![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
134 Cards in this Set
- Front
- Back
|
Tachycardia |
Faster heart rate - >100bpm |
|
|
Bradycardia |
Slower heart rate - <60bpm |
|
|
Paroxysmal AF |
Episodes >30 seconds but <7 days. Recurrent and self-terminating |
|
|
Persistent AF |
Episodes > 7 days, unlikely to self-terminate |
|
|
Permanent AF |
Fails to terminate with cardio version, or long term AF where cardioversion is not attempted |
|
|
Echocardiogram |
Ultrasound of heart to assess structure and function of heart and valves |
|
|
Chest X-Rays in AF |
Identify pulmonary problems that may cause AF e.g. COPD |
|
|
Thyrotoxicosis |
Excess of thyroid hormone. Can be underlying cause of AF |
|
|
Atrial fibrillation |
Disorganised, often fast rhythm from multiple foci within the atria. AV mode received more impulses than it can conduct - ineffective atrial contraction |
|
|
First line AF treatment |
Rate control: slow conduction through the AV mode to control ventricular rate. B-blockers (not sotalol) Rate-limiting CCBs (diltiazem is verapamil) Digoxin - only effective at rest, for sedentary patients with paroxysmal AF |
|
|
Life threatening AF presentation |
Emergency cardioversion without delaying to achieve anticoagulation |
|
|
Non-life threatening AF, onset <48hours or uncertain |
Rate control preferred. If cardioversion agreed - IV amiodarone (preferred for structural heart disease) or flecainide acetate Urgent rate control - IV B-blocker or verapamil |
|
|
Cardioversion |
Electrical (preferred >48hrs) - should be anticoagulated for at least 3 weeks or parenteral anticoagulation given and continued for 4 weeks. Or pharmacological - flecainide or amiodarone |
|
|
Rhythm control |
B-blockers (incl. sotalol) Amiodarone Dronaderone Pill-in-pocket |
|
|
Pill-in-pocket approach |
Oral flecainide or propafenone to self-treat episodes of AF when they occur. |
|
|
Class I antiarrythmics |
Disopyramide(IA) Lidocaine (IB) Flecainide acetate (IC) Propafenone (IC) |
|
|
Class III antiarrhythmics |
Amiodarone Dronaderone QT prolongation ! |
|
|
Other antiarrhythmics |
Adenosine - rapid reversion to sinus rhythm or radionuclide myocardial perfusion imagine Vernakalant- blocks K+ and Na+ channels in atria - rapid cardioversion Specialist hospital only |
|
|
CHA2DS2VASc |
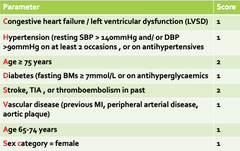
|
|
|
HAS-BLED |
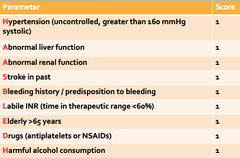
|
|
|
Choice of anticoagulants? |
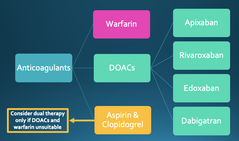
|
|
|
B-blocker use - first line |
Atenolol, acebutolol, metoprolol, nadolol, oxeprenalol and propanolol licensed. Bisoprolol off-label. Sotalol AMBER and not recommended first line. |
|
|
B-blocker side effects |
- Bradycardia - Masking hypoglycaemic symptoms - Masking thyrotoxicosis symptoms - Cold extremities - Sexual dysfunction - Nightmares - Fatigue |
|
|
B-blocker monitoring |
- Heart rate - BP - Side effects - Avoid in uncontrolled asthma: cardioselective may be initiated in secondary care |
|
|
What are the cardioselective B-blockers? |
Less effect on beta-2 receptors - less risk of bronchospasm Atenolol, bisoprolol, metoprolol, nebivolol, acebutolol (less so) |
|
|
B-blockers with long duration of action? |
Atenolol Bisoprolol Celiprolol Nadilol |
|
|
B-blockers: less bradycardia & coldness side effects? Why? |
Intrinsic sympathomimetic activity - partial agonist so less side effects. Celiprolol Pindilol Acebutolol Oxprenolol |
|
|
B-blockers with less sleep disturbance? |
Water soluble: less likely to cross BBB Atenolol Celiprolol Nadolol Sotalol Renal excretion - adjustments required Present in breast milk in greater amounts |
|
|
B-blocker - hypertension mode of action? |
- Reduce cardiac output - Alter baroreceptor reflex sensitivity - Block peripheral adrenoreceptors Some depress renin secretion. ** Effective at reducing BP but other classes more effective at reducing cardiovascular risk & therefore preferred. |
|
|
Phaeochromocytopenia: B-blockers |
