![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
351 Cards in this Set
- Front
- Back
|
What are the 3 major structural molecules in cells formed by?
|
Fat, protein and carbohydrate
|
|
|
What 4 molecules are essential for the functioning of cells?
|
Fat, protein, carbohydrates and nucleic acid
|
|
|
What is the sub-unit of nucelic acid?
|
Pentose sugars
|
|
|
What is nucleic acid used for in cells?
|
Synthesising DNA; it is also used by mRNA and tRNA for transcription
|
|
|
What is the sub-unit of proteins?
|
Amino acids
|
|
|
What is protein used for in cells?
|
To synthesize other proteins such as enzymes and hormones. It is also used to build up muscles for movement.
|
|
|
What is the sub-unit of carbohydrates?
|
Monosaccharides
|
|
|
What are carbohydrates used for in cells?
|
As energy (glucose) and for storage (as glycogen in the liver)
Can also be used as structure ( cellulose) |
|
|
What are the sub-units for lipids?
|
Glycerol and fatty acids
|
|
|
What are lipids used for in cells?
|
Plasma Membranes
|
|
|
What two features do eukaryotic cells have that prokaryotic cells do not have?
|
Membrane bounded organelles.
Distinct nucleus |
|
|
Name 3 examples of eukaryotic cells
|
Fungi, animals and plants
|
|
|
In which organelle would you find the cristae?
|
Mitochondria
|
|
|
In which organelle would you find cisternae?
|
Endoplasmic Reticulum
|
|
|
What is chromatin and where is it found?
|
Uncondensed DNA (in diffuse form) within the nucleoplasm in the nucleus
|
|
|
Name two organelles with a double membrane
|
Nucleus and mitochondria
|
|
|
Where will you find ribosomes in an eukaryotic cell?
|
Some will be free in the cytoplasm but most are studded on the RER.
|
|
|
What does the word "lysis" mean and what has this got to do with lysosomes?
|
Lysis=to break
Lysosomes are vesicles which contain enzymes in order to break down pathogens,or, dead or worn down organelles. |
|
|
What is the matrix, its consistency and where is it found?
|
Found in the mitochondria it is a semi-rigid material which contains proteins, lipids, enzymes and traces of DNA
|
|
|
What is the singular of mitochondria?
|
Mitochondrion
|
|
|
What is the consistency of the nucleoplasm?
|
A granular, jelly-like substance
|
|
|
What large molecules do the nuclear pores in the nucleus let through?
|
mRNA for transcription
|
|
|
At process causes epithelial cells to use a lot of energy whilst absorbing substances from the intestine?
|
Active transport
|
|
|
What is the nuclear envelope continuous with?
|
ER
|
|
|
What is the position and the function of the nucleolus?
|
In the centre of the nucleus, within the nucleoplasm it manufactures rRNA and assembles ribosomes
|
|
|
Where are the enzymes involved in respiration found?
|
The matrix in the mitochondria
|
|
|
Why does the cristae need a large surface area?
|
So that more enzymes can attach themselves onto it for respiration
|
|
|
What are the flattened sacs on the ER and Golgi Apparatus called?
|
Cisternae
|
|
|
What is the main function of the RER?
|
To synthesise and transport proteins
|
|
|
What is the main function of the SER?
|
To synthesise, store and transport lipids and carbohydrates
|
|
|
What cells will need an extensive number of mitochondria?
|
Muscle and epithelial cells
|
|
|
What cells will need an extensive ER system?
|
Liver and epithelial cells
|
|
|
What does the Golgi Apparatus modify?
|
Lipids and proteins (by adding carbohydrates to form glycoproteins)
|
|
|
What does the Golgi Apparatus secrete?
|
Carbohydrates such as cellulose
|
|
|
How are the proteins and lipids produced in the ER passed through to the Golgi Apparatus?
|
In strict sequence
|
|
|
Once sorted, how are the modified proteins and lipids transported from the Golgi Apparatus?
|
Vesicles
|
|
|
What do vesicles do?
|
Transport the non-harmful molecule to the cell membrane where it will fuse and thus release its contents to the outside
|
|
|
What does the Golgi Apparatus produce and so in which cells are they well developed with GA?
|
Secretory enzymes, and so it is popular in secretory cells
|
|
|
What is exocytosis and autolysis, and what does this?
|
The lysosomes release substances to the outside (exocytosis) and break down cells which have died (autolysis).
|
|
|
What are the two types of ribosomes and where would you find them?
|
80S - in eukaryotic cells
70S - in prokaryotic cells, slightly smaller |
|
|
What is the ribosomes' structure and function?
|
Its assembly consists of a large sub-unit and a small sub-unit. They are made of rRNA and protein.
It is where protein synthesis occurs |
|
|
When the cell membrane folds what is formed? What is its function relating to structure?
|
Microvilli; hair-like structures which increase surface area for efficient absorption.
|
|
|
Why does the RER have a large surface area?
|
So that more ribosomes can attach themselves onto it
|
|
|
What do lysosomes do to worn out organelles and why?
|
They digest them so that they can can re-use the useful materials they are made from
|
|
|
Whatbdo lysosomes do to dead cells?
|
Completely break them down
|
|
|
In what cells are lysosomes popular?
|
Secretary, epithelial and phagocytic
|
|
|
For a microorganism to be considered a pathogen it must.. (4)
|
Gain entry
Colonise tissues Resist defences Cause damage to tissues |
|
|
How do organisms get into the body?
|
Penetrating one of the organism's interfaces with the environment
|
|
|
What properties does our skin have to stop organisms getting into the body?
|
Thick
Keratin layer Continuous Physical barrier |
|
|
When does an invasion occur via skin?
|
When cut or through insect bites
|
|
|
Key features of how interfaces have evolved to allow exchange of material
|
Thin, permeable
Moist Large surface area Well supplied with blood vessels |
|
|
How does a mucous layer prevent the entry of pathogens?
|
Traps microorganisms
Thick, sticky barrier which is harder to penetrate |
|
|
How do enzymes prevent entry of microorganisms?
|
Break down pathogens
Denature proteins in enzyme causing a change of 3D shape |
|
|
Two main ways in which pathogens cause disease
|
Damaging tissues
Producing toxins |
|
|
How can a pathogen damage tissue? (3)
|
Sheer number of pathogens causes the cell to burst/not be able to function.
