![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
300 Cards in this Set
- Front
- Back
|
Name the nurse that started the Red Cross. |
Clara Barton |
|
|
Describe the nurse that started the Red Cross. |
- gave care in the tents near the battlefields during the Civil War. - did not discriminate, gave care regardless if from the North or the South, Black or White. |
|
|
Who was known as the "Lady of the Lamp"? |
Florence Nightingale. |
|
|
Describe the nurse known as the "Lady of the Lamp". |
- Was a field nurse during the Crimean War - in 1860, organized the first school of nursing at St. Thomas hospital in London. - considered the nurse to be a colleague of the physician rather than the servant - used her experience to lobby politicians and physicians about the importance of nursing and the need for public health reform - her practices remain a basic part of nursing today |
|
|
What did Florence Nightingale implement to help decrease mortality, length of hospital stay and nosocomial infections? (important) |
Air, Light, Adequate Ventilation and Space to assist the patient to recuperate. |
|
|
What does the definition of nursing include? |
- The promotion of health - The prevention of illness - The care of the ill, disabled and dying people |
|
|
When rendering care, what guides a nurse? |
A code of ethics developed by the American Nurses Association. |
|
|
What is nursing? A profession, an occupation or a discipline and why? |
A profession. - it requires an extended education - requires a body of knowledge - provides a specific service - has autonomy - incorporates a code of ethics |
|
|
How can nursing improve it's recognition as a profession? |
- Standardizing educational requirements for entry - enacting uniform continuing education requirements - encouraging more nurses to participate in professional organizations - educating the public about the true nature of nursing practice |
|
|
Who can be called a "nurse"? |
- A person who has graduated from an accredited nursing program - a person who has passed a licensure exam |
|
|
What's the difference between a registered nurse and a practical nurse? |
A registered nurse requires a Bachelor's degree and a LPN (Licensed Practical Nurse) works under an RN or a physician. |
|
|
What are the phases of nursing? |
Stage 1: Novice - a beginner or student Stage 2: Advanced beginner - a new nurse Stage 3: Competent - 2 to 3 years in the same type of position Stage 4: Proficient - more than 2 to 3 years in the same position Stage 5: Expert - diverse experience with an intuitive grasp |
|
|
What is the nurse practice acts? |
Laws to regulate nursing practice at the state level. Each US state has their own. |
|
|
What is the state boards of nursing? |
The agency responsible to regulate nursing practice. |
|
|
What does NCLEX stand for? |
National Council Licensure Exam |
|
|
What is direct care and give an example. |
Involves personal interaction between the nurse and the patient. An example would be giving medication. |
|
|
What is indirect care and give an example. |
Working on behalf of the patient. An example would be to arrange unit staffing or stocking the code cart. |
|
|
What is the purpose of nursing care? |
Health promotion, illness prevention, health restoration, and end of life care. |
|
|
Where do nurses work today? |
Only 62% work in hospitals. Others work in extended care facilities, ambulatory care, in patient homes and in the community such as schools. |
|
|
What are outside nursing influences? |
The National Economy Consumers Legislation Women's movement Collective bargaining Aging Society Technology |
|
|
Name the characteristics of a full-spectrum nurse. |
Clinical judgement Critical thinking Problem solving |
|
|
What does clinical judgement include? |
Observing comparing contrasting evaluating |
|
|
What is critical thinking? |
Involves collecting and analyzing information and carefully considering options for action |
|
|
What is problem solving? |
Considering an issue and attempting to find a satisfactory solution |
|
|
What is the science of nursing based on? |
The body of knowledge that is consistently changing and evolving. |
|
|
What is the art of nursing based on? |
The practice of compassion, respect, & dignity given to patients & family members. The patient is the center of care and the family members will also have needs. |
|
|
What are the six quality and safety competencies for nurses? |
1. patient-centered care 2. teamwork and collaboration 3. evidence-based practice 4. quality improvement 5. safety 6. information |
|
|
What is nursing research and what does it encompass? |
A systemic, objective process of analyzing phenomena of importance in nursing. It encompasses all clinical practice arenas, nursing education and nursing administration. |
|
|
What are the ways to gain nursing knowledge? |
- trial and error plus common sense - authority and tradition - intuition and inspiration - logical reasoning |
|
|
What does the scientific method do? |
By being a systematic data collection, it makes data observable and verifiable. |
|
|
What is the purpose of the scientific method? |
To describe, explain and predict events. |
|
|
What two major categories does the scientific method research design fall into? Explain them. |
Quantitative (generalized to populations) and Qualitative (focuses on lived experiences of people). |
|
|
What are the steps of the research process? (important) |
- select and define the problem - select a research design - collect data - analyze the data - use the research findings |
|
|
What are the rights of research participants? |
- informed consent - right not to be harmed - right to full disclosure - right to self-determination (right to say no) - rights to privacy and confidentiality |
