |
-Decreased ventricular response to <100bpm (considered rate control) -Conversion to sinus rhythm if possible -Prevention of stroke -Is treating the causes considered the goals of treatment? *Keeping Potassium WNL is not a goal of treatment. |
|
|
|
Rate Control of A-Fib |
-Calcium Channel Blocker: Diltiazem. ^If HR is down to at least 120 titrate medication down. ^D/C med if HR is <100 -Amiodarone: Pacerone, Corderone. Dronedarone or Mutlaq. ^If BP drops but HR increases, change med. ^Amiodarone is a vesicant (causes tissue necrosis) drug, so use larger veins and 20 Gauge needle. ^Has a 60 day half-life. ^Check kidney function. -Beta Blockers: Try these first. If they don't work, change to Cardizem (Diltiazem: CCB) -Digoxin: last resort due to side effects (dig toxicity). |
|
|
|
Conversion to Sinus Rhythm |
-Rhythm vs Rate Control: if onset is within the last 24 hours, may be able to arrange cardioversion (use heparin around procedure). -Need TEE (Transesophageal Echo) prior to cardioversion (high risk for thrombus). *This looks at the back side of the heart to check for thrombus formation. -If unable to definitely conclude onset in the last 24-48 hours: need 3-4 weeks of anticoagulation therapy prior to cardioversion, and warfarin for 4-12 weeks after. |
|
|
|
Cardioversion |
-Synchronized (with the QRS complex) delivery of electrical current to the heart and depolarizes the tissues in the re-entrant circuit. -Chemical, IVPB, done every 15 mins. -Not to be confused with defibrillation. |
|
|
|
Defibrillation |
-Non-Synchronized delivery of a current to the heart |
|
|
|
Chemical Cardioversion |
-Ibutilide (Corvert) -Adenosine -What about Digoxin and Amiodarone? ^Digoxin is the last resort medication due to its side effects. ^Amiodarone is a vesicant (causes tissue necrosis) |
|
|
|
Acute Management of A-Fib |
-Heparin Drip ^Weight based ^Use of Bolus ^Then protocol for dose changes is based on aPTT results. *Draw every 6 hour until there are 2 therapeutic results. ^Very short half life ^Requires dual sign off *Heparin antidote: Protamine Sulfate -Dose not dissolve existing blood clots, but prevents from new ones from forming. -Enoxaparin (Lovenox): ^Monitor INR and Platelets ^Given BID (am, pm) without needing heparin ^Is not cost effective ^Therapeutic ^May be given prophylactically to prevent blood clots (usually 40mg). *If a patient has A-Fib, what would you question giving? Heparin, Lovenox is the better choice!" |
|
|
|
Prevention of Stroke |
Long Term: -Warfarin (Coumadin): ^ INR monitoring- Check weekly until therapeutic then monthly. ^Warfarin Antidote: Vitamin K ^ Multiple drug interactions- Tagamet ^Dietary Considerations- No leafy green vegetables ^ Goal: INR of 2.0-3.0 (2.5) -Apixaban (Eliquis) -Dabigatran (Pradaxa) -Rivaroxaban (Xarelto) -Edoxaban (Savaysa) *Do not eat green leafy vegetables as they contain large amounts of Vitamin K. ~Dabigatran, Rivaroxaba, and Edoxaban are very expensive! |
|
|
|
Atrial Flutter |
-Occurs from the Atrium, generating impulses at a rate of 250-400bpm. -A rapidly-firing Atrial ectopic focus -Rhythm is regular with characteristic of a "sawtooth" pattern -Causes and treatments are the same as A-Fib. |
|
|
|
1st Degree AV Block |
-Prolong PR interval of >200ms -If accompanied by wide QRS complexes, refer to cardiology as patient has a high risk of progression to 2nd and 3rd degree blocks -Otherwise, benign if asymptomatic. *Check medications to see if they are the cause of the 1st degree block. |
|
|
|
2nd Degree AV Block Mobitz Type 1 (Wenckebach) |
-Progressive PR elongation, with eventual non conduction of a P Wave. -May be in 2:1 or 3:1 ratio -Patient may need a pacemaker -Longer, longer, drop, you have a Wenckebach. -Usually asymptomatic, but with accompanying bradycardia can cause angina and syncope, especially in elderly. ^ Will need pacing if symptomatic. - Also can be caused by drugs that slow conduction such as beta blockers, calcium channel blockers, digoxin. -Correct if cause is reversible, avoid medications that block conduction. |
|
|
|
2nd Degree AV Block Mobitz Type II (Mobitz 2) |
-Normal PR Intervals with sudden failure of P Wave to conduct. -Usually below AV Node and accompanied by BBB (Bundle Branch Block) or fascicular block (Left Bundle Branch block). -Often causes pre/syncope -Symptoms often worsen with exercise. - Generally need pacing, possibly urgently if symptomatic |
|
|
|
3rd degree AV Block (Also known as an "escape rhythm") |
-Complete AV disassociation, HR is a ventricular rate. ^Ventricles usually only fire at 30 beats per minute decreasing Cardiac Output. -Will often cause dizziness, syncope, angina, and heart failure. -Can degenerate to V-Tach, V-Fib or prolonged Sinus pause -Will need pacing with an urgent referral |
|
|
|
Heart Block Poem |
-If the R is far from P, you have a FIRST DEGREE. -Longer, longer, longer, drop! Then you have a WENCKEBACH. -If some P's don't get through, then you have MOBITZ 2. -If P's and Q'd don't agree, then you have a THIRD DEGREE. |
