![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
|
Adaptive vs innate immunity |
Innate is for all Adaptive is 4 vertebrates only |
|
|
First line of defense of immune system |
Secretions that trap or kill pathogens guard the body’s entrances and exits, while the linings of the digestive tract, airway, and other exchange surfaces provide additional barriers to infection. |
|
|
Innate immunity of invertebrates |
-Insect exoskeleton (polysaccharide chitin) is physical defense -chitin lines intestine to block infections-lysozyme in digestive system is chemical barrier -Insect exoskeleton (polysaccharide chitin) is physical defense -chitin lines intestine to block infections-lysozyme in digestive system is chemical barrier -Insect exoskeleton (polysaccharide chitin) is physical defense -chitin lines intestine to block infections-lysozyme in digestive system is chemical barrier |
|
|
Lymphocytes
|

Ada ptive immunity relies on T cells and B cells, which are types of white blood cells called lymphocytes. originate from stem cells in the bone marrow called hematopoietic stem cells. Some IMMATURE T CELLS migrate from the bone marrow to the thymus, an organ in the thoracic cavity above the heart These lympho-cytes mature into T cells there in the thymus. Lymphocytes that remain and mature in the bone marrow develop as B cells there in the bone marrow. (Lymphocytes of a third type
remain in the blood and become the natural killer cells active in innate immunity.). T and B cells responds to antigen n have antigen receptors n have specificity area that bind to A specific part of the antigen EPITOPE They have just one variety of receptor n all of the antigen receptors made by a single B or T cell are identical. N they go thru the lymph nodes |
|
|
What type of response to T cells and B cells respond to respectively |
T cells do t cell mediated immmuneresposnse n b cell does antibody respone aka humoral reponse
|
|
|
How many epitope are there in a antigen |
alot
|
|
|
WHAT MAKE S A t CELL NAIVE |
NEVER ENCOUNTERED AN ANTIGEN
|
|
|
RECEPTOR EDETING |
MAKING SURE T AND B CELLS DONT ATTACK SELF
|
|
|
Central vs peripheral lymphoid organs |
central is bone marrow as well as thymus and peripheral is spleen n stuff
|
|
|
primary v sopportunistic infectuons |
primary is make healthy ppl sick can b life threwarning can b asymtomatic. opportunistic is when body weak they get triggered
|
|
|
Innate immunity vs adaptive immunity |
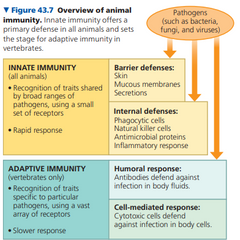
innate is preexisting n immediate N NONSPECIFIC N IS FIRST LINE OF DEFENSE .
|
|
|
Innate immunity of invertebrates |
only in phagocytic cell, epithelial cells r also a ddefense, linked together by tight junctions n marka a seal, when a pathogen can get thru thats an infection, mucus traps n tags invadors, HCL in stoam,ch
|
|
|
B cells look like |
|
|
|
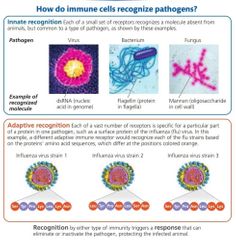
Pattern recognition receptors PRR |
distinguish seld n nonself, innate is braid so it reads but doesnt memorize. There can be free, membrane bound, phagocytic. Recgonoxze fifrent patterns recognize PAMPS
|
|
|
Toll like receptors |
part of cellular innate immunity, recognixze ligands n have diff actions, some initiate phagocytosis. Ca b extra or inntra cellular. Maling a signal transduction pathway.