|
|
How do nurses identify clinical nursing problems? |
- through experience - social issues - theories - ideas from others - nursing literature |
|
|
What is a PICO question? (important) |
A question to help guide research P - Patient/ population (which age, gender, etc) I - Intervention (which one is worthwile) C - Comparison intervention (what others are used) O - Outcome (what's the desired result) |
|
|
When analyzing research, what are the 4 questions to keep in mind? |
1. What is the book (journal, article) about as a whole? 2. What is being said in detail and how? 3. Is the book (journal, article) "true" in whole or in part? 4. What do you make of it? |
|
|
After answering the 4 questions to keep in mind regarding research, what questions should we then consider? |
1. Do the articles together offer evidence to explain or answer my PICO questions? 2. Do the articles show support for the reliability and validity of the evidence? 3. Can I use the evidence in practice? |
|
|
What is validity? |
When the study actually measures the concept it claims to measure. |
|
|
What is reliability? |
It refers to the accuracy, consistency, and precision of a measure. Repeating the same test will result in the same outcome. |
|
|
What is the reason for conducting research? |
To establish evidence-based practice, utilize research. |
|
|
How is evidence used in the clinical setting? |
- teaching tools - clinical practice guidelines and policies and procedures - new assessment or documentation tools |
|
|
What is nursing theory? |
An organized set of related ideas and concepts in nursing. |
|
|
What does nursing theory do? |
- Helps us find meaning in our clinical experiences - organizes our thoughts around an idea - helps us develop new ideas and insights into the work we do |
|
|
What are the components of a theory? (important) |
- Phenomena (Observed reality) - assumptions - concepts - definitions - statements/ propositions
|
|
|
What is a paradigm? |
A pattern of thought that is used to describe a domain (perspective of a profession) |
|
|
What is a conceptual framework? |
a set of concepts related to form a whole (not based on research) |
|
|
What is a model? |
a symbolic representation of a framework or concepts (diagram, Picture, drawing) |
|
|
What are the essential concepts of a nursing theory? |
- person/ patient - environment - health - nursing |
|
|
What is inductive reasoning? |
Goes from specific to general. Often used in nursing practice. Ex. my ball is round so all balls must be round. |
|
|
What is deductive reasoning? |
Goes from general to specific. Ex. All balls are round. This is round so it must be a ball. |
|
|
Describe nursing theories. |
- They describe, explain and predict human behavior - they are used in practice, education and research - since much of nursing cannot be measured, theories help identify what nurses do |
|
|
Name some important nursing theorists. |
- Florence Nightingale - Virginia Henderson - Hildegard Peplau - Patricia Benner and Wrubel - Madelaine Leninger - Jean Watson
|
|
|
Name some theories from disciplines other than nursing. |
- Maslow's hierarchy of basic human needs - stress and adaptation theory (some stress is good) - developmental theories (life stages) - systems theory (subsystems - can be applied to any discipline) |
|
|
What is the first step to good care? |
Communication |
|
|
How do nurses communicate with patients, families and other health professionals? |
With nonverbal, verbal and technological skills. |
|
|
What is communication? |
- sharing or transmitting thoughts and feelings - A process: the act of sending, receiving, interpreting and reacting to a message - content: the actual subject matter, words, gestures and substance of the message |
|
|
What are the 3 levels of communication? |
- intrapersonal (self-talk) - interpersonal (one on one) - group (such as a staff meeting) |
|
|
What are the components of communication? |
- subject matter - words - gestures - substance of the message - open to interpretation (Ex. I slept through lunch) |
|
|
What is the active part of communication? |
- sending - receiving - interpreting - reacting |
|
|
What are the 5 elements of communication? |
1. Sender (encoding) 2. message (content) 3. channel (means of conveying face to face, text) 4. receiver (decodes message) 5. feedback (both verbal and nonverbal) |
|
|
What is "decoding" during the communication process? |
The interpretation of the message by the receiver. |
|
|
What influences interpretation by a receiver? |
- educational background - culture - age - past experiences |
|
|
What are the types of verbal communication? |
- vocabulary - denotation - connotation - pacing - intonation - clarity & brevity - timing & relevance - presence of others - credibility - humor |
|
|
The nurse is teaching the client about his upcoming procedure and the client is very stressed. It would be most important for the nurse to: |
Determine if the teaching should take place at a different time. Clients who are stressed may be unable to listen fully and will not receive/understand the intended message. |
|
|
What is nonverbal communication? |
The unconscious use of body language when sending a message |
|
|
What are the factors that affect a person's nonverbal communication, or body language? |
- eye contact - facial expression - posture & gait - personal appearance - distance - gestures - touch |
|
|
What are the factors that affect communication in general? |
- environment (is it quiet?) - developmental factors (child? language skills?) - gender - territoriality - sociocultural factors - roles and relationships - personal space |