|
|
|
PVC - Premature Ventricular Contraction |
-Extremely common throughout the population, both with and without heart disease. -Wide, bizarre, QRS Complexes. -Usually asymptomatic, except rarely dizziness or fatigue in patients that have frequent PVCs and significant left ventricle dysfunction -Generally not dangerous, but if the patient has too many in a row, it may turn into V-Tach -Treatment is not necessary when risks outweigh the benefits. ^If patient is symptomatic then give Beta Blockers or Amiodarone. ^Remove lifestyle triggers ^Optimize cardiac and pulmonary disease management. -Unifocal vs Multifocal -R on T phenomenon -Bigeminy, Trigeminy, quadrigeminy, etc. -May feel like paliptations. |
|
|
|
Non-Sustained Ventricular Tachycardia (Non-Sustained V-Tach) |
-Defined as 3 or more consecutive ventricular beats, but less than 10. -Rate of >120bpm lasting less than 30 seconds. -May be discovered on a Holter monitor or other exercise testing. -Heart may have a spurt of energy then goes back into sinus rhythm -Need to exclude heart disease with echocardiogram and stress testing -May need anti-arrhythmia treatment such as Amiodarone, Flecainide, Sotalol, etc. -In presence of heart disease, patient has an increased risk of sudden death. |
|
|
|
Sustained Ventricular Tachycardia (V-Tach) |
-Ominous rhythm due to low cardiac output, minimal filling time, and lack of Atrial kick. ^Lowest Cardiac output of any other cardiac rhythm. -Monomorphic vs Polymorphic (Torsade's de Pointes) ^Polymorphic looks like a party streamer; Give Magnesium. -Ventricular rate is 100-200bpm with wide, bizarre QRS Complexes. -Causes of V-Tach: ^ CAD, MI, Dig Toxicity, CHF, drug toxicity, R on T Phenomenon. -Treatments of V-Tach: ^Always assess pt first ^Stable with a pulse: Antiarrhythmic drugs such as Amiodraone, Lidocaine, or Magnesium. ~Lidocaine deadens area around the heart and numbs the nerves. -Unstable without a pulse- Start CPR immediately, defibrillation, and begin ACLS protocols. |
|
|
|
Ventricular Fibrillation |
-Rapid, disorganized quivering of the Ventricles. Very erratic rhythum -No Cardiac Output -Death is imminent and requires immediate defibrillation -CPR and ACLS measures are instituted. ^Every 2 minutes, pulse check and shock. ^Every 3 minutes, give epinephrine ^Code lasts until somebody calls it. |
|
|
|
Unstable V-Tach and V-Fib |
-CPR -Immediate defibrillation -Vasopressin and Epinephrine -Amiodarone and Lidocaine -Magnesium for Torsade's de Pointes |
|
|
|
Asytole and PEA - Pulseless Electrical Activity |
-"Flatline" -May also present as PEA -Check the patient and confirm in 2 leads -CPR ONLY DO NOT DEFIBRILLATE -Epinephrine (1mg) -Critical to reverse identified cause if able -May use pacing until rhythm is established |
|
|
|
Pacemakers |
-Definition: Delivers artificial stimulus to heart. Causes depolarization and contraction. *Does not pump the heart, but provides impulse to keep it pumping on its own. -Uses: Bradyarrhythmia, Asystole, Tachyarrhythmia (Override pacing). -Atrial pacemaker shows up as a line on the P Wave of an ECG. -Ventricular pacemaker show up as a line beginning of the QRS complex of and ECG. -No line present on an ECG indicates that the heart is pumping on its own without the need of pacemaker. |
|
|
|
Types of Pacemakers |
-Fixed: fires at a constant rate -Demand: senses Patient's rhythm. Fires only if no activity is sensed after preset interval (escape interval) -Transcutaneous vs Implanted: single chamber vs dual chamber *Special considerations: Does not affect treatment of cardiac arrest. -Do not fire defibrillator directly over pacemaker generator. -Pacemakers can cause AEDs to delay advising to shock. |
|
|
|
Implanted Defibrillators |
-AICD: Automated Implantable Cardio-Defibrillator. ^Uses: -Dangerous Tachyarrhythmias such as V-Tach or V-Fib -Used as a safety measure in patients with extremely low ejection fraction who are prone to the development of deadly arrhythmias. -Programmed at implantation to deliver therapy at present parameters. -Also function as a pacemaker. |
|
|
|
AICD Potential Complications |
-Fails to deliver therapies as intended (failure to capture). ^Worse possible complication -Delivers therapies when not appropriate (failure to sense). ^Broken or malfunctioning lead. ^Parameters not specific enough and may need adjusting. -Continues to deliver shocks ^Requires a reset. ^May be shut off with a donut magnet. |
|
|
|
Care of Pacemaker Patients |
-Assess for Complications: ^Bleeding ~Pressure dressing applied ~remove pressure dressing in the morning after implantation. -Pneumothorax (puncture lung) -Infection *Sling/Swathe: -Keeps patient from moving muscles and dislodging device while it is implanting into the heart muscles. -Activity Limitations: ^Patient is on bedrest at no more than 30 degrees for the first 4 hours after implantation, then bedrest for 24 hours after implantation. -Follow up Care |
|