TL3 recognize double stranded viral DNA, TL4 recognize lippolysachride found on some bacteria. TL5 recognizes protein fro bacterial flagellum, tl9 recognizes protozoa DNA |
|
|
Toll receptors on fruit flys |
droso mason.experiment, 4 chroimosmes, wild type is stamndra, mutant is low expression of toll receptor protein .
is toll pathways required for immune response . We treat flies by exposing them to water or fungal spore water . Normally can fight against fungus. Follow survival rates of 6 days. 4 samples, mutant vs wild and water vs fungus . U need air flow n year nutrients to keep control to make sure they dont accidenl die. A northern blo for RNA. we looking at antipathogen genes the fighters. We get mrna then do gel electrophoresis. We take to membrane to probe. After 3 days mutant n fungus died. Northen blo showed low antipathogen in wild type water cuz ofc they not threatened. High at wild type fungus ofc cuz they being attacked. N mutant fungus w little nno make sense cuz they should have high antigen cuz they getting attacked meandsthat wo toll they not going thru antipathogen synthesis. No active immune response. We followed the downstream genes made. TOLLLLLL in flys not toll like, we do toll like |
|
|
Inflamatoorry response |
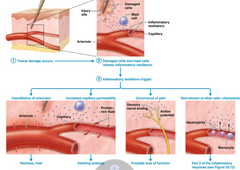
tissue damage occurs
histamine vasodilates damage cells n mast cells release stuff like cytokines, which trigger stuff vasodillation of arterioles (red n hot), increased capillary permeability(CELLS ENTER N EXIT LIKE NEUTROPHILS), pain, chemotaxis (recruit other cells). Macrophages LIVE THERE r activated n trigger neutrophils n macrophages,. Local macrophages r activated, neutrophils come into area thru chemoxtaxis n start to do diapedsis (crawl out of edethelial cells from blood to tissue). Monocytes also come in by chemotaxis n become macrophages b phagocytize the cellular debris. Endothelial cites refctuit leukocytes (from bone marrow ) to place which make cell adhesion molecules called selectins. Selectins make membrane stickier making it easier to snag leukocytes from blood. Once snagged they enter prtocess of entry. This is called margination when it interacts w selectin of endothelial cells n strarts to move into tissue (diapedisis) leukocytes n neutrophils do margination downstream condeseuwnece is (leukocytosius) bone marrow will make more leukocuyes |
|
|
Cytokine |
small proteins,
enhance immune response in short distnmaces, can do paracine, autocrine n endo associated w inflammation ex interferon (virus enters host, replicates, we turn on interferon gene, makes interferon mrna to inteferon proteins to intergerons molecules that alerts neighnoring thru interferon receptors (so water soluble) signaling cells that turn on antiviral proteins being synthesized. OG cell dies but neighbors survive) interleukins (cytokines made by t lhymphocites innate n adaptive immunity. activate macrophage. apoptotic pathway taslk. incraese t cells) tumor necrosis factor( made by macrophages when find bacteria, recruit phagoicytes to infection, stimulate more cytokines, kill cancer cells) colony stimulating factors (luekopoliss) chemokines (TAXING , CONTROL RATE OF MOVMENT N RECRUITMENT) if too much could b harmful so we havae to limit |
|
|
Fever |
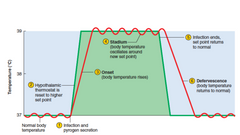
pyrexia aka fever, has increase intervferon, tissue repear.
Pyrogens initiate heat both exogenous (from bacteria) and endigenous(cytokines), in and out of cell. Stimulates neurons in hypothalmus that raises normal range of body temp, we maintain stadium, temp related to pyrogen amount. Once it ends its defervescence body return to normal. |
|
|
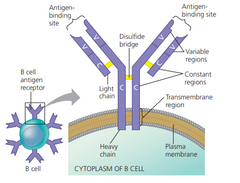
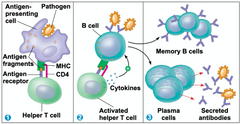
What happens after a B cell binds with an antigen |

Note B cells bind to intact antigens. Ok after that formation of cells that secrete a soluble form of the receptor. This secreted protein is called an antibody, also known as an immunoglobulin (Ig). Antibodies have the same Y-shaped structure as B cell antigen receptors but lack a membrane anchor. They provide a direct defense against pathogens in body fluid by binding to antigen n interfering w its activity or marking for destruction like neutralization ADD PIC
