![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
39 Cards in this Set
- Front
- Back
|
If we see a negative p-wave, and a shortened PR (but normal QRS, QT, and T)... what should we think about?
|
depolarization of the atria is heading in the opposite direction of normal, and it's getting to the ventricle sooner.
= junctional/ectopic rhythm. |
|
|
Describe first degree AV block.
|
not really even a 'block' persay, it's just a large delay b/t p-wave and QRS.
Everything else is normal though, and every P has a QRS, etc. |
|
|
Second Degree AV block has two types, what are they? What is also called Wenckebach?
Which is more dangerous? Why? |
Mobitz type I, Mobitz type II
Type I Type II - it is more likely to progress to complete block. |
|
|
Describe the Wenckebach irregularity.
Describe 2nd deg. AV Type II. |
Progressive prolongation of the PR interval, until you lose a beat. You will often see a pattern of "group beating"
fixed P to R relationship (consistent conduction), just suddenly dropped a beat. NO steady prolongation. |
|
|
What is seen in a high grade AV block?
Third Degree AV block? |
Basically a more severe Mobitz type II - this is a bridging term.
can be 3:1 or larger.... Complete dissociation of P waves from QRS |
|
|
What is a Supraventricular tachycardia? Another name?
Characteristics? |
rhythm process in which the ventricles are activated from the atria or AV node/His bundle region
- narrow QRS tachycardia QRS typically narrow (w/o additional BBB) Usually paroxysmal (starts and stops abruptly) = PSVT |
|
|
What are some causes of sinus tachycardia?
|
Hypovolemia
Fever Respiratory distress Hyperthyroidism Bronchodilators exercise, excitement, etc. |
|
|
What is the typical direction for an atrial flutter circuit?
What is seen on ECG? Most important leads to look at? |
counterclockwise.
P-wave vector changes, now looks away from your inferior leads, and is aiming more towards V1. - sawtoothed P-waves in inferior leads w/ variable ventricular response - positive in V1. - ~300waves/min inferior leads and V1 |
|
|
What is a typical description of an a.fib rate?
Which lead is it best seen in? What is actually keeping us alive? |
Chaotic, rapid atrial rate at 400-600 bpm
No well described circuit... V1 The fact that most impulses are being blocked by the AV node. - Irregular which ones get through! |
|
|
What are the 3 forms of a.fib? Which is unable to be restored to sinus rhythm by Tx?
Associated dz? |
Paroxysmal, Persistant, Permanent
Chronic/Permanent Cardiac dz like HTN, CAD, etc. |
|
|
What can RF be used to treat? What does it do?
|
a.flutter, afib, SVT
Compartmentalizes the atria |
|
|
What is ventricular tachycardia? (VT) Common rate range?
Can be either non-______ or ______. What do these categorizations mean? Features? What is a specific sign (but not a sensitive one)? |
Focused firing from the ventricles
100-250bpm non-sustained or sustained: Non-sustained VT is defined as a run of tachycardia of less than 30 seconds duration; a longer duration is described as sustained VT. Wide-complex tachycardia P's aren't associated with V's.... look for them - they are specific but not very sensitive. |
|
|
What is the difference between a monomorphic and a polymorphic VT?
When you think something might be VT or PSVT, what do you do? |
VT may be monomorphic (typically regular rhythm originating from a single focus with identical or similar QRS complexes) or polymorphic (may be irregular rhythm, with beat to beat variation in QRS complexes).
Treat as if VT. some Tx for PSVT can kill VT pts. |
|
|
* Rate greater than 100 beats per minute (usually 150-200)
* Wide QRS complexes (>120 ms) * Presence of atrioventricular (AV) dissociation * Fusion beats .... suggests? |
VT.
|
|
|
Monomorphic VT implies ______, but sometimes be seen in structurally ______ hearts.
Polymorphic VT can result from ________ or conditions that prolong _______ _______. |
Heart Dz; normal
myocardial ischemia; ventricular repolarization |
|
|
Totally chaotic rapid ventricular rhythm; often precipitated by VT is called? Tx?
Order the following: Polymorphic VT, VF, Monomorphic VT |
VFibrillation
Fatal unless promptly terminated (DC Shock) Mono --> poly --> VF |
|
|
What is a delta wave?
|
preexcitation of the ventricle, obliterating QRS interval. Depending on how much preexcitation you get, you'll get more/less slurring.
|
|
|
What are some characteristics of Wolff-Parkinson-White Syndrome?
|
very short PR interval, slurred QRS (Delta waves). Very suspicious for preexcititation of the ventricles.
|
|
|
(aVF, aVL, V1) = format of positivity of delta wave. Given these patterns, give probably WPW AP location:
+ + - + - + - - + - + + |
Left lateral
left posterior septal Right post. septal Right. Lateral/anterior |
|
|
What else can sort of cause the Sx of WPW?
|
Atrioventricular re-entry tachycardia, if it is orthostatic.
|
|
|
What defines a Long QT (LQT)? Autosomal dominant inhereited dz? Recesive? Is sporadic dz possible?