The virus replicates itself until the host cell burst, releasing the virus into the bloodstream -infecting new cells. Viruses inhibit synthesis of DNA,RNA and proteins in cell Break down membranes of cell, rupturing it so that all of its nutrients are released -starving it. |
|
|
The time taken for a pathogen to cause damage depends on
|
How quickly it divides
|
|
|
Lifestyle factors which contribute to cancer
|
Smoking
High fat, high salt, high alcohol, low antioxidants, low fibre, low fruits and vegetables diet Overweight Little exercise High exposure to sunlight -UV radiation |
|
|
How to lower blood pressure
|
Stress less
Exercise more Avoid obesity Eat less salt |
|
|
How to lower blood cholesterol levels
|
Fewer saturated fatty acids
|
|
|
BMI which brings increased risk of CHD
|
25
|
|
|
Function of phagocytes
|
Enulf pathogens through phagocytosis
|
|
|
Type of microorganism of influenza
|
Virus
|
|
|
Type of microorganism of chickenpox
|
Virus
|
|
|
Type of microorganism of mumps
|
Virus
|
|
|
Type of microorganism of food poisoning
|
Bacterium
|
|
|
Type of microorganism of whooping cough
|
Bacterium
|
|
|
Type of microorganism of tuberculosis
|
Bacterium
|
|
|
Type of microorganism of athlete's foot
|
Fungus
|
|
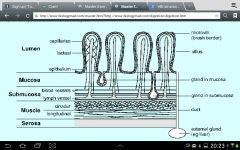
Describe function of the five layers
|
Lumen- space in gut, layer of epithelia cells
Mucosa- secrete mucus and absorbs digested food Submucosa -controls the cell using blood vessels and lymph vessels Muscle - maintains concentration gradient inside lumen by contracting. Circular = squeeze. Longitudinal = shortens. Serosa -holds gut together |
|
|
What is the structure inside one villus and how do they help in its function?
|
Good network of capillaries to transport absorbed molecules to cells
Lacteal transports fatty substances Layer of one cell thick epithelia cells = short diffusion path Microvilli = brush border increases surface are for absorption. |
|
|
Describe structure and function of oesophagus
|
Transports food from mouth to stomach
Thick muscular wall |
|
|
Structure and function of stomach
|
Muscular sac filled with gastric juices which contain trypsin and hydrochloric acid.
Goblet cells secrete mucus to help reduce friction and also prevent the enzymes digesting the stomach. |
|
|
Describe structure and function of large intestine
|
Absorbs water ( and electrolytes) and so causes the chyme to become drier and thicker = faeces
|
|
|
Structure and function of rectum
|
Final section of intestines
Stores faeces before being egested through anus |
|
|
Structure and function of salivary glands
|
Secretes saliva through duct containing amylase to break down starch into maltose. Also contains mucin used to bind food together.
|
|
|
Quaternary structure of proteins
|
Combination of different polypeptide chains associated with non-protein (prosthetic) groups
|
|
|
Position, structure and function of pancreas
|
Below stomach
Secretes lipases, proteases and carbohydrases such as amylase = pancreatic juice |
|
|
Examples of physical breakdown of food in body
|
Mastication = teeth
Stomach muscles churn up food to mix all the contents in gastric juices and also break it up. |
|
|
What is the point of breaking down food
|
Smaller, soluble pieces = larger surface area for chemical digestion (hydrolysis) to take place
Can pass through cell surface membranes |
|
|
General formula of monosaccharides
|
CnH2nOn
|
|
|
Formula of glucose
|
C6H12O6
|
|
|
Examples of reducing sugars
|
All monosaccharides
Maltose Can donate electrons |
|
|
What is Benedict's reagent?
|
Alkaline solution of copper sulfate
|
|
|
What happens to Benedict's reagent when heated with a reducing sugar?
|
Insoluble brick-red precipitate of copper oxide
|
|
|
How to test for a reducing sugar
|
Add equal volume of benedict's reagent
Heat in water bath Turns brick-red |
|
|
Sample in tests must be solid or
|
Ground up
|
|
|
Maltose =
|
Alpha glucose + alpha glucose
|
|
|
Sucrose =
|
Alpha glucose + fructose
|
|
|
Lactose =
|
Beta glucose + galactose
|
|
|
How do monosaccharides join?
|
Condensation reaction - gives out water
Glycosidic bond |
|
|
How to break down disaccharides
|
Hydrolysis - add water
|
|
|
How to test for non reducing sugars
|
When hested up with benedict's reagent initially solution remains blue.
Add equal volume of dilute hydrochloric acid Add enough sodium hydrogencarbonate until ph is 7 Test with ph paper Retest solution with benedict's reagent and heat in a water bath Now should turn brick-red |
|
|
What is the pont of adding hydrochloric acid to test for a non reducing sugar?
|
Hydrolyses sample into constituent monosaccharides which are all reducing sugars
|
|
|
What is the point of adding sodium hydrogencarbonate to test for non reducing sugars?
|
Return ph of solution back to neutral as test will not work in acidic conditions
|
|
|
How to test for starch
|
Add equal volume of iodine (potassium iodide)
Shake/stir Iodine turns from yellow to blue-black |
|
|
How does the stomach prevent further hydrolysis of starch?
|
Acidic environment in stomach denatures amylase enzyme inhibiting its effects.
|
|
|
Why does the pancreas need to have a neutral ph and how does it do this?
|
Alkaline salts produced so that amylase can work to hydrolyse starch.
|
|
|
How is the saliva's ph maintained and why does it do this?
|
Mineral salts produced so that amylase can work to hydrolyse starch into maltose
|
|
|
What enzyme does the epithelial cell of the small intestine produce?
|
Maltase which breaks down maltose through hydrolysisinto alpha glucose + alpha glucose
|
|
|
Describe lactose intolerance in terms of water potential
|
Unhydrolysed lactose = soluble, remains in lumen. This reduces the lumen's water potential meaning that water moves from the epithelial cells out into the lumen from an area of higher water potential to an area of lower water potential
|
|
|
Magnification =
|
Image/object
|
|
|
How do people develop lactose intolerance?
|
Production of lactase diminishes after childhood
Insufficient amount of lactase in ratio to lactose ingested. |
|
|
How does lactose intolerance cause bloating?
|
Undigested lactose ferments in large intestine producing large volumes of gas
|
|
|
How can you live with lactose intolerance?
|
Drink milk with added lactase
Or do not drink any milk at all but keep up with vitamin D and calcium requirements |
|
|
What are the four groups attached to the central carbon in a protein?
|
Amino group (NH2)
Carboxyl group (COOH) Hydrogen group (H) R group (variety of different chemical groups) |
|
|
How can you form a dipeptide?
|
Join two amino acid monomers through a condensation reaction to form a peptide bond.