|
|
|
T cell look like |
|
|
|
Similarities n differnce3s btween t and b cells |
t cell activation is dif by when become effector cell aka activated they remain bound to emembrane. Receptor all on cell, disulfide bridge, transmembrane region, polypeptide, antigen binding site, constant region
|
|
|
Difference btween BCR n antibodies |
antibodies ois just y shaped floating around, BCR is when its still stuck on B cell
|
|
|
B cell looks like |
|
|
|
What happens after T cell binds with an antigen |
note t cells bind w fragments of antigen. Ok so they only detect cell surface antigen fragments. Those fragments r held by major histocompatibility complex (MHC) 2 molecule. So if theres no MHC presentation, t cell wont work
t cell communicated to self n dendritic cfell to t cell ADD PIC |
|
|
How do lymphocytes have different receptors |
same dna but recombinatiopn n introns n extrons translate to different variable regions |
|
|
Specificity of major histocompatibility complex (MHC) molecule |
not specific but antigen receptors of t cell v specific
mhc 1 says ahhh im infected MHC 2 is health of body n shows exogenoud peptides found |
|
|
four major characteristics of adaptive immunity |
First, the immense repertoire of lymphocytes and receptors enables detection of antigens and pathogens never before encountered.(example light chains in Ig has 200 different ways (40 V * 5 J * 1 C) and V and J regions use RECOMBINASE to do all types of combos. Only 1 allele of ligh n 1 of heavy are rearranged. This is permanent n passed to daughter cells) Second, adaptive immunity normally has self tolerance, the lack of reactivity against an animal’s own molecules and cells. (thymus, their antigen receptors are tested for self-reactivity. Some B and T cells with receptors specific for the body’s own molecules are destroyed by apoptosis) Third, cell proliferation triggered by activation greatly increases the number of B and T cells specific for an antigen. Fourth, there is a stronger and more rapid response to an antigen encountered previously, due to a feature known as immunological memory,
|
|
|
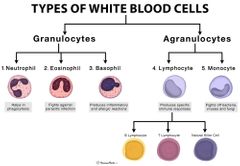
Macrophages |
all tissues found, fixed and moving. Long lived. First cells that phagocytosis when invaders come in. innate cuz they already there.
Have tissue damage n cells live in tissue predebut form is monocytes |
|
|
Neutrophils |
circulating, PRR on surface,
go from bloods stream to tissue. Phagocytic but mostly make a killing zone Engulkd n eat w lysosome enzymes or go throw their enzymes from lysosomes in tissue but make a toxic killing zone n kill self, usually dye at site. (respiratory burst which toxic chems) Chromatin nets that they make like spider, keep pathogens from going further n also kills themselves triggered by bacteria |
|
|
Eosinophils |
phagocytic against big parasitic worms,
at allergy n inflamation n pasratsitic infectiom places, release neurotoxins n trigger other cells to come help (basophils n mast cells) Stay at granules n are triggered when needed. |
|
|
Basophils aka mast cells |
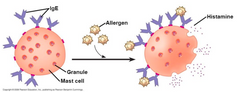
IGE aka natibody bind to mast cells, n when its triggered by an allergen it triggers antibody which triggers mast cell to release granules (degranulationn) calles histamine that call leukocytes (increase blood flow) and heparin (anticoouagulant makes blood not clot)
|
|
|
Dendritic cells |
phagocytosis,wridley distributed, immune response, prrs have, activated by phagocytosis n take to lymphatic system. Have costimulatory proteins which help activate cells associated w adaptive immunity. Release cytokines that influence adaptive immune response n r a rapid first line of defense
|
|
|
Natural killer cells |
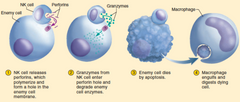
innate immune sytem, recrutied earlt. Destoy infected cells inducing cells to kill themselves. Engage w infected cells cuz they change membrane proteins. A protein called class 1 MHC proteins, that give info of cell health. When MHC expression goes down natural killer cells go to celll n release perforins that stab membrane n granzymes released that enter cell thru perforation which makes cell kill itself. Macrophage eats dead body.