What are the three types of LQT and their pathophysiological mechanisms? Where is each seen? |
QTc > .46s (fem) .44 (male)
Romano-Ward Syndrome Jervelll-Lange-Nielsen Syndrome Yes. LQT 1 (exercise/swimming), 2 (emotion/auditory): decreased function of 2 potassium channels, prolong QT LQT 3 (die in sleep/rest): gain of functon in NA channel, prolongs ST segment and thereby prolongs QT |
|
|
Of the LQTs the one that has Tall, wide-based T-waves?
T-valve alternans, low or not T-wave? tall, wide based waves? |
LQT1
2 3 |
|
|
The ST segment represents the current flow generated when myocardial cells repolarize
This is mediated by the opening of ________ channels on the cell membrane allowing ________ to flow out of the cell and return to a negative membrane potential |
potassium, potassium
|
|
|
ST elevation in one region of the heart can yield __ ________ on the other side.
|
ST depression.
|
|
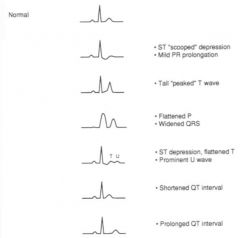
Please give the drug therapy or ion change (increase/decrease) associated with each of the following ECG changes.
|
|
|

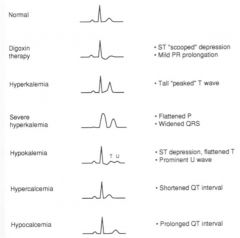
Please fill in the blanks.
|

|
|
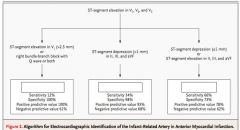
Plz fill in the blanks.
|
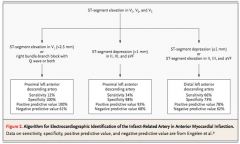
|
|
|
ST depression, T wave inversion, no Q waves
ST seg elevation, no Q waves Abnormal Q waves, ST seg elevation or depression, T waves may be abnormal please match these with MI, myocardial ischemia, and myocardial injury |
Ischemia: ST segment depression, T wave inversion, no Q waves
Injury: ST segment elevation, no Q waves Infarct: abnormal Q waves, ST segment elevation or depression, T waves may be abnormal |
|
|
Leads __ and ___ are the most sensitive to look at for MI b/c they're over the most muscle.
|
V5 and V6
|
|
|
ST elevation that can signify an MI has what characteristics?
|
>1-2mm in two or more contiguous leads
usually upwardly convex configuration |
|
|
When localizing an MI, tell me what location you think of when you see q's in:
V1-V3 V2-V4 V4-V6 I, avL II, III, avF Do these localizations hold true for RBBB? LBBB? Which leads can be assessed, if this doesn't hold true? |
anteroseptal
anterior anterolateral high lateral inferior (basically just the areas that they're over) RBBB yes. LBBB, no. - have to assess only V5, V6, I, aVL |
|
|
R wave should be (smaller/larger) in leads over the infarcted tissue?
How many leads w/ Q are needed for true localization? How about for just calling the cath lab? |
smaller.
3 leads. 2 leads. |
|
|
What leads are opposite of the inferior leads?
|
The anterior leads! V1-V3
|
|
|
To Dx an Acute MI in LBBB, you need:
>/= ___mm STE concordant w/QRS >/= ___mm STD in _____ >/= ____mm STE discordant w/ QRS |
1mm
1mm in V1-V3 5mm |
|
|
How can you Dx a posterior infarct?
|
R in V1 or V2 >/= 0.04
R > S in V1 or V2 -- This is the 'mirror image' of a Q wave if we had a posterior lead. ***Understand?*** Acute STD & upright T in V1 or V2 |
|
|
What is Cabrera's sign?
Does LBBB preclude Dx-ing MI? |
'notching' or the ascending S in the mid-left precordial leads.
No, but it can mask changes of prior or acute MI --> reducing sensitivity of ECG in those situations. |
|
|
When you see an ECG i/ someone w/ respiratory infection where the J-point (bt QRS and ST/T) is trying to reach back to baseline.... coupled with diffuse elevations.... what should you be suspicious of?
|
pericarditis.
|
|
|
ST elevation (all leads except aVR)
J point returns to baseline T wave inversion ECG resolution ST/T changes PR depression Low voltage QRS Electrical alternans Sinus tachycardia --- what should we be thinking of? |
Acute pericarditis
|
|
|
Acute MI
Aneurysm Pericarditis Early repolarization LV hypertrophy LBBB/RBBB Paced rhythms Hyperkalemia Assorted cardiomyopathies (HCM, WPW, Brugada, infiltrative disease, myocarditis) Congenital heart disease Pulmonary disease (chronic, PE) .....all are on the diff Dx of ___ _______. |
ST elevation
|