Carboxyl group from one amino acid joins with a hydrogen group of another amino acid to form water |
|
|
What is polymerisation?
|
Series of condensation reactions joining many amino acids together to form a polypeptide.
|
|
|
Where does variety in an amino acid come from?
|
R group
|
|
|
Where do hydrogen bonds in proteins form and why?
|
Hydrogen from amino group (now only NH as the other H has been used during condensation reaction) bonds with O from carbonyl group (used to be carboxyl group but OH used in condensation reaction)
Hydrogen= + Oxygen = - |
|
|
Primary structure of proteins
|
Sequence of amino acids
|
|
|
Secondary structure of proteins
|
Alpha helix
Beta pleated sheet Hydrogen bonds twist polypeptide into different 3D shapes |
|
|
Tertiary structure of proteins
|
Alpha helix or beta pleated sheet are twisted more which creates an original 3D shape with is maintained by:
Disulfide bonds Hydrogen bonds Ionic bonds |
|
|
Strength order of bonds in tertiary structure of proteins
|
Disulfide bonds are strongest = covalent
Ionic = quite strong but influenced by changes in ph Hydrogen bonds = numerous but weak |
|
|
Where do ionic bonds in proteins' tertiary structure form?
|
Carboxyl and amino groups which have not already been involved in condensation reactions
|
|
|
How to test for proteins
|
Add an equal volume of biuret's reagant
Turns purple = indicates the presence of peptide bonds Maintains blue = no peptide bonds present |
|
|
Example and function of fibrous proteins
|
Collagen
Structural |
|
|
Example and function of globular proteins
|
Enzymes
Metabollic functions |
|
|
Structure of collagen
|
Fibrous protein
Long chains - parallel, with cross links Three quaternary chain fibres wound together |
|
|
Lock and key theory limitation
|
Enzyme is thought as rigid
|
|
|
Why does an enzyme's active site bind to a substrate?
|
They have a complementary shape and with the sufficent activation energy they will bind.
|
|
|
Enzyme + substrate =
|
Enzyme-substrate complex
|
|
|
Enzyme-substrate complex --->
|
Enzyme + product
Enzyme is not used up in reaction |
|
|
Describe the induced fit model
|
Enzyme is considered flexible and moulds around substrate.
As the enzyme changes shape, it puts strain on the molecule, weaking and distorting the bonds within the substate. As a result, this lowers its activation energy |
|
|
How can you the measure the rate of enzyme-catalysed reactions
|
Formation of products
Disappearance of substrate |
|
|
What problem may be caused by an increase of product in an enzyme-catalysed reaction?
|
Increase in product, decrease in substrate - product may get in the way of remaining substrate molecules to bind to an active site causing a decrease in rate.
|
|
|
What do competitive inhibitors bind to?
|
Active site of enzyme
|
|
|
What do non-competitive inhibitors bind to?
|
Allosteric site of enzyme
|
|
|
How does a competitive inhibitor reduce the enzyme's activity?
|
Inhibitor binds to active site of enzyme
This blocks substrate from bonding to the enzyme meaning that fewer enzyme-substrate complexes are formed, meaning that there is less product - reduces the rate of reaction. |
|
|
How can you reduce the effect of a competitive inhibitor? Why does this happen??
|
Increase substrate concentration
Inhibitor is not permanently boud to enzyme and so when it leaves a substrate can take its space if there is a plentiful supply of them The greater the concentration of inhibitor, the slower it takes for an increase in substrate to have an effect |
|
|
How does a non-competitive inhibitor reduce enzyme activity?
|
Inhibitor binds to allosteric site of enzyme
As it does so, the enzyme's active site is changed meaning that no substrates can bind to the enzyme to form enzyme-substarte complexes, and thus form product. This reduces the rate of reaction. |
|
|
How can you decrease the effect of a non-competitive inhibitor?
|
You can't
After the inhibitor changes the active site of the enzyme, substrate still fit but do not fully bind. As a result, an increase in substarte has no effect on the inhibitor asbthey are not competing for the same site. |
|
|
What is a metabolic pathway?
|
Series of reactions where each step is catalysed by an enzyme
|
|
|
What is end-product inhibition?
Why is it needed? |
When the end product inhibits enzyme A if there is a oversupply of end product (you don't want to waste energy).
If there is not enough end product there will be less to i hibit enzyme A and so its level will return to normal. Usually non-competitive |
|
|
Millimetre equivalent in metres
|
10^-3
|
|
|
Micrometre equivalent in metres
|
10^-6
|
|
|
Nanometre equivalent in metres
|
10^-9
|
|
|
3 features of solution needed for cell fractionation. Why?
|
Cold- reduce enzyme activity (like those which may have been released by broken lysosomes) as they may otherwise break down the organelles
Isotonic - reduce osmotic gain or loss of water so that the organelles remain the same size ( do not burst or shrink) Buffered - to maintain a constant ph so that there is no denaturing. |
|
|
What is the feature of the isotonic solution needed for cell fractionation?
|
Has same water potential as original tissue
|
|
|
What is the point of homogenation?
|
Splitting open cells to release organelles from cell
Produce homogenate where everything is equally mixed |
|
|
Why is the homogenate filtered in cell fractionation?
|
To remove any whole cells or large pieces of debris
|
|
|
What machine is used for cell fractionation? How does it work?
|
Ultracentrifuge.