|
|
|
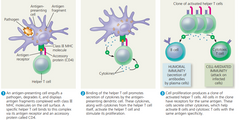
Clonal selection of lymphocytes |
when activated they clone selves n some become effector cells that are short lived n imminently attack pathogen ( for B cells these r called plasma cells which secrete antibodies and for T cells the effector r called helper T cells and cytotoxic T cells) the remaining r memory cells that r long lived that can trigger effector cells
|
|
|
Primary vs secondary immune response |
The primary
response peaks about 10–17 days after the initial exposure. If the same antigen is encountered again later, there is a secondary immune response, a response that is faster (typically peaking only 2–7 days after exposure), of greater magnitude, and more prolonged n rely on t and B memory cells |
|
|
Humoral vs cell mediated immune response |
humoral protects blood n lymph, eliminates toxins/pathogens in body fluids, can be seen if there's secretion of antibodies by clonally selected b cells. Cell mediated is specialized T cells destroy infected host cells
|
|
|
Helper t cell AKA cd4 CELLS |
activates humoral (b cells) and cell-mediated immune responses (cytotoxic t cell). Before this can happen, however, two conditions must be met. First, a foreign molecule must be present that can bind specifically to the antigen receptor of the helper T cell. Second, this antigen must be
displayed on the surface of an antigen-presenting cell. An antigen-presenting cell can be a dendritic cell , macrophage, or B cell (Antigen presentation by a dendritic cell or macrophage activates a not activated helper T cell, which then proliferates, forming a clone of activated cells. In contrast, B cells present antigens only to already activated helper T cells, which in turn activate the B cells. Activated helper T cells also help stimulate cytotoxic T cells) they present this info w their MHC1 molecule |
|
|
Antigen presenting cells vs infected cells |
Most body cells
have only the class I MHC molecules, but antigen-presenting cells have both class I and class II MHC molecules. The class II molecules provide a molecular signature by which an antigen-presenting cell is recognized. A helper t cell binds w class II MHC molecules w the help of CD4 protein n when they do bind they produce cytokines. MHC 2 says hi yes we found a bad antigen we needa do something. MHC 1 is saying hi this is whats inside me, it could b good could b bad only boiinds to proteins different types for 1 n 2 |
|
|
Neutralization vs opsonization |
neutralization is that antibodies bind to proteins on the surface of a virus, bound antibodies prevent viral infection of a host cell, thus neutralizing the virus. Opsonization is antibodies that are bound to antigens on bacteria do not block infection, but instead present a readily recognized structure for macrophages or neutrophils, thereby promoting phagocytosis
|
|
|
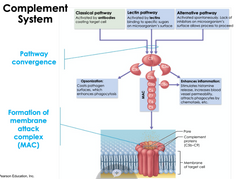
How exactly do complementary proteins help |
Binding of a complement protein to an antigen-antibody complex on a foreign cell triggers events leading to formation of a pore in the membrane of the cell. Ions and water rush
into the cell, causing it to swell and lyse. |
|
|
B cell immunogoblin and which is membrane bound |
IgA, IgD, IgE, IgG, and IgM. For a given B cell, each class has an identical antigen-binding specificity but a distinct heavy-chain C region. The B cell antigen receptor, known as IgD, is exclusively membrane bound. Other Ig are found in blood, tears, saliva and breast milk
|
|
|
Cytotoxic T cells |

part of the cell mediated immune response. They use toxic proteins (perforins that form pores in infected cell and granzymes that do aptosis) to kill cells infected. Activated by getting signaling from helper T cells n interaction w antigen presenting cell that have class I MHC molecules. Have accessory protein called CD8
memory cytotoxic t cell is alwasys wimmina round half active naive cant release cytokines activated by activated helper T cells or antigen presenting celkls |
|
|
Full adaptive immune response cycle |

|
|
|
Antibodies for each blood type |
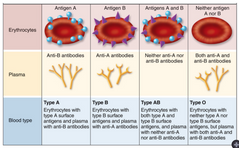
basically take ur blood type, ok thats the glucose chaons u have, anything besides urs is a threat to ur body n there fore theres antibodies for the other types in ur plasma
|
|
|
Anti a n anti b |
anti serum used to see if theres any antibodies interacting w antigen present. Antigen here would be the gluten chains on blood that make us a or b or ab or o
|
|
|
Rh and mothers |
mother makes antibodies to ababy but medically u can desensitize body to antigen aka baby. Reduce antibody
|
|
|
Vaccination what is it n who made it |
uses the idea of second immune response, Edward jennet saw that farmers that got coupon didn't get small pox, so now we use weak/inactivated/killed/weaker related pathogens. We eradicated smallpox this way
|
|
|
Active immunity vs passive immunity |
active is when a pathogen causes an immune response. Passive immunity is when antibodies made by another individual like fetus getting mom antibodies or artificial passive by injection
|
|
|
Monoclonal antibodies |
antibody clones of one epitope type antibosy (used in pregnancy tests)
|
|
|
Why are skin transplants rejects |
immune response where MHC molecules n it's membrane proteins have different genes, to reduce rejection donors w similar MHC molecules r looked for n medicine that suppresses immune system is taken
|
|
|
How does blood group in transfusions affect immune system |
blood cell glycoproteins are A, B, AB and O. A person with type A blood will respond to the bacterial epitope similar to the B carbohydrate and make antibodies that will react with any B carbohydrate encountered upon a transfusion. N cause lysis, triggering chills, fever, shock, and perhaps kidney malfunction. However, that same person doesn’t make antibodies against the bacterial epitope similar to the A carbohydrate because lymphocytes that would be reactive with the body’s own cells and molecules were inactivated or eliminated during development.