|
|
How does space affect communication? |
- intimate - 18 inches - personal - 18 inches to 4 feet - social - 4 to 12 feet - public - 12 feet |
|
|
What does it mean to communicate assertively? |
It means to express both positive and negative thoughts and feelings: - directly - openly - honestly - spontaneously - responsibly - without judgement - focus on the issue, accept criticism and do not become defensive |
|
|
What is a therapeutic relationship in health care? |
- it Focuses on improving the health of the client - it Provides necessary information about health, treatments, and care - it Involves the use of therapeutic communication |
|
|
What are two keys to therapeutic communication? |
1. patient-centered - focusing on the patient 2. goal-directed - intended to bring about change to the patient |
|
|
What are the phases of the therapeutic relationship? |
1. pre-interaction phase 2. orientation phase 3. working phase 4. termination phase (POWT) |
|
|
What is the pre-interaction phase of the therapeutic relationship? |
- occurs before meeting the patient - when information is gathered prior to meeting the patient |
|
|
What is the orientation phase of the therapeutic relationship? |
Meeting the patient and establishing a rapport and trust. |
|
|
What is the working phase of the therapeutic relationship? |
- Use of techniques applicable to therapeutic communication - Active part of the relationship - Client (patient) clarifies feelings and concerns through verbal and nonverbal communication - Nurse & client work together to solve problems & accomplish goals |
|
|
What is the termination phase of the therapeutic relationship? |
- Conclusion of the relationship - End of shift - Patient is discharged |
|
|
Use of the statements "Tell me more about…" or "I see" encourage clients to continue talking and expressing themselves. What is this called? |
Encouraging elaboration |
|
|
What are the key characteristics of therapeutic communication? |
- Empathy - Respect - Genuineness - Concreteness (like "45 min" instead of "awhile") - Confrontation |
|
|
What are the client factors affecting effective therapeutic communication? |
- Language barrier - Impaired cognitive skills - Sensory-perceptual alterations - Physiological barriers (expressive or receptive aphasia) |
|
|
What is expressive aphasia? |
When a person cannot express themselves (speak), though they may understand when spoken to. |
|
|
What is receptive aphasia? |
When a person can speak normally but may not understand what is being said to them. |
|
|
What enhances therapeutic communication? |
- Active Listening - Establish trust - Be assertive - Restate, clarify, and validate message - Interpret body language - Share your observations to clarify - Explore Issues: Use open-ended questions - Use silence - Process Recordings 2 people talk 3 person records - Summarize the conversation |
|
|
What nonverbal communication is important in a therapeutic relationship? |
1. Sit down to talk with your client 2. Use direct eye contact: shows interest and attention 3. Make sure your facial expression matches the patient's 4. keep a therapeutic distance of 18"- 4 feet 5. Lean forward to show caring 6. Use touch if appropriate |
|
|
What are the barriers to therapeutic communication? |
- Asking too many questions - Closed-ended questions - Too much information: fire hose: over whelming - Asking “Why?” - Changing the subject abruptly - Failing to listen & probing the patient (interrogation) - Failing to explore issues in detail - Expressing approval or disapproval - Offering advice - Giving false reassurance - Stereotyping - Using patronizing language |
|
|
What are important things to keep in mind regarding communication with a patient from another culture? |
- use a Translator (never a family member) - can use a Picture board - Know your own culture & patient’s culture - Respect and convey empathy - Direct eye contact - How much space? - Touch appropriate? - Proceed slowly - make no assumptions |
|
|
What are important things to keep in mind regarding communication with an impaired patient? |
- Always try to communicate - Don’t rush client - Use multiple communication modalities - Provide reminders - Orientate them - they may not remember - Stimulate memory - Use short sentences - Limit choices - Ask yes/no ? - Avoid slang - Use gestures |
|
|
How do you communicate with a speech impaired client? |
Can use nonverbal communication or a picture board. Sometimes a family member may know what they're trying to say. |
|
|
How do you communicate with a cognitive impaired client? |
Always try to communicate, even if you don't know if they understand. Don't rush, ask easy questions. |
|
|
How do you communicate with a hearing impaired client? |
Talk slowly and clearly and be sure to face them directly. They may read lips. |
|
|
How do you communicate with a vision impaired client? |
Always announce when you're in the room. Be sure to explain before any procedures. |
|
|
How do you communicate with an unresponsive client? |
Treat them as though they are responsive. They may still hear you and may still be aware that you are there. |
|
|
Summarize actions for therapeutic communication. |
- keep a positive attitude - keep the goals of the interaction in mind - focus on the patient |
|
|
What is infection? |
When microorganisms capable of producing disease invade the body |
|
|
What are the 6 links to the spread of infection? |
1. The infectious agent 2. The reservoir 3. The portal of exit (from the reservoir) 4. The mode of transmission 5. The portal of entry 6. A susceptible host |
|
|
What are infectious agents? |
- pathogens - normal flora that become pathogenic |
|
|