Spins filtered homogenate at a high speed to create a centrifugal force |
|
|
Describe process of ultracentrifugation
|
Filtrate placed in ultracentrifuge
Spun at low speed Organelle with heaviest mass (nucleus) forms as a pellet on bottom Supernatant removed and spun again at a higher speed The next heaviest organelles (mitochondria) form as a pellet |
|
|
Advantage of cell fractionation
|
Allowed scientists to isolate organelles to create a detailed study of structure and function of organelles.
|
|
|
In which substances are lipids soluble/insoluble?
|
Water = insoluble
Alcohols/Acetone = soluble |
|
|
Why are lipids a good source of energy
|
Provide more than twice the amount of energy produced by carbs
|
|
|
Why do plants and mammals have wax/oil cover/secretion
|
Lipids are insoluble in water
Waterproofing to conserve water |
|
|
What two features are fats (lipids) useful for?
|
Insulation - retains body heat as fats are slow conductors of heat
Protection - surrounds organs such as kidneys |
|
|
What are the main groups of lipids?
|
Triglycerides (fats and oils), phospholids and waxes
|
|
|
Condensation reaction of glycerol + 3 fatty acids -->
|
Triglyceride + 3 waters
|
|
|
Why are oils liquid at room temperature whereas fats are solid?
|
Oils are unsaturated, the double bonds cause a curve and so cannot pack together as closely as fats which are saturated (have no double bonds)
|
|
|
Where do the differences in the properties of fats and oils come from?
|
Fatty acid, glycerol remains the same in all.
|
|
|
What does saturated mean?
|
No double carbon-carbon bonds. Each carbon is bonded with the maximum number of hydrogen atoms
|
|
|
Hat does monounsaturated mean?
|
One double carbon-carbon bond present
|
|
|
Phospholipid structure
|
Phosphate hydrophilic head(polar)
2 fatty acids which are hydrophobic |
|
|
Test for lipids
|
Add 2.5x solution volume of ethanol
Add equal volume to that of ethanol of water Shake Cloudy white emulsion indicates presence of a lipid |
|
|
If you did the test for lipids on water what colour should the final solution be?
|
Clear, colourless
|
|
|
Why does an emulsion appear cloudy?
|
Light passing through is refracted from water to oil droplets as the sample is dispersed in solution finely
|
|
|
Before testing for lipids what should you check for in the test tube?
|
Grease free
Dry Otherwise it may show a positive result when there is nothing there |
|
|
What gives plasma membranes their different properties?
|
Substances such as proteins and cholesterol
|
|
|
what bonds are there in cellulose?
|
1-4 glycosidic bonds within the beta-glucose molecules
There are also hydrogen bonds between the chains which give great tensile strength |
|
|
Where is the hydroxyl group in relation to carbon 1 in alpha glucose?
|
Below carbon 1
|
|
|
Three hexose monosaccharides
|
Glucose
Fructose Galactose |
|
|
Which is more soluble (and thus sweeter): fructose or galactose
|
Fructose
|
|
|
What are alpha and beta glucose?
|
Structural isomers
|
|
|
What bond is found in maltose?
|
1-4 alpha glycosidic bond
|
|
|
What bond is found in sucrose?
|
1-4 alpha glycosidic bond
|
|
|
What bond is found in lactose?
|
1-4 beta glycosidic bond
|
|
|
Where and how is starch stored?
|
In plants
As grains called in organelles called plastids |
|
|
How is starch produced?
|
Photosynthesis
|
|
|
During which process is starch broken down?
|
Respiration
|
|
|
Photosynthesis equation
|
Carbon dioxide + water --> alpha glucose + oxygen
|
|
|
Respiration equation
|
Glucose + oxygen --> carbon dioxide + water
|
|
|
Why and how is cellulose very strong?
|
Hydrogen bonds between layers give great tensile stress
Microfibrils are layered over each other to prevent cells from bursting ehrn they take in excess water |
|
|
Animals do not store carbohydrates as starch but as..
|
Glycogen
|
|
|
What bond is present in glycogen
|
1-6 alpha glycosidic bonds
|
|
|
Where and how is glycogen stored?
|
Granules inside liver/muscles
|
|
|
Why can glycogen be broken down quicker via metabollism than starch
|
More soluble
Less dense |
|
|
Examples of pentose monosaccharides
|
Ribose and deoxyribose
|
|
|
What is different structurally between ribose and deoxyribose?
|
Deoxyribose does not have a hydroxyl group attached to carbon 2 like ribose does, only another hydrogen.
|
|
|
What are dextrins?
|
Partial breakdown by-products of starch when it has been hydrolysed
|
|
|
What are the advantages of saccharides being soluble?
|
Easily absorbed into system to use as energy in the form of ATP.
|
|
|
What are the advantages of saccharides being sweet?
|
Aid seed dispersal
Attracts animals |
|
|
Describe the process by which proteins transport molecules through active transport
|
Molecules/ions bind to receptor of protein
ATP binds to protein - which splits into ADP and a phosphate molecule. As a result, the protein molecules changes shape and releases the molecules onto the other side of the membrane |
|
|
Features of fibrous proteins
|
Insoluble in water
Structural Rope like structures with high tensile strength Parallel polypeptide chains with cross links Silk, keratin, collagen |
|
|
Features of globular proteins
|
Transport
Spherical shape caused by tightly folded polypeptide chains Soluble as hydrophyllic groups on outside whilst hydrophobic groups on inside |
|
|
What are essential amino acids?
|
Those which have to be present in a person's diet as they cannot be manufactured inside the body
|
|
|
Effect of temperature on enzymes
|
Increasing temperature increases kinetic energy
Collisions become more frequent More ES complexes formed, and more product Once past the optimum temperature, too much energy causes bonds within the enzyme (H) to break This denatures the enzyme, affecting its shape meaning that it is no longer complementary to the substrate and so it will no longer bind to the substrate. No more ES complexes are formed and so there is a decrease in rate of reaction. |
|
|
Effect of pH on enzymes
|
H+ ions acidic
OH- ions alkaline Charged ions disrupt ionic bonds within enzyme's structure. This denatures the enzyme, affecting its shape meaning that it is no longer complementary to the substrate and so it will no longer bind to the substrate. No more ES complexes are formed and so there is a decrease in rate of reaction. |
|
|
Effect of increasing substrate concentration on enzymes
|
Increasing substrate concentration increases number of substrate molecules
Collisions between enzyme and substrate more frequent. More ES complexes formed, more product increases rate of reaction until enzyme becomes saturated. Enzyme works at max turnover rate - number of enzymes is the limiting factor. |
|
|
What do the hydrophilic heads interact with in the cell-surface membrane?