B-blockers can be used for rate control, but never without concurrent alpha blockade. |
|
|
Dronedarone uses |
Less toxic but less efficacious than amiodarone Licensed for maintenance after sinus rhythm restored. Requires: >/1 of: hypertension, diabetes, previous stroke/embolism, > 70yrs or sufficient atrial diameter AND no left ventricular dysfunction or heart failure |
|
|
Dronedarone side effects |
Bradycardia Congestive heart failure Diarrhoea/GI disturbance Pulmonary toxicity - discontinue if dry cough/dysponea Livery injury - discontinue if 2 occurrences of ALT >3x Increased serum Cr QT prolongation |
|
|
Dronedarone monitoring |
Heart failure ECG 6 monthly Serum Cr baseline + 7/7. Repeated after 7/7 if raised LFTs - baseline, 7/7, monthly for 6/12, 3/12 for 6/12 then periodically |
|
|
Dronedarone cautions |
Cardiac disease including permanent AF Lung/liver issues with previous Amiodarone |
|
|
Amiodarone Multiple MOA Who can initiate? |
Slows conduction through AV node and prolongs cardiac action potential AMBER drug |
|
|
Amiodarone loading dose
|
Long half life 200mg TDS 7/7 200mg BD 7/7 200mg OD continued |
|
|
Amiodarone side effects |
GI disturbance Taste alteration Pulmonary toxicity Thyroid dysfunction Photosensitivity Hepato-bilary disorders Corneal deposits Neurological symptoms Cardiac toxicity |
|
|
Amiodarone monitoring |
HR Liver function - before & 6mthly Thyroid function - before & 6mthly U&Es - potassium Chest x-ray - before |
|
|
Amiodarone caution/CI |
Conduction disturbances QT prolongation Elderly Hypokalaemia Bradycardia Thyroid disease |
|
|
Amiodarone STOPP criteria |
First-line therapy in supraventricular arrhythmias Higher risk of side effects than B-blockers, digoxin, verapamil or diltiazem |
|
|
Cardiac catheter ablation |
Catheter threaded through groin via vena cava Tip destroys tissue generating the inappropriate APs - non-conductive so pathway is blocked. |
|
|
Sotalol hydrochloride indications |
- ventricular tachyarrhythmias - Prophylaxis of paroxysmal atrial tachycardia/AF - Maintenance of sinus rhythm following cardio version of atrial flutter |
|
|
Sotalol contraindications |
QT prolongation - avoid hypokalaemia and hype-magnesia. Torsade de pointes |
|
|
Sotalol monitoring |
Corrected QT interval ECG U&Es |
|
|
Digoxin use |
Cardiac glycoside - increases force of myocardial contraction and reduces AV node conductivity Ventricular rate control in sedentary patients or in combination Rarely for rapid control |
|
|
Digoxin therapeutic window |
1.5-3mcg/L Regular monitoring is not required unless toxicity is suspected Hypokalaemia increases risk - may be managed with potassium-sparing diuretic or supplementation |
|
|
Digoxin toxicity |
Life threatening arrhythmia can be managed by digoxin-specific antibody fragments when unresponsive to atropine and beyond the control of withdrawal + electrolyte correction |
|
|
Digoxin STOPP criteria |
- In heart failure with normal systolic ventricular function (no clear benefit) - Long term dose >125mcg daily if eGFR <30ml/min (risk of toxicity) |
|
|
Digoxin contraindications |
Constrictive pericarditis Hypertropic cardiomyopathy Heart block Myocarditis Supraventricular arrhythmias associated with accessory conducting pathways e.g. Wolff-Parkinson-White syndrome |
|
|
Digoxin cautions |
Hypercalcaemia Hypokalaemia Recent MI Severe respiratory disease Sick sinus syndrome Thyroid disease |
|
|
Digoxin monitoring |
Concentration-assay taken at least 6 hours post dose U&Es - renal function and electrolytes may increase toxicity |
|
|
Digoxin elixir use (2 points) |
Patients must be counselled to use the graduated pipette supplied for all doses Must not be diluted |
|
|
Digoxin side effects |
Arrhythmias Cardiac conduction disorder Cerebral impairment Diarrhoea Dizziness Eosinophilia Vision disorders Skin reactions Nausea/vomiting |
|
|
Antifibrinolytic for menorrhagia |
Tranaxemic acid - up to 4 days use, once menstruation has started |