What is a reservoir? |
Where pathogens live and multiply. For example, in people, or contaminated water. |
|
|
What is a portal of exit? |
The way in which a pathogen leaves the reservoir. For example, body fluids. |
|
|
What is a mode of transmission? |
- direct (kissing) or indirect (fomite like a door handle) contact - from a droplet (expelled onto you) - airborne (from sweeping or air conditioning) |
|
|
What are the stages of infection? |
- Incubation (no symptoms, but contagious) - prodromal (vague symptoms) - illness (symptoms) - decline (getting better) - convalescence (return to health) |
|
|
How are infections classified by location? |
- local (in the wound) - systemic (in the blood or lymphatic system) |
|
|
How are infections classified by duration? |
- acute (rapid onset and stays weeks or days) - chronic (slow onset and stays weeks to years) - latent (infection present with no discernible symptoms) |
|
|
If a person is sick with mono and then gets a cold, what is the cold considered to be? |
A secondary infection. |
|
|
What is a healthcare related infection called? |
Nosocomial infection. |
|
|
What kinds of nosocomial infections are there? |
Exogenous and endogenous |
|
|
What is an exogenous nosocomial infection? |
A pathogen acquired from the healthcare environment. |
|
|
What is an endogenous nosocomial infection? |
Normal flora multiply and cause infection as a result of treatment |
|
|
What is drug resistance? |
Microorganisms (mainly bacteria) that are able to mutate in order to survive exposure to antimicrobial drugs |
|
|
What are the primary defenses against infection? |
Anatomical features limiting pathogen entry - Intact skin - Mucous membranes - Tears - Normal flora in GI tract - Normal flora in urinary tract (MINT) |
|
|
What are the secondary defenses against infection? |
Biochemical processes activated by chemicals released by pathogens - Phagocytosis - Complement cascade - Inflammation - Fever |
|
|
What are the tertiary defenses against infection? |
- Humoral immunity (B-cells) - cell-mediated immunity (T-cells) |
|
|
What are factors that increase infection risk? |
- Developmental stage (babies put everything in their mouths) - Breaks in the skin - Illness/injury, chronic disease - Smoking, substance abuse (interferes with normal respiratory function) - Multiple sex partners - Medications that inhibit/decrease immune response - Nursing/medical procedures |
|
|
What are the factors that support immune function? |
- Adequate nutrition (to be able to make cells) - Balanced hygiene (not too much or too little) - Rest/exercise - Reducing stress - Immunizations |
|
|
What can the hospital do to prevent infection? |
Maintain medical asepsis (state of cleanliness) |
|
|
How does the hospital maintain medical asepsis? |
- Maintaining clean hands - Maintaining a clean environment - Following Centers for Disease Control (CDC) guidelines |
|
|
If the patient has contact precautions beyond standard of care and requires extra PPE, where should the PPE be kept? |
On a cart outside the patient's room. |
|
|
If the patient has droplet precautions and needs to be transported, what are the requirements for transport? |
The patient should wear a mask, but the transporter is not required to wear one. |
|
|
If the patient has airborne precautions and needs to be transported, what are the requirements for transport? |
The patient should wear a mask and any infectious lesions must be covered. Transporter is not required to wear a mask. The receiving department must be notified of patient's imminent arrival. |
|
|
If a patient requires PPEs, when should the PPE be removed? |
Before leaving the patient's room. |
|
|
When a pathogen is spread by direct contact, what could be sources of infection? |
- draining wounds - secretions - supplies |
|
|
If the patient has contact precautions, what should be done with linen laundry? |
It should be double-bagged and marked with precautions on the bag. |
|
|
If the patient has contact precautions, what should be done with contaminated items? |
They should be disposed of. |
|
|
If the patient has contact precautions, what should be done with contaminated items that are not disposable? |
They should be kept in the room with the patient until the patient is discharged. |
|
|
If the patient has droplet precautions, what additional PPE should be used? |
Mask and eye protection within 3 feet of the patient. |
|
|
Name some pathogens that can be transmitted airborne. |
- Tuberculosis - measles - chickenpox |
|
|
If the patient has airborne precautions, what additional PPE should be used? |
A special room and a special mask for the caregivers. |
|
|
If the patient has contact precautions, what additional PPE should be used? |
Gown. |
|
|
What patients require protective isolation? |
immune-compromised client population |
|
|
What precautions are required for patients in protective isolation? |
- Room with special ventilation and air filters; no carpeting; daily wet-dusting - Avoiding standing water in the room (e.g., humidifier) - Nurse not assigned to other clients with active infection - Standard and transmission-based precautions, plus mask and other PPE (to protect patient) |
|
|
What is involved in maintaining a clean environment? |
- Clean spills and dirty surfaces promptly - Remove pathogens through chemical means (disinfect) - Remove clutter - Consider supplies brought to the client room as contaminated - Consider items from the client’s home as contaminated |
|
|
What do you do if you are exposed to any blood, body fluid, or tissue? |
1.) first wash the exposed area 2.) notify appropriate people 3.) seek medical attention 4.) complete an injury report |
|
|