|
|
|
Allergies |
hypersensitive to allergens, most allergies are about IgE antibodies. Some IgE antibodies from b cell attach to mast cells and trigger histamine release. Antihistamines block receptors 4 histamine making symptoms less severe. Could cause anaphylacyic shock. Allergies r type 1 accute rapid response. Cause vasodilatipon. Epinephrin restores blood pressure
|
|
|
Anaphylactic shock |
Inflammatory
chemicals released from immune cells trigger constriction of bronchioles and sudden dilation of peripheral blood vessels, which causes a precipitous drop in blood pressure. Death may occur within minutes due to the inability to breathe and lack of blood flow. An injection of epinephrine rapidly counteracts this allergic response, constricting peripheral blood vessels, reducing swelling in the throat, and relaxing muscles in the lungs to help breathing |
|
|
Autoimmune diseases |
systemic lupus erythematosus, commonly called lupus, the immune system generates antibodies against histones and DNA released by the
normal breakdown of body cells. These self-reactive antibodies cause skin rashes, fever, arthritis, and kidney dysfunction. Other targets of autoimmunity include the insulin-producing beta cells of the pancreas (in type 1 diabetes) and the myelin sheaths that encase many neurons (in multiple sclerosis). Women r more likely. Regulatory T cells aka Tregs modulate system activity n prevent self antigens |
|
|
complement system |
blood has antimicrobial proteins
innate immunity complement system, liver makes inactive proteins. infection triggers activation All pathways (classical requires antibody so adaptive , but other 2 (lectin and alternative) are innate) start from C3 which is split into C3b makes opsonization and there's c3A enhancement of inflammatory response. Or c3B cytolysis which is membrane attack complex MAC. makes a ring/hole that makes cel lysys cuz water rushes in . Its self amplifying so its important to inactivate it fast. Inactivate thru inhibitors or instability of components of stuff in cascade they work together as cascade triggered by antibodies innate |
|
|
How does stress, sleep n exercise affect immune system |
light exercise helps immune system but too much to the point of exhasutiom leads to frequently being sick. Stress disrupts immune system hormones. Less sleep = more sick
|
|
|
Who evades innate immunity |
pneumonia bacteria, tuberculosis
|
|
|
Immunodeficiency disease |
immune system response to antigen is broken or gone. There inborn (ur born w it, genetic, ex> In severe combined immunodeficiency (SCID), functional lymphocytes are rare or absent. Lacking an adaptive immune response, SCID patients are susceptible to infections that can cause death in infancy, such as pneumonia and meningitis. Treatments include bone marrow and stem cell transplantation.) And there's acquired from exposure to stuff (Drugs used to fight
autoimmune diseases or prevent transplant rejection suppress the immune system, leading to an immunodeficient state. Certain cancers also suppress the immune system, especially Hodgkin’s disease, which damages the lymphatic system.) |
|
|
3 ways pathogens have evolved to avoid aimmune responses |
antigenic variation, latency, direct attack
|
|
|
Antigenic variations |
changing epitopes like flu or trypanosomiasis (sleeping sickness)
|
|
|
Latency |
infect cells then enter largely inactive state called latency, where no viral proteins r produced. Latency makes viral genome live in nucleus until favorable conditions for viral transmission are found. Ex is Herpes simplex viruses activated when sick like fever
|
|
|
HIV |
hiv infects helper Tcells binding to CD4 accessory protein, even when there's few CD4 like in brain n macrophage cells. Hiv rna is reverse transcribed and the product DNA integrated into host DNA to make new viruses. High mutation rate, kills n avoids adaptive immunity. Loss of helper t cells by aptosis (bad for humoral n cell mediated immune responses) gives u aids. Passed on thru fluids, can I fect others before they express symptoms
|
|
|
Aids |
acquired immunodeficiency deficiency syndrome, impaired immune responses, n leave u ready for infections. Some funguses that have no reaction for healthy ppl can cause death on ppl w aids.