|
|
Von Willebrand's disease |
Genetic disorder caused by missing or defective von Willebrand factor (VWF), a clotting protein. VWF binds factor VIII, a key clotting protein, and platelets in blood vessel walls, which form a platelet plug during the clotting process. Treated with coagulation factors. |
|
|
Patients at risk of venous thromboembolism |
Substantial reduction in mobility (>3 days) Obesity Malignant disease History of VTE Thrombophilic disorder Over 60 years Pregnancy/post partum |
|
|
Mechanical thromboprophylaxis |
Anti-embolism stockings (14-15mmHg) Worn day and night until mobile. - Not for acute stroke or peripheral artery disease, severe leg oedema or local conditions OR Intermittent pneumatic compression |
|
|
Pharmacological prophylaxis initiation |
Within 14 hours of admission |
|
|
High risk of VTE in patients with anticoagulant therapy |
Offer prophylaxis if anticoagulant therapy interrupted |
|
|
VTE prophylaxis in major trauma or surgery (not orthopaedic or general) |
Offer mechanical prophylaxis, continue until sufficiently mobile or discharged from hospital. - 30 days if undergoing spinal or cranial surgery |
|
|
Pharmacological VTE prophylaxis in renal impairment |
Unfractionated heparin preferred |
|
|
Preferred pharmacological VTE prophylaxis in abdominal, bariatric, thoracic or cardiac surgery |
Fondaparinux |
|
|
Preferred pharmacological VTE prophylaxis in lower limb immobilisation or pelvis/hip/femur fracture |
Fondiparinux |
|
|
Length of pharmacological prophylaxis in spinal surgery |
30 days |
|
|
Length of pharmacological prophylaxis in general surgery |
7 days (or until mobile) |
|
|
Length of pharmacological prophylaxis in major cancer surgery in abdomen |
28 days |
|
|
When is intermittent pneumatic compression considered for major trauma? |
Pharmacological prophylaxis is contraindicated |
|
|
Elective hip replacement VTE regimen |
LMWH for 10/7 Aspirin for 28 days OR LMWH for 28/7 with compression stockings OR Rivaroxaban (dabigatran/apixaban alternatives) |
|
|
Elective knee replacement VTE regimen |
Aspirin for 14/7 OR LMWH 14/7 with compression stockings OR Rivaroxaban/apixaban/dabigatran |
|
|
VTE prophylaxis in acutely ill medical patients |
LMWH for minimum of 7/7 Fondaparinux as alternative Renal impairment: LMWH or heparin |
|
|
Acute stroke patients at risk of VTE? |
Mechanical with intermittent pneumatic compression within 3/7, continued for 30/7 or until mobile |
|
|
Thromboprophylaxis in pregnancy - birth or miscarrage/termination in last 6/52 WITH risk factors |
LMWH during hospital admission, until risk of VTE has passed. Start 4-8hrs after event and continue for minimum 7/7. Additional mechanical for those with significantly reduced mobility - Intermittent first line |
|
|
First line mechanical prophylaxis in pregnancy |
Intermittent pneumatic compression |
|
|
Edoxaban |
Oral treatment and prophylaxis of VTE. Should not be used in pulmonary embolism, haemodynamic instability or pulmonary embolectomy. |
|
|
Initial treatment of DVT |
LMWH/heparin as IV loading dose, followed by continuous infusion, or intermittent SC. Oral anticoagulant (usually warfarin) started at the same time as heparin. Heparin continues for at least 5 days or until INR >/=2 for 24hrs. Monitoring for APTT essential |
|
|
Intermittent IV heparin for DVT treatment |
Not recommended |
|
|
Heparin monitoring |
Activated partial thromboplastin time (APTT) |
|
|
Treatment of DVT in pregnancy |
Heparins do not cross placenta LMWH preferred as lower risk of osteoporosis and heparin-induced thrombocytopenia ** eliminated more rapidly in pregnancy so dosing needs to be adjusted |
|
|
LMWH antidote |
Protamine sulfate (partially reverses effects) |
|
|
TIA immediate treatment |
Aspirin 300mg OD until cause established |
|
|
Initial ischaemic stroke management |
Alteplase (within 4.5hrs) Aspirin (+ PPI if required) |
|
|
Are anticoagulants recommended in ischaemic stroke? |