Why would you need to complete an injury report? |
So the hospital is aware of why it happened and how it happened in an effort to make changes and avoid it happening again. |
|
|
The client has a draining abdominal wound that has become infected. In caring for the client, what precautions will the nurse implement? |
Contact precautions. |
|
|
How is sterilization performed? |
With high heat or gas. |
|
|
How is surgical asepsis achieved? |
- with sterile tools - use of a sterile field - use of surgical hand scrub - use of surgical attire |
|
|
What is a sterile field used for? |
It is used in healthcare settings to perform a variety of sterile procedures. Only sterile objects are placed in the field. |
|
|
What is the definition of mobility? |
A person's ability to move in the environment. |
|
|
What is the definition of physical fitness? |
The ability to carry out activities of daily living with vigor and alertness without fatigue and enough energy for leisure pursuits and to respond to emergencies. |
|
|
What is the definition of exercise? |
A planned, structured, repetitive and purposeful activity for improving or maintaining physical fitness, performance or health. |
|
|
What 4 concepts involves moving the body? |
1. Body alignment 2. Balance 3. Coordination 4. joint mobility |
|
|
What does body alignment do? |
Places the spine in a neutral position and gives balance |
|
|
What is "balance"? |
Line of gravity from head to feet |
|
|
What is "coordination"? |
Smooth movement between nervous system and musculoskeletal system. |
|
|
What does joint mobility do? |
Allows one to sit, stand, walk and bend |
|
|
How should we move our body without causing injury? |
- have proper posture - have a wide base for support (feet spread) - avoid bending or twisting while lifting - squat to lift - keep objects close when lifting - raise the bed to hip height when working - Push instead of lift to move something - use help - people or equipment |
|
|
What are the tips for maintaining good posture? |
- don't stand in one position for too long - if you must stand a long time, place a foot on a box - don't lock knees while standing - tightening stomach muscles to support back - don't bend at waist or neck when working at a low position - when seated, work at a comfortable height - don't wear high heels or platforms for too long - don't slump when seated - sit close to work - use a chair to support the back - sit with feet flat on the floor - sleep on a firm mattress (not hard) |
|
|
What is "range of movement" (ROM)? |
The maximum movement possible at a joint. |
|
|
What is active ROM? |
The movement of a joint through the entire ROM by the individual (by themselves). |
|
|
What is passive ROM? |
A nursing activity that involves moving a patient's joint. |
|
|
What should a nurse do if the patient says "it hurts" during passive ROM? |
The nurse should back off a little from the point of pain. |
|
|
Define abduction. |
Moving a limb away from the midline of the body. |
|
|
Define adduction. |
Moving a limb closer to the midline of the body. |
|
|
Define flexion. |
Bending, decreasing the joint (shortening the muscle). |
|
|
Define extension. |
Straightening, increasing the joint. |
|
|
Define Circumduction. |
Circular motion |
|
|
Define internal rotation. |
Turning toward the midline of the body (such as a club foot). |
|
|
Define supination. |
Turning upwards (as if holding a bowl of soup) |
|
|
Define pronation. |
Turning downwards (as if pouring the soup). |
|
|
What does a well-rounded exercise program include? |
Flexibility, resistance training & aerobic conditioning. |
|
|
How much exercise a week is recommended? |
150-300 minutes a week of moderate and vigorous exercise. |
|
|
What are benefits of exercise? |
- enhances the immune system - promotes weight loss - improves cardiovascular health - increases muscle tone and flexibility - decreases stress/ increases feeling of well-being |
|
|
What are the types of exercise? |
- isometric - isotonic - aerobic - anaerobic |
|
|
What is isometric exercise? |
Muscle contraction without motion (pushing on a wall). |
|
|
What is isotonic (isokinetic) exercise? |
Uses specialized equipment to give resistance to movement, such as rubber bands. |
|
|
What is aerobic exercise? |
Acquires energy from metabolic pathways that use oxygen, such as running or bicycling. |
|
|
What is anaerobic exercise? |
The amount of oxygen taken into the body does not meet the amount of oxygen needed to do activity. Examples include lifting barbells or sprinting. |
|
|
What are the risks associated with exercise? |
- cardiac injury (if not fit for exercise) - muscular skeletal injury (bones, joints, muscles) - dehydration - hyperthermia - hypothermia |
|
|
What are the factors that affect mobility? |
- Lifespan (developmental age) - nutrition (obesity) - Lifestyle - stress (causes fatigue) - external environment - disease |
|
|
What can bed rest do? |
One week of bed rest can decrease muscle strength 7 - 10%. |
|
|
What are the effects of immobility? |
- muscle atrophy - joint dysfunction - atelectasis or pneumonia - venous stasis (blood pooling in lower legs) - increased coagulability (risk for blood clot) - orthostatic hypotension - glucose intolerance |
|
|
What is orthostatic hypotension? |
Postural syncope. Blood pressure drops as person sits from lying position and stands from a sitting position. |
|
|
Name some more effects of immobility. |
- pressure ulcers - constipation - paralytic ileus - urinary tract infection - renal calculi - depression - sleep disturbances - disorientation |
|
|
What is paralytic ileus? |
Paralysis of the bowel |
|
|
What is renal calculi? |
Kidney Stones |
|
|
What does the nursing history assessment focus on? |