|
Water in cytoplasm of cell/ water surrounding cell
|
|
|
Functions of phospholipids in cell-surface membrane
|
Make membrane flexible
Prevent water soluble substances entering and leaving cell Allow lipid soluble substances to enter and leave the cell |
|
|
Definition and examples of extrinsic/Peripheral (proteins)
|
Partly embedded in cell-surface membrane
Does not extend completely across it Glycolipid, glycoprotein, proteins |
|
|
Definition and examples of intrinsic/Integral (protein)
|
Completely span the phospholipid bilayer
Carriers, enzymes |
|
|
Function of cholesterol in fluid-mosaic model
|
Add strength
|
|
|
Function of glycolipids in fluid-mosaic model
|
Recognise other cells
|
|
|
Function of glycoproteins in fluid-mosaid model
|
Receptor molecules to bind with hormones or neurotransmitters
|
|
|
Function of enzymes in fluid-mosaic model
|
Catalyse reactions on cell-surface
|
|
|
Why can heat lead to the cell-surface membrane becoming "leaky"?
|
Increase kinetic energy, vibrate more, pores become unstable and let through more molecules
|
|
|
What is one way to increase resistance to heat in the cell-surface membrane?
|
Increase amount of cholesterol in it.
|
|
|
Why is the fluid-mosaic model called "fluid"?
|
Flexible
Molecules more relative to each other |
|
|
Why is the fluid-mosaic model called "mosaic"?
|
Embedded proteins vary is size and shape
|
|
|
Drugs that bind to receptors and mimic the body's normal messengers are called
|
Agonists
|
|
|
Drugs that bind to receptors and block the body's normal messengers are called
|
Antagonists
|
|
|
Why must water pass via osmosis through a channel protein
|
water is an ion
water must avoid the hyrophobic tails of the phospholipds in membrane structure |
|
|
Factors which affect rate of diffusion
|
Temperature
Concentration gradient Surface area Thickness |
|
|
Ions diffuse through membranes via?
Passive/Active? Examples |
Channel proteins
Facilitated diffusion Passive process Salt/Water |
|
|
Larger molecules diffuse through membranes via?
Passive/Active? Examples |
Carrier protein
Facilitated diffusion Passive - as it goes along the concentration gradient Glucose |
|
|
What is dynamic equilibrium?
|
There is an equal number of molecules on both sides but their positions are always changing
|
|
|
Why does the rate of facilitated diffusion plateau after a while?
|
Once carrier/channel proteins are saturated they cannot bind to any more molecules
|
|
|
Diffusion is proportional to
|
the difference in concentration between two areas
|
|
|
What size molecules diffuse faster - big/small?
|
Small
|
|
|
How do proteins transport molecules to the other side of the membrane?
|
Bind to molecule
Protein changes shapes in such a way that the molecule is released across the membrane |
|
|
Name two substances which pass through membranes via simple diffusion
|
CO2
O2 |
|
|
What effect does adding a solute do to a solution's water potential?
|
Lower
|
|
|
In what direction does water move?
|
From an area of high er water potential to an area of lower water potential
|
|
|
The highest water potential available is
|
0
|
|
|
Percentage change =
|
[(new value - old value)/old value] x 100
|
|
|
What happens to a plant cell if put in a solution with a higher water potential than itself?
|
Net movement = enters plant cell
Vacuole and cytoplasm increase in volume Cell membrane and protoplast pushed up against cell wall Plant cell swells to become TURGID |
|
|
What happens to a plant cell if put in a solution which has a lower water potential than itself?
|
Net movement of water = leaves plant cell
Vacuole and cytoplasm decrease in volume Cell membrane and protoplast pulled away from cell wall Plant cell shrinks, is FLACCID and then goes onto becoming PLASMOLYSED |
|
|
What happens to an animal cell if placed in a solution which has a higher water potential than itself?
|
Net movement of water = enters animal cell
Cell swells and may burst because animal cells do not have a cell wall |
|
|
What happens to an animal cell if placed in a solution which has a lower water potential than itself?
|
Net movement of water = leaves animal cell
cell shrinks and may become flaccid |
|
|
What happens to an animal/plant cell when placed in a solution which has an equal water potential to itself?
|
Net movement of water = neither enters nor leaves
Cell remains in same state |
|
|
In what direction does active transport move molecules?
|
From an area of low concentration to an area of high concentration
|
|
|
What is required for active transport to work?
|
Energy in form of ATP
|
|
|
What happens to ADP during repiration?
|
Bonds with a phosphate molecule to make ATP which can be used for active transport
|
|
|
Metabollic energy is provided in the form of
|
ATP
|
|
|
How is glucose absorbed from the small intestine?
|
Sodium ions are actively transported out of the epithelial cell (villus) into the blood via the sodium-potassium antiport pump.
There is now a higher concentration of sodium ions in the lumen in comparison to that in the epithelial cell. Sodium ions through facilitatied diffusion diffuse via a symport cotransporter with glucose. Sodium goes along conc. gradient whereas glucose goes against conc. gradient. Glucose passes through epithelia cell into blood via a different carrier protein |
|
|
Why is glucose absorption in the small intestine an indirect form of active transport rather than a direct form?
|
Concentration gradient movement of sodium ions powers the movement of glucose molecules rather than ATP directly.
|
|
|
What is the role of the cell wall in a prokaryotic cell?
|
Physical barrier against mechanical damage to exclude certain substances made of polysaccharides and polypeptides (peptidoglycan)
|
|
|
What is the role of the capsule in a prokaryotic cell?
|
Mucilaginous layer which helps bind cells together
Also hides antigens on cell surface |
|
|
Wha is the role of the plasmid in a prokaryotic cell?
|
Allows cell to survive in adverse conditions by reproducing independently (to give resistance to antibiotics)
|
|
|
What is the structure of the plasmid in a prokaryotic cell?
|
Small circular piece of DNA
|
|
|
Where are mesosomes found, what is their function and what is their structure?
|
Infoldings of cell surface membrane which hold enzymes associated with respiration in prokaryotic cells.
|
|
|
What is the function of the cell surface membrane in prokaryotic cells?
|
Controls entry and exit of materials - selectively permeable.
|
|
|
What is the structure of cytoplasm in prokaryotic cells?
|
jely-like substance which contains enzymes
|
|
|
What is the function of a flagellum?
|
Locomotion - aid movement to help cell spin through fluids
|
|
|
What is the structure of a flagellum?
|
Rigid corkscrew shape - looks like a tail.
|
|
|
What is the scientific name of cholera?
|
Vibrio cholorae
|
|
|
How is cholera transmitted?
|
Drinking contaminated water (with faecal matter) as a result of unpurified water or leakages of sewage.