Not if in sinus rhythm. Aspirin must be given for 2/52 before starting ACs with AF. Parenteral ACs may be used in those at high risk of developing DVT or PE. |
|
|
When should warfarin be used in ischaemic stroke? |
Not until AFTER acute phase. |
|
|
Risk of haemorrhagic transformation in ischaemic stroke? |
Anticoagulants - stop for 7 days and substitute with aspirin |
|
|
Hypertension treatment in ischaemic stroke |
Do not treat ! Reduced cerebral perfusion so should only be initiated in event of hypertensive crisis |
|
|
Long-term ischaemic stroke management |
Clopidogrel (or dipyridamole MR + aspirin) Or mono therapy with either if CI'd. Review for long-term anticoagulation if AF High intensity statin (regardless of cholesterol) BP control Lifestyle modification |
|
|
Blood pressure target following stroke |
<130/80mmHg |
|
|
B-blockers in ischaemic stroke |
Not recommended unless for co-existing condition. |
|
|
Intercranial haemorrhage initial treatment |
Surgical intervention to remove haematoma OR Rapid BP lowering if 150-200mmHg to 130-140mmHg within 1 hour of treatment for >7/7. |
|
|
When should rapid BP lowering not be used for haemorrhagic stroke? |
- Underlying structural cause - GCS <6 - Early neurosurgery to excavate the haematoma |
|
|
PE/DVT in haemorrhagic stroke? |
Anticoagulants or caval filter |
|
|
Long-term management of haemorrhagic stroke |
Aspirin and clopidogrel not recommended routinely. Those with CV risk need specialist advice. BP treatment and monitoring, care to avoid hypoperfusion - Statins not recommended unless CV risk outweighs risk of future haemorrhage |
|
|
Anticoagulant uses? |
To prevent thrombus formation (or extension) in the slower-moving venous side. Less use preventing thrombus in arteries as composed of mainly platelets with little thrombin. |
|
|
Vitamin K antagonists |
Warfarin, acenocoumarol and phenindione |
|
|
Vitamin K antagonists - time to anticoagulation |
48-72 hours |
|
|
LMWH/heparin - time to anticoagulation |
Immediate |
|
|
Cerebral thrombosis or peripheral artery occlusion |
Aspirin. Warfarin not recommended. |
|
|
VTE prophylaxis in warfarin patients |
Unfractionated heparin preferred, warfarin may be continued in select patients undergoing surgery and at high risk. |
|
|
Initiating warfarin |
Baseline prothrombin time needed but initial dose should not be delayed while waiting. |
|
|
INR target guidelines |
British Society for Haematology |
|
|
Threshold for warfarin dose adjustment |
Within 0.5 of INR target value |
|
|
INR target 2.5 for... |
- DVT treatment - Myocardial infarction - AF - Cardioversion (at least 3 weeks before + 4 weeks after) - Dilated cardiomyopathy - Mitral stenosis or regurgitation in AF - Bioprosthetic valves in mitral position - Acute arterial embolism |
|
|
INR target 3.5 for... |
- Recurrent DVT or PE in those with INR >2 - Mechanical prothetic heart valves (depends on type and location of the valve) |
|
|
Warfarin duration recommendations |
6/52 - isolated calf vein DVT 3/12 - VTE provoked by surgery or risk factor at least 3/12 - unprovoked proximal DVT or PE |
|
|
Major bleeding with warfarin |
Stop warfarin and give phytomenadione (Vitamin K1) by slow IV injection, dried prothrombin complex or fresh frozen plasma |
|
|
Minor bleeding with INR >8.0 |
Stop warfarin and give vitamin K by slow injection - repeat after 24hrs if still high. Restart warfarin when INR <5.0 |
|
|
No bleeding with INR >8.0 |
Stop warfarin and give vitamin K by slow injection - repeat after 24hrs if still high.Restart warfarin when INR <5.0 |
|
|
Minor bleeding with INR 5.0-8.0 |
Stop warfarin and give vitamin K by slow injection. Restart warfarin when INR <5.0 |
|
|
No bleeding with INR 5.0-8.0 |
Omit 1 or 2 warfarin doses and reduce subsequent maintenance dose |
|
|
Unexpected bleeding with INR in range |
Investigate underlying causes e.g. renal or GI pathology |
|
|
When should warfarin be stopped prior to elective surgery? |
5 days before.