A patient's - height - weight - age - VS - BMI - joint function - gait - physical state |
|
|
Give examples of activity intolerance. |
- Shortness of breath - COPD |
|
|
What is an example of impaired physical mobility? |
A broken leg |
|
|
What are nursing interventions to promote exercise and mobility? |
1. overcoming objections to exercise 2. preventing injury from exercising 3. positioning the patient 4. moving the patient in the bed 5. transferring the patient out of bed 6. performing ROM 7. assisting with ambulation 8. daily stretching 9. plan and vary exercise routine 10. use buddy system and rewards 11. integrate exercise into routine activities 12. attain target heart rate |
|
|
What is a hand roll and what is it used for? |
A cloth rolled up and placed inside the hand of a bed-ridden patient to keep the hand from developing contractures. |
|
|
What is a trochanter roll and what is it used for? |
Sheets folded lengthwise and placed under a bed-ridden patient's hips to keep the patient in the correct position. |
|
|
What is Fowler's position and what is it used for? |
It is when the head of the bed is raised 45 to 60 degrees to allow a bed-ridden patient to eat or breathe better if there are breathing issues. |
|
|
What is lateral position and what is it used for? |
It is lying on the side with hip and knee flexed and in front of the body. Best for sleeping. |
|
|
What is prone position and what is it used for? |
Lying on the stomach, possibly used for surgical patients |
|
|
What is Sim's position and what is it used for? |
Semi-prone, used in rectal exams, tonsillectomies and mouth care on an unconscious patient. |
|
|
What is the supine position? |
On the back. |
|
|
What is orthopneic position and what is it used for? |
It is leaning forward on arms on a table in order to help cardiac or COPD patients to breathe better. |
|
|
What kinds of equipment can help a patient out of bed? |
- A transfer board - a mechanical lift - a transfer belt |
|
|
What is pertinent when helping a patient out of bed? |
- to lock the bed wheels and put the bed in it's lowest position - be sure the patient is wearing skid-resistant socks - be sure canes, walkers, crutches, etc. have rubber bottoms |
|
|
What is a log roll and what is it used for? |
A maneuver used to roll a patient in a way that will keep their spine in alignment. A sheet under the patient is used by hospital personnel. |
|
|
What is a sliding board? |
A board used to slide a patient from a stretcher to a bed. |
|
|
When using a cane, which side does the patient use it on? |
The stronger side so that the cane and the weaker side can be advanced at the same time. |
|
|
When a patient on crutches uses the stairs, how are the crutches to be used? |
They lead with the unaffected leg going up the stairs and lead with the affected leg going down the stairs. (The good go to heaven and the bad go to hell). |
|
|
Who uses a transfer board? |
Patients with chronic mobility problems. Helps to increase their independence. |
|
|
A patient is flexing her arm pulling against wrist restraints in bed. What kind of exercise is this? |
Isometric |
|
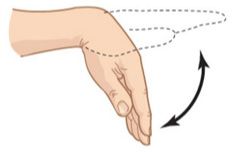
What is this picture an example of? |
Flexion |
|
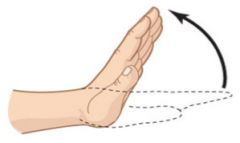
What is this picture an example of? |
Hyperextension |
|
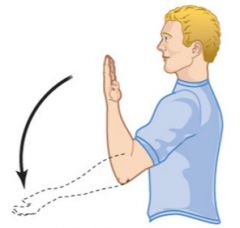
What is this an example of? |
Extension |
|

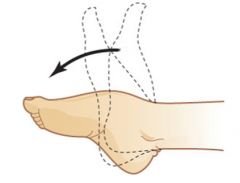
What is this an example of? |
Supination |
|
What is this an example of? |
Plantar flexion |
|
|
Of the following interventions for the client who is immobile, the nurse will give priority to Encouraging a diet high in fiber and extra fluids Administering the PRN medication for sleep Having the client use his incentive spirometer q2hrs Massaging the client’s legs every hour |
3. Having the client use his incentive spirometer q2hrs. It helps to prevent atelectasis. |
|
|
What is atelectasis? |
Incomplete lung expansion that can be caused by extended bed rest, bronchial obstruction or lack of breathing at birth. |
|
|
What is the difference between sleep and rest? |
With rest, the body is inactive with mild to no activity. With sleep, there is an altered consciousness that restores the body. Rest does not restore the body. |
|
|
Describe sleep. |
- basic physiological need - Cyclical states/altered consciousness - State of decreased motor activity/perception - Body slows, metabolism falls 20-30% - Selective response to external stimuli - Sleep restores the body |
|
|
Describe rest |
- Body is inactive with mild to no activity - Relaxation: stress-free, anxiety free - Leads to feeling refreshed (ex. reading, meditating, listening to music) |
|
|
What are the benefits of sleep? |
- Increasesmentalperformance Improves learning Helps the storage of long-term memory - Restores energy - Improves ability to cope - Strengthens the immune system |
|
|
Why is sleep so important? |
Long term sleep deprivation can result in stress-related illnesses & injuries (car accidents). Poor sleep even one night can reduce mental performance. |
|
|
How much sleep does a young adult (age 18-40 years) need? |
7-8 hours a day |
|
|
How much sleep does toddler need? |
12-14 hours a day |
|
|
How much sleep does an infant up to 4 months need? |
16-20 hours a day |
|
|
How much sleep does an elderly person need? |
5-7 hours a day |
|
|
What factors affect sleep? |
- age - lifestyle |
|
|
What lifestyle factors affect sleep? |
- work - physical activity (can help if 2 hrs before bed) - food - alcohol (causes sleep problems) - meds - nicotine & caffeine - an illness |
|
|
What environmental factors can affect sleep? |