Faecal contamination of hands Eating shellfish which feed from the sea |
|
|
In what form is DNA contained in a prokaryotic cell?
|
Circular strings of DNA
Nuclear material |
|
|
How are most cholera bacteria killed when ingested?
|
Killed by acidic conditions in stomach
|
|
|
Where and how do surviving cholera bacteria transport themselves once in our bodies?
|
Propel themselves in a corkscrew fashion using flagellum through the mucus lining of small intestine
|
|
|
How does the cholera baterium cause disease?
|
Produces a toxic protein
1. One part binds to complementary carbohydrate cell receptors on epithelial cell of small intestine 2. Other part binds to chloride channel proteins. As a result, the chloride channel proteins open, raising the the water potential inside epithelium. Thus, water moves out of the epithelium cell into the lumen from an area of higher water potential to an area of lower water potential. As a result, the chloride concentration within epithelial cell of smal intestine is lowered, meaning that chloride ions diffuse via channel proteins from the blood. Thus, the water potential inside epithelial cell increases in comparison to the blood. In order to retify this, water moves from the blood by osmosis back into the epithelial cell. |
|
|
Why do we get diarrhoea when we have cholera (toxin)?
|
Loss of chloride ions inside epithelial cell of small intestine raises water potential in epithelial cell higher than that of the lumen of small intestine meaning that water moves via osmosis out into the lumen
|
|
|
Why do we become dehydrated when we have cholera?
|
Loss of chloride ions means that there is a higher concentration present in blood in comparison to the epithelial cell and so chloride ions move from the blood into the epithelial cell via channel proteins.
As a result, the water potential inside the epithelial cell of small intestine lowers to that of the blood and so water from the blood moves into the epithelial cell through osmosis. |
|
|
Where are pili found, what do they look like and what is their function?
|
Hair-like structures on prokaryoic cells
Help transfer genetic material between bacteria - conjugation |
|
|
Why else might we get diarrhoea when we have cholera?
|
Loss of microvilli due to toxins
|
|
|
Why is drinking water ineffective when you have cholera?
|
Not being absorbed
Does not replace electrolytes (ions) being lost |
|
|
Disadvantages of ORT?
|
Requires trained personnel
Tested on animals and children Given regularly in large amounts |
|
|
What do ORT solutions contain and why?
|
Water - rehydrate tissues
Sodium - use alternative sodium-glucose carrier proteins Glucose - stimulate sodium-glucose carrier proteins as it s powered by active transport; also to provide energy Potassium - replace lost K ions and stimulate appetite Electrolytes - reduce electrolyte imbalance |
|
|
Why do aerobic organisms require a constant supply of oxygen?
|
Release energy in form of ATP from respiration
lots of ATP needed as we have high metabollic rates - with a large volume of cells. |
|
|
State structures which air moves through during inhalation
|
Mouth/nostril
Trachea Bronchus Bronchiole Alveoli |
|
|
Meaning of poikliothermic
|
Cold blooded
|
|
|
Meaning of homeothermic
|
Warm blooded
|
|
|
Features which make lungs effective for gas exchange/ prone to infection
|
Moist - dissolve CO2 and O2
High surface area to volume ratio - maximise gas exchange Rich blood supply - circulate O2 to cells and CO2 out - maintain concentration gradient Thin - short diffusion pathway for O2 and CO2 - partially permeable |
|
|
Why must mammalian lungs be internal?
|
Need to be moist - if outside they would dry out
Protected by ribcage Air is not dense enough to support lungs. |
|
|
Decribe structure of lungs
|
Lobed
Range inside from bronchioles to alveoli |
|
|
Decribe structure and function of trachea?
|
Rings of cartillage to prevent trachea collapsing when air pressure FALLS during inspiration
Ciliated epithelium waft trapped dirt up to oesophagus to be swallowed into stomach Goblet cells produce mucus to trap dirt and bacteria |
|
|
What is similar about bronchi with the trachea?
|
Also lined in ciliated epithelial cells
Larger bronchi supported with cartilage |
|
|
What are the bronchioles lined with?
|
Muscle made of epithelial cells
Muscle can constrict to control air flow |
|
|
Describe structure of alveoli
|
Collagen and elastin fibres allow alveoli to stretch when filled with air (and recoil back when epelling carbon dioxide)
Lined with epithelium |
|
|
Decribe function of alveolar membrane
|
Gas exchange surface
|
|
|
What feature makes alveoli effective?
|
Millions of spherical alveoli - large surface area
|
|
|
What is on the surface of the alveoli and decribe how its structure relates to its effectiveness?
|
Network of capillaries which are one cell thick.
Short diffusion path - 2 cells between air space and capillary Alveolus epithelial lining Blood capillary endothelial lining Red blood cell - squeezed inside capillary s it pushes up against side |
|
|
Describe mechanism of inspiration
|
Internal intercostal muscles relax
External intercostal muscles relax Ribcage moves up and out Diaphragm contracts and flattens Internal volume increases Internal pressure inside decreases lower in comparison to outer atmosphere Air passes in from an area of higher pressure (out) to an area of low pressure (in) |
|
|
Describe mechanism of expiration
|
Internal intercostal muscles contract
External intercostal muscles relac Diaphragm relaxes and goes up Ribcage moves down and in Volume inside decreases Internal volume increases Air moves out from an are of higher pressure (in ) to an area of lower pressure (out) |
|
|
Units of Pulmonary Ventilation
|
dm^3min^-1
|
|
|
Pulmonary Ventilation equation
|
= tidal volume x ventilation rate
|
|
|
Units of tidal volume
|
dm^3
|
|
|
Units of ventilation rate
|
min^-1
|
|
|
Wat can pulmonary ventilation indicate?
|
Pulmonary disease - lungs working inefficiently
|
|
|
Symptoms of pulmonary tuberculosis
|
Persistent cough
Tiredness Loss of appetite Weight loss Shortness of breath Fever Coughing up blood |
|
|
How can TB be prevented?
|
BCG vaccine
|
|
|
How is pulmonary tuberculosis transmitted?
|
Air droplets egested when an infected individual sneezes, laughs or talks.