If INR </=1.5 then give oral vitamin K |
|
|
When can warfarin be restarted following surgery? |
If haemastasis adequate - restart normal dose in evening or next day. |
|
|
When is warfarin bridging required? |
If at high risk of VTE: - Previous event within 3/12 - AF with previous stroke or TIA - Mitral heart valve |
|
|
Warfarin bridging regimen timings? |
LMWH at treatment dose given, stopped at least 24 hours before surgery. If high risk of bleeding the LMWH should not be restarted until at least 48hrs after. |
|
|
Emergency surgery in patients on warfarin |
If able to be delayed for 6-12 hours - give IV vitamin K. If not, give dried prothrombin complex in addition and check INR pre-surgery. |
|
|
Combined anticoagulant and anti platelet therapy |
Add warfarin when indicated (e.g. VTE or AF) after risks of bleeding established and discussed with cardiologist. Aspirin + warfarin/aspirin with clopidogrel + warfarin must be kept to minimum. Many be possible to withdraw anti platelet until warfarin therapy is complete to reduce time spent. |
|
|
Why use heparin over LMWH? |
Short duration of action. Initiates therapy or used in those at high risk of bleeding as effect terminated rapidly after withdrawal. |
|
|
LMWHs? |
Dalteparin Enoxaparin Tinzaparin |
|
|
Why are LMWH preferred over heparin? |
Lower risk of heparin induced thrombocytopenia. Does not required monitoring Once daily administration in some indications |
|
|
Danzeparinoid |
Heparinoid used for prophylaxis of DVT in general/orthopaedic surgery. Has a role in heparin-induced thrombocytopenia (when no evidence of cross-sensitivity) |
|
|
Argatroban |
Oral anticoagulant can be given once thrombocytopenia has resolved |
|
|
Hirudins |
Bivalirudin Thrombin inhibitor for unable angina/NSTEMI AND an anticoagulant for percutaneous coronary intervention (STEMI included) |
|
|
Epoprostenol MOA & licensing |
Inhibits platelet aggregation during renal dialysis when heparins unsuitable. Licensed for primary pulmonary hypertension. Potent vasodilator. |
|
|
Fondaparinux MOA? |
Inhibites activated Factor X |
|
|
How is epoprostenol given? |
Half life of 3 minutes so must be given as continuous IV infusion |
|
|
Rivaroxaban and apixaban specific antidote? |
Andexanet alfa - Recombinant of Factor X, reverses effects (£11,000/4 vials) |
|
|
Dabigatran antidote? |
Idarucizumab MAb that binds specifically to dabigatran and metabolites |
|
|
Indication for long term aspirin? |
Secondary prevention only. (With established CV disease) Primary prevention not recommended. |
|
|
High risk of GI bleeding on aspirin? |
Give PPI |
|
|
NSTEMI clopidogrel? |
Aspirin + clopidogrel for 3/12. Increases risk of bleeding. |
|
|
STEMI clopidogrel? |
Aspirin + clopidogrel for up to 4/52. Increases risk of bleeding. |
|
|
ACE inhibitors contraindication |
In combination with aliskiren in patients with <60ml/min eGFR or diabetes melatus |
|
|
ACE inhibitors contraindication |
In combination with aliskiren in patients with <60ml/min eGFR or diabetes melatus |
|
|
ACE inhibitor general cautions |
Afro-Caribbean patients (may respond less) Concomitant diuretics |