- Temperature and humidity - Noise and light - No noxious odor - Comfort of bedding |
|
|
What part of the brain is responsible for maintaining wakefulness? |
The reticular formation |
|
|
How do the brain waves of a wakeful person differ from a sleeping person? |
In general the more rapid the brain waves the greater the brain activity |
|
|
What is a biorhythm? |
“biological clocks”: controlled in the body & synchronized with environmental factors like lightness & darkness and gravity |
|
|
What is a circadian rhythm? |
a biorhythm based on the day-night pattern in a 24hr period. |
|
|
What are the stages of sleep? |
NonREM REM |
|
|
Describe nonREM sleep (non-Rapid Eye Movement). |
- Also called slow wave sleep - Restful phase of sleep where physiological - function slows - 4 stages The stages are I, II, III & IV |
|
|
Describe REM sleep |
- Brain is highly active - brain waves similar to an awake & person occurs 90 minutes after the onset of sleep & after deep sleep IV - dreaming |
|
|
Name some sleep disorders. |
- Insomnia Most common sleep disorder - Circadian disorders: sleep/wake schedule - Sleep apnea |
|
|
What is sleep apnea? |
Stopping breathing while sleeping for approximately 10 seconds. |
|
|
What is the different between transient insomnia and chronic insomnia? |
Transient lasts less than a month and chronic lasts more than a month. |
|
|
What is narcolepsy? |
Uncontrollable episodes of sleep during the day (dangerous can come on while standing or driving car) |
|
|
What are parasomnias? |
Patterns of waking behavior that appear during sleep |
|
|
Name some parasomnias (five). |
- Sleepwalking/talking - REM sleep behavior disturbances: violently act out a dream - Enuresis: Bed wetting |
|
|
What medical conditions can cause secondary sleep disorders? |
- Depression - Hyperthyroid - hypothyroid - sleep apnea |
|
|
What medical conditions are worsened with sleep (five)? |
- CAD (coronary artery disease) - Asthma - COPD - Diabetes - ulcers |
|
|
What nursing interventions can promote sleep? |
- schedule nursing are around sleep times - create a comfortable, restful environment - promote relaxation - support bedtime rituals and routines - offer foods that promote sleep - maintain safety - teach about sleep hygiene - warm bath - teach about sleep-inducing meds |
|
|
What does maintenance of personal hygiene do for a person? |
- Promotes comfort |
|
|
What does ADL stand for? |
Activities of daily living. |
|
|
What is a nursing role for a patients ADLs? |
- Assess self-care abilities - Provide assistance with ADLs - Promote self-care in ADLs - Delegate appropriate parts of hygiene care |
|
|
When delegating hygiene care, what should be considered? |
- be certain the NAP has the capabilities - assess the patient's abilities and situation |
|
|
What factors influence hygiene? |
- psychosocial factors - personal preference - culture and religion - economic status - developmental level - knowledge level - physical factors (including cognitive & emotional) |
|
|
What is bathing a good opportunity for? |
Assessment of the integumentary system (the skin). |
|
|
What conditions should be watched for while bathing a patient? |
- colors of the skin - skin conditions |
|
|
What colors are to be examined during bathing? |
- pallor (pale) - erythema (redness) - jaundice (yellow discoloration) - Cyanosis (bluish color due to low oxygen) |
|
|
What conditions of the skin are to be examined during bathing? |
maceration Acne Excoriation Abrasion Pressure Ulcer Burns |
|
|
What is maceration? |
The softening of the skin due to prolonged exposure to moisture. |
|
|
What is excoriation? |
Areas where the skin has been scratched off due to rash or itchiness. |
|
|
What is a pressure ulcer? |
A bedsore or ulceration of the skin caused by poor circulation due to prolonged pressure on the body part, in particularly bony protuberances. |
|
|
What are the common types of baths? |
- assist bath - partial bath - bed bath |
|
|
What is an assist bath? |
The nurse only bathes the patient in areas the patient can't reach. |
|
|
What is a partial bath? |
The nursing bathing areas that are pertinent. Given when a complete bath is too stressful for the patient. |
|
|
What kinds of bed baths are there? |
- complete - partial - help All taken place in the bed |
|
|
What does oral care facilitate? |
Removal of food particles and secretions Improved appetite Assessment of client’s oral status Care of dentures |
|
|
When assessing the patient's oral status, what conditions should be watched for? |
- stomatitis - glossitis - oral lesions - malignancies - gingivitis |
|
|
When providing oral care for the unconscious patient, how should the nurse place the patient? |
Place the patient on his side with the head of the bed in a lowered position. |
|
|
When caring for a mustache or beard or shaving a client, what medication should we check for first? |
Coumadin |
|
|
With diabetics, what hygiene care areas should be given special care and why? |
The feet due to neuropathy. They cannot feel if there is a problem. |
|
|
The doctor ordered 250mg. of a medication. There are 500 mg in 5 mL. How many mL will you be giving the patient? |
Xml = 250mg/1 X 5/500mg = 250mg/1 X 1/100mg = 250/100 = 2.5mL |
|
|
Your patient weight 350 pounds. How many kilograms does he weigh? |
Xkg = 350lb/1 X 1/2.2kg = 350/2.2 = 159.1 Kg |
|
|
The doctor as asked you to administer 150mg to a patient of a medication. There are 1000mg per Liter. How many mL do you administer? |
XmL = 150mg X 1000mL/1000mg = 150mL (there are 1000mL in a L) |
|
|
How many mL in a teaspoon? |
Five |
|
|
How many pounds in a kilogram? |
Two and a half |
|
|
When administering oral liquids, which is the most accurate way? Dosing cup, oral syringes or droppers? |