Bacteria is then inhaled Transmitted through unpasteurised milk from cows |
|
|
Describe the course of infection of pulmonary tuberculosis
|
LOCAL PRIMARY INFECTION: Bacteria grow and divide in upper regions of lungs - where there is a plentiful supply of oxygen
White blood cells (T cells and macrophages) accumulate at site of infection and isolate bacteria (in a dormant state) in tubercles This leads to inflammation and enlargement of lymph nodes in lungs Once the individual's immune system is weakened the bacteria can break through the tubercle/ if a different strain re-emerges POST-PRIMARY TUBERCULOSIS occurs: Infected tissue encased in tubercle dies, forming scar tissue - fibrosis Once the bacterium enters the bloodstream it can spread to the kidneys, bone and spinal cord. |
|
|
How can pulmonary tuberculosis be treated?
|
Antibiotics
Inactive TB can be prevented from becoming active using anibiotics Active TB requires several antibiotics |
|
|
In what kind of areas does pulmonary tuberculosis tend to be more widespread?
|
Poor hygiene levels
Poor ventilation system Crowded areas - hospitals, prisons Damp |
|
|
Why might a person not show any symptoms of pulmonary tuberculosis and not transmit the bacteria on?
|
Bacteria isolated in an inactive state within a tubercle
|
|
|
When and where does post-primary pulmonary tuberculosis arise?
|
Adults
Upper region of lungs where oxygen is plentiful for bacteria to respire |
|
|
Why is one of the symptoms of TB a fever?
|
Body raises temperature so that it makes it harder for bacteria to replicate themselves - so that the body's immune system can gain advantage.
|
|
|
Why is one of the symptoms of TB a cough?
|
Body tries to expel damaged lung tissue as it is blocking the airways, along with blood
Reflex action |
|
|
Why is one of the symptoms of TB shortness of breath?
|
TB causes fibrosis which reduces the tidal volume meaning that it is hard for the lungs to be efficiently ventilated
Damaged tissue is thickened and becomes less elastic, increasing the diffusion path meaning that it is harder for the lungs to maintain an oxygen concentration gradient. |
|
|
What is pulmonary fibrosis?
|
Epithelium of the lungs becoming thickened as a result of scars.
|
|
|
Why might you get chest pain if you have pulmonary fibrosis?
|
Lung damage and change of pressure ?
|
|
|
Why is it hard for air to be expelled out if you have pulmonary fibrosis?
|
Lung tissue become less elastic
|
|
|
What is dyspnea?
|
Shortness of breath
|
|
|
Why may you suffer from weakness/fatigue if you have pulmonary fibrosis?
|
Reduced oxygen transfer into blood as a result of reduced tidal volume
Less oxygen - less respiration - less energy produced |
|
|
State groups with reduced immunity
|
Malnutrition
AIDS Taking immunosuppressants Very old/very young Take drugs Smoke Chemotheraphy |
|
|
Why is Pulmonary Tuberculosis making a comeback?
|
New strains resistant to antibiotics
Overcrowding in houses Fewer vaccinations |
|
|
What is asthma?
|
Localised allergic reaction which affects the bronchioles
|
|
|
What causes asthma?
|
Allergic triggers such as pollen, cold air, exercise cause the white blood cells lining the bronchi and bronchioles to release the chemical histamine
STIMULI Laughing = hyperventilating |
|
|
What are the effects of asthma (in lungs)?
|
Airway lining becomes inflamed and sensitive
Goblet cells present on epithelial cells on bronchioles secrete larger amounts of mucus than normal, blocking oxygen from reaching alveoli Smooth muscle surroundng bronchioles have contracting spasms, narrowing airways further. Difficult to ventilate lungs |
|
|
Why is gas exchange less efficient for asthma sufferers?
|
Thicker diffusion path - contracting muscle
Lower concentration gradient - greater resistance of air flow due to mucus and fluid in airways Smaller surface area - airways become narrower because of muscle spasms and inflammation |
|
|
Why do asthma sufferers have difficulty in breathing?
|
Obstruction in bronchioles
Inflamed linings Mucus Fluid |
|
|
Why do asthma sufferers make a wheezing sound when breathing?
|
Air passing though a narrow, constricted bronchi and bronchioles
|
|
|
Why do asthma sufferers experience a tight feeling in chest?
|
Lungs not ventilated properly as a result of obstructed bronchi and bronchioles
|
|
|
Why do asthma sufferers cough?
|
Reflex action in an effort to remove obstruction (mucus and fluid) in bronchi and bronchioles
|
|
|
Risk factors of asthma
|
Hereditary = some are more prone to allergic hypersensitivity
Bronchiolitis = lung infection causing the swelling of bronchioles Smoking = weakens immune system and lungs making you more prone to infections such as bronchiolitis Premature baby = lungs not developed |
|
|
Why is there an increase in asthmatics?
|
Increase of air pollution
Chemicals present in food |
|
|
What are the effects of emphysema (in lungs)?
|
Elastin permanently stretched in lung tissue
Irreversible air pockets in alveoli - walls break down Smoking and air pollution paralyse the cilia - mucus builds up in clumps and is coughed up Bronchial tubes become inflamed - creating more mucus Smoking causes growth of fibrous tissue around bronchioles, narrowing the passageway |
|
|
Why do people with emphysema feel breathless?
|
Loss of elasticity in lungs mean that alveoli cannot fill up with fresh air containing a higher percentage of oxygen as it can't expel the "old" air out
Smaller surface are as a result of damaged alveoli lead to reduced levels of oxygen - person breathes more to make up for insufficient oxygen |
|
|
Why do people with emphysema feel tired?
|
Alveoli walls ruptured, smaller surface area, less oxygen uptake
Less elastin in alveoli meaning that they cannot expel air to replenish themselves with fresh air in order to maintain a concentration gradient. As a result, there is less oxygen available for respiration, to provide energy for cells. |
|
|
Why do people with emphysema have a chronic cough?
|
Body's reflex in an attempt to expel damaged lung tissue and mucus which cannot be removed naturally since the cilia on the bronchi and bronchioles have been destroyed
|
|
|
Where does the left side of the heart transport blood (oxygenated/deoxygenated?) to?
|
Body
Oxygenated |
|
|
Where does the body transport blood (ox/deox?) to?
|
Right side of heart
Deoxygenated |
|
|
Where does the lungs transport (ox/deox?) blood to?
|
Left side of heart
Oxygenated |
|
|
Where does the right side of the heart transport (ox/deox?) blood to?
|
Lungs
Deoxygenated |
|
|
Why is there a double pump system?
|
Insufficient pressure for blood to travel whole way around body
|
|
|
What is the function of the heart?
|
Deliver essntial materials to all cells such as monosaccharides, amino acids, fatty acids, glycerol, oxygen, hormones and water.