|
|
|
Cancer |
when adaptive immunity is damaged u can get cancer easier, viruses are involved in 15% to 20% so since the immune system can recognize viral proteins as foreign, it can act as a defense against viruses that can cause cancer and against cancer cells that harbor viruses.
|
|
|
What virus can cause cancer in humans and any vaccines |
kaposis sarcoma Herpes virus, hepatitis B cause cancer and there's a human papillomavirus vaccine to reduce cervical n oral cancers
|
|
|
cells in adaprive vs innate immunity |

|
|
|
what cells r phagocytci in innate immunity |
macrophages, dedritic n neurtophils |
|
|
histamines vs cytakines |
Histamines only for allergies but r a first line defense, cytokines for inflammation r more adaptive n come later |
|
|
who destroys tumnor cells n cancer cells |
natural killer cells |
|
|
how do interferons work |
(from sick cells) stick to healthy cells |
|
|
how do helper t cells talk w B cells |
cytokines |
|
|
what happens if u switch a C part of heavy n light chains of antibodies |
Class switching, also known as isotype switching, is a process that allows B cells to change the class of antibodies they produce while retaining specificity for the same antigen. This process involves rearranging the DNA encoding the immunoglobulin heavy-chain constant (C) regions. The rearrangement of the heavy-chain C region DNA results in the production of antibodies with a different heavy-chain constant region, which determines the antibody's class or isotype (e.g., IgM to IgG).The process of class switching is essential for generating different types of antibodies with distinct effector functions. It occurs in response to signals from helper T cells and cytokines in the microenvironment and allows the immune system to tailor its antibody responses to specific types of pathogens and immune challenges |
|
|
NK cells vs cytotoxic t cells |
both use perforins n granules. NK is innate, Cytotoxic is adaprive. NK cells looks for cells lacking MHC1 and cytotoxic t cells look for antigen presenting MHC1 |
|
|
What section are recombination in b cell chains |
V and j J is joining but sloppy so not identical deletd neulotides between V and j In DNA |
|
|
Heavy vs light chain |
Heavy has VDJC Light has VJC |
|
|
What are the antigen presenting cells |
Have MHC2 complex Dendritic Macrophage Sometimes B cell NOT NEUTROPHILS |
|
|
B cell activated by? |
Only activated helper T cell so its BCR binds to a antigen, it consumes antigen n breaks it up present piece of antigen on an MHC 2 receptor so that a T cell can activate B cell |
|
|
T cells when activated do what signaling |
Paracrine n autocrine |
|
|
CD4 binds to |
MH2 only |
|
|
endogenous vs exogenous derived |
endogenous is made in cell MHC1 exogenous is not like antigens in blood MHC 2 |
|
|
specioficty for self |
apoptosis can retry again random of which on it is |
|
|
B cells can bind to vs t cells |
B cells DNA oligosachride carbohydrate peptide sequences T cells peptides |
|
|
memory cells |
half activted gene excpression so kinda like plasma kinda like original |
|
|
opsinization |
macrophage can bind to constant region of antibody |
|
|
leukocytes |
|
|
|
lymphoocytes |
b cells tcells phagocytic cells like macropahges |
|
|
somatic hyper mutations vs class switching |
somatic hyper mutations on the b cell once the b cell is activated (when u bind to antigen) then u refine the antigen binding site (the v region) class swithcing now that ur a free floating antibody. just changing constant region |
|
|
Rh - and Rh + |
rh - in mom no d antigen rh+ in bb maybe (could get from dad) yes d antigen moms body attacks baby cuz baby has d antigen rhodam inhibits immune |