Oral Syringes |
|
|
What does parenteral mean? |
A route other than the digestive system. |
|
|
Where can drugs be injected? |
• Intradermal (ID) = into the skin (TB test) • Intramuscular (IM) = into muscle (vaccines) |
|
|
What are the 3 parts of a syringe? |
1. Needle 2. barrel 3. plunger |
|
|
What sizes do syringes come in? |
Anywhere from 1mL to 60mL |
|
|
What are the 4 names a medication is given? |
1. Chemical name – hardly ever used 2. Generic (nonproprietary name) – Ex. ibuprofen 3. Official name – same as generic usually 4. Brand (trade, proprietary) name – Ex. Advil |
|
|
Which names of a medication are important to know? |
The brand name and generic name (ex. Tylenol and acetaminophen) |
|
|
How are controlled substances stored? (important to know) |
In a double locked drawer. Always behind two locks. |
|
|
What steps should be taken when administering a drug you're not familiar with? |
Look up the medication and consider why this may be given to your patient. |
|
|
What is pharmacokinetics? |
The study of how a medication moves through the body. |
|
|
What are the four processes in pharmacokinetics? |
- Absorption - Distribution - Metabolism - Excretion |
|
|
What are primary or therapeutic effects of medications? |
The intended effect of the medication, the desired, or palliative effect. |
|
|
What are secondary effects of medications? |
Unintended or non-therapeutic effects of medications, often referred to as side effects. |
|
|
Name some secondary effects of medications. |
- allergic reaction - upset stomach - constipation (as from narcotics) - drug interactions |
|
|
What is absorption? |
The movement of drug from the administration site into the bloodstream. |
|
|
What factors affect the rate of absorption? |
- The route of administation - pH of the blood - drug solubility - blood flow to the body areas - stomach contents |
|
|
What is distribution? |
Is the transportation of the drug to tissues and organs in the body (mainly by blood) |
|
|
What factors affect distribution? |
- local blood flow - membrane permeability - protein-binding capacity |
|
|
What is Metabolism? |
The chemical conversion of a medication into a form the body can excrete. |
|
|
What factors affect metabolism? |
- liver function - health or disease status - first-pass effect |
|
|
What is first-pass effect? |
The amount of drug lost in the process of absorption before it reaches the blood stream. Different medications have different first-pass effects. |
|
|
Where are drugs metabolized? |
- Kidneys - Liver - Lungs |
|
|
What is excretion? |
Elimination of the medication. |
|
|
Where are drugs excreted? |
- kidney - liver - lungs - exocrine glands |
|
|
What factor effects excretion? |
Organ function |
|
|
What are the 4 concepts related to pharmacokinetics? |
1. Time until onset and peak (important for insulin) 2. Therapeutic range/ level 3. half-life 4. concentration of the drug at the target site |
|
|
What is "half-life"? |
The time it takes for one half of the original amount of a drug to be removed from the body. |
|
|
What is a nurse to do is they don't understand an order or think it may be incorrect? |
Check with the medical provider that wrote the order. |
|
|
What types of medication orders are there? |
- Written order |
|
|
What are the components of a prescription? |
Client’s full name & address sometimes Date and time Name of medication Dosage size, frequency, number of doses Route of administration Printed name and signature of prescriber |
|
|
When preparing to administer a medication, how many times should a nurse check it and when? |
Three times: 1. Before it is mixed/poured or drawn up 2. after the medication is prepared 3. At the bedside |
|
|
What is important at the bedside when administering a medication? |
Watch the patient take the medication and do not leave it in the room. |
|
|
What are the six rights of a patient to keep in mind? |
The right patient The right drug The right dose The right time The right route The right documentation (Patients Do Drugs Timely, Routinely, Daily) |
|
|
What are three other rights of a patient? |
The right reason The right to know The right to refuse |
|
|
What is an MAR? |
Medication Administration Record |
|
|
What is the first thing a nurse should do should they commit a medication error? |
Assess the patient: vital signs, side effects, physical status. |
|
|
What do oral medications include? |
Tablets, pills, capsules Liquids Buccal: cheek Sublingual: under tongue Enteral medications: Nasogastric or Gastrostomy |
|
|
If a patient is vomiting, what is to be considered when administering medication? |
If it is to be given orally, see if there's another route that can be taken |
|
|
What is it when a medication is given buccal? |
It is to be dissolved against the inside of the cheek |
|
|
What is it when a medication is given sub-lingually? |
It is to be dissolved under the tongue |
|
|
What ways can a topical medication be given? |
- Lotions, creams, ointments - Transdermal patches |
|
|
What is the cartilage of the ear called and what do we do with it when administering ear drops? |
Pinna. It is pulled down when giving to a baby and pulled up when giving to an adult |
|
|
After administering an injection, what is important to remember when handling the needle? (important to know!) |
Never recap a used (dirty) needle |
|
|
Is it okay for a nurse to delegate medication administration? (important) |
No, a nurse is never to delegate medication administration. |
|
|
Who is Madeleine Leninger? |
She is the founder of transcultural nursing. She felt it important to understand a patient's culture and background to provide appropriate care. |