Also removes waste products such as carbon dioxide and urea. |
|
|
Why is the muscle size of the atria smaller than the muscle size of the ventricles?
|
Atria needs to transport blood short distance - down - whereas ventricles have to pump blood all the way to body/lungs
|
|
|
Why does the left ventricle have more muscle than the right ventricle?
|
Lungs are closer than the extremities of the body
|
|
|
If the coronary arteries become blocked what happens, and why?
|
Myocardial infarction
Area becomes deprived of oxygen and nutrients and so dies. |
|
|
What prevents oxygenated and deoxygenated blood mixing in the heart?
|
Septum
|
|
|
What is the difference between the bicuspid and tricuspid valves
|
bi = right side of heart - two cup shaped flaps
tri = left side of heart - three cup shaped flaps |
|
|
Function of aorta
|
Carries oxygenated blood to the body
connected to left ventricle |
|
|
Function of vena cava
|
Carries deoxygenated blood back from the body
connected to right atrium |
|
|
Function of pulmonary artery
|
Carries deoxygenated blood to the lungs
connected to right ventricle |
|
|
Function of pulmonary vein
|
Carries oxygenated blood back from lungs
connected to left left atrium |
|
|
Describe the cardiac cycle
|
Blood enters atrium. Higher pressure in atrium than in ventricles and so atrioventricular valves open to allow blood to enter into the ventricles.
The ventricle now has a higher pressure than in the atrium bu the valves prevent backflow of blood. Ventricle has higher pressure than aorta. Semi-lunar valves open to allow blood to pass through to aorta. Aorta now has a higher pressure than the ventricles but the semi-lunar valves prevent backlfloe of blood back into ventricle. |
|
|
What happens to the heart muscles when blood enters into atrium down into ventricle?
|
Atria diastole
Ventricle diastole |
|
|
What do the heart muscles do to actively get the last 20% of blood into ventricle?
|
Atria systole
Ventricle diastole |
|
|
Why is there a short delay before the impulses pass through the AVN?
|
Allows time for atria to empty before going into systole
|
|
|
Why does ventricle contraction start at the apex?
|
Systole pushes blood upwards towards major arteries
|
|
|
Wha muscles contract during ventricular systole?
|
Papillary
|
|
|
What causes the "lub dub" sound?
|
1. atrioventricular valves closing
2. semi-lunar valves closing |
|
|
What do the heart muscles do to release blood out rhough major arteries?
|
Atria diastole
Ventricle systole |
|
|
Describe the structure of valves in heart
|
Tough but flexible and fibrous tissue
|
|
|
Cardiac output =
|
stroke volume (dm^3) x heart rate (min^-1)
|
|
|
Why is the pressure in the atrium never very high?
|
Thin walls of muscle
|
|
|
Why is the pressure in the aorta always fairly high?
|
Small diameter
|
|
|
Why does the aortic tissue recoil?
|
As blood passes through the aorta's diameter widens
Elastic tissue goes back into original shape |
|
|
Define myogenic
|
not controlled by brain
Heart is controllen by SAN (pacemaker) Muscle contraction initiated from muscle itself |
|
|
Describe the nervous control of the cardiac cycle
|
SAN initiates impulse
Impulse travels across both atria causing atrial systole The atrioventricular septum (a layer of insulating tissue) prevents the impulse from reaching the ventricles. This allows time for the atria to empty into the ventricle before the ventricle goes into systole. The impulse arrives ar the AVN which conducts the impulse after a short delay through to the ventricular septum. The impulse travels through the ventricular septum via the bundle of His down into the apex The purkinje fibres branch out conducting the impulses through to the left and right ventricles, stimulating the ventricles to go into systole |
|
|
Where is the SAN located?
|
Top of right atrium in the heart
|
|
|
Suggest one advantage of the high rate of conduction in the Purkinje fibres?
|
Contract quickly so that both ventricles go into systole simultaneously
|
|
|
Why do those with CHD have a reduced blood supply to cardiac tissues?
|
Arteries become narrowed as a result of atheroma
|
|
|
What is an atheroma? What is the effect?
|
Fatty plaques deposited in the inner lining (endothelium) of arteries as a result of high levels of LDLs in diet
Narrows the artery Increases risk of blood clotting Traps white blood cells |
|
|
Why do those with CHD have higher blood pressure?
|
Narrowed vessels - smaller volume = higher pressure
|
|
|
What is angina and how is it caused?
|
Chest pain due to shortage of blood to specific regions of heart muscle - muscles do not die
Blood flow restricted further down on one of the smaller coronary arteries. |
|
|
What is atherosclerosis?
|
Narrowing of coronary arteries
Hardened, become less elastic |
|
|
Why is angina more prone during exercise?
|
Exercise = heart works harder to transport oxygen to respiring cells and get rid of carbon dioxide
|
|
|
What causes myocardial infarction?
|
Coronary artery totally blocked by thrombus
No blood supply to heart muscle, deprived of oxygen and nutrients and so dies - cannot pump any more. |
|
|
Describe embolus
|
Circulation of thrombus which gets lodged in different arteries - can affect brain
|
|
|
What is atheromatous plaque made of?
|
cholesterol
fibre dead muscle cells white blood cells which have taken up LDLs |
|
|
Describe aneurysm
|
Weak walls which may burst outwards- haemorrhage
|
|
|
Why do the artery walls harden if you have high blood pressure?
|
Protects walls from damage from high pressure
|
|
|
What type of lipoproteins does the liver break down?
|
High density lipoproteins
|
|
|
What is the function of high-density lipoproteins?
|
Pick up low-density lipoproteins and transport it to the liver for excretion.
|
|
|
What is the function of low-density lipoproteins?
|
Transport cholesterol from the liver to the tissues
|
|
|
Describe the formation of thrombosis
|
Atheroma plaque ruptures - tough surface
LDLs deposit on rough surface |
|
|
Why is smoking a risk factor for CHD?
|
Carbon monoxide binds irreversibly to haemoglobin - carboxyhaemoglobin
Reduces capacity for oxygen to bind - reduced uptake of blood, heart works harder to overcome Nicotine - adrenaline increases heart pressure and heart rate Increases risk of thrombus as platelets more readily form clots (become sticky) |

