![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
60 Cards in this Set
- Front
- Back
|
Spirochetes |
Helical in shape long and thin axial filaments cannot be seen by compound microscope must use dark field microscope fragile easy to kill with antibiotics hard to grow in culture |
|
|
Treponema pallidum |
syphilis Sexually or congenitally (acquired at Birth) transmitted Features: Can't be seen by light microscopy Cannot be grown in vitro Very susceptible to heat and drying 2-3 week incubation |
|
|
Primary syphilis infection |
Chancre small hard based ulceration or sore for few days Painless. Many patients do not even know its there. |
|

Secondary syphilis |
Occurs 1 to 3 months later Appears as widespread skin rash even on palms Mild fever Lymphadenopathy (swollen lymph nodes) sore throat Myalgia (sore muscles) Highly infectious |
|

Tertiary syphilis |
May occur decades later Neurological symptoms Circulatory involvement and gummas(large lesions) Accommodation of pupils but no reaction to light (Argyll Robertson pupils)
Dorsal root column demyelination (tabes dorsalis) which causes sharp pains "slapped foot walking" |
|
|
Congenital syphilis |
May range from Intrauterine death Congenital abnormalities or silent infections which do not show up until about 2 years of age as facial and tooth deformities Transmission usually occurs after first trimesterMay range from Intrauterine death Congenital abnormalities or silent infections which do not show up until about 2 years of age as facial and tooth deformitiesDiagnosis by dark field microscopy answerologyNo vaccine . Penicillin for treatment Diagnosis by dark field microscopy answerology No vaccine . Penicillin for treatment |
|
|
Borrelia recurrentis |
Relapsing fever Transmitted through soft tick bites and body lice ***HALLMARK**** Recurring bouts of fever about 1 week apart. Features Endemic (indigenous) in rodents After 3-4 days incubation. Individual develops sudden chills and fever lasting about 3-5 days. Fever relapses are due to antigenic variation of the spirochetes. Diagnosis is by blood smear. Treatment: tetracycline |
|
|
Borrelia burgdorferi |
Lyme disease Transmitted by hard ticks SYMPTOMS: Diagnosis by serology difficult to see slow progressing 1 week incubationLater neurological and cardiac problems Later neurological and cardiac problems ****HALLMARK** Bulls eye skin lesion in 50% of cases. Arthritic symptoms otherwise. Treatment: tetracycline erythromycin and penicillin |
|
|
Campylobacter jejune |
Outbreaks of foodborne intestinal disease Transmission: foodborne Features Diarrhea abdominal cramps fever NO vomiting Associated with poultry milk and water Household pets may serve as a reservoir Invades GI epithelium and produces cytotoxin (bacterial toxins that kill host cells) Incubation: 2-11 days Duration: 3 Days To 3 weeksNo No No vaccine, self-limiting disease. |
|
|
Helicobacter pylori |
Gastritis ( inflammation of the stomach) and gastric ulcers Route of transmission unknown
Features Produces cytotoxins as well as ammonia as a result of urease to neutralize stomach acid in the localized regions of the colony. As colony grows the cytotoxins form and ulceration.
Responsible for 100% of all duodenal ulcers and 80% of peptic ulcers. The remaining 20% come from OTC drugs like NSAIDs.
Also strongly associated with stomach cancer
No vaccine , treat with antibiotics but not anti-acids b/c it will only exacerbate the growth of organism ****HALLMARK**** Responsible for almost all ulcers. Have been proven using Koch's postulates |
|
|
Gram-negative aerobic |
The pseudomonads (pseudomonas) Legionella pneumophila
Moraxella lacunata Bordetella pertussis Brucella melitensis Francisella tularensis
|
|
|
Pseudomonads (pseudomonas) |
Rod shaped with polar flagella and often produce defusable pigments Many are capable of growing at refrigerator temperatures and decomposing chemicals which kill moves microbes They can grow in soaps adhesives and even some antiseptics Resistant to a wide variety of antibiotics Very proficient opportunistic pathogenMany are capable of growing at refrigerator temperatures and decomposing chemicals which kill moves microbesThey can grow in soaps adhesives and even some antisepticsResistant to a wide variety of antibioticsAerobic but they are capable of anaerobic respiration using nitrate as a terminal electron acceptor because of this ability they contribute to the conversion of nitrates from soil into a form usable by plants Aerobic but they are capable of anaerobic respiration using nitrate as a terminal electron acceptor because of this ability they contribute to the conversion of nitrates from soil into a form usable by plants |
|
|
Pseudomonas aeruginosa |
Dermatitis (inflammation of the skin) outer ear infections infections of burns and cystic fibrosis patients
Route of transmission: waterborne direct contact nosocomial infections
Opportunistic pathogen Can colonize hair follicles and cause self-limiting rash Can be transmitted in pools hot tubs loofah sponges infected areas ****HALLMARK**** Fluorescent green pigment heavy pigment and very characteristic odor May exhibit blue green pus due to pigment very distinctive putrid grape like odor Vaccine: none |
|
|
Legionella pneumophila |
Legionnaires disease or legionellosis Respiratory route of transmission Colonize streams water lines and hospitals showers and cooling towers of air conditioning systems Grows in macrophages Legionnaires disease is an atypical pneumonia meaning it is not caused by the three leading bacterial agents it is severe and quickly fatal in older persons particularly smokers and heavy drinkers Also causes pontiac fever Vaccines: none |
|
|
Bordetella pertussis |
Whooping cough Respiratory route of transmission
3 stages of disease in children
1. Catarrhal stage- resembles a cold 2. Paroxysmal phase- accumulation of mucus in trachea and lungs causing characteristic whooping cough ****HALLMARK*** due to destruction of the MUCOCILIARY ESCALATOR 3. Convalescence phase- may last months
Vaccine: DTaP ( diphtheria tetanus and acellular pertussis) |
|
|
Convalescence phase Bordetella pertussis |
|
|
Moraxella lacunata |
Conjunctivitis (pink eye). One of the most common bacterial causes of pink eye.
Strictly aerobic coccobacillus Route of transmission is direct contact Strictly aerobic coccobacillus An inflammation the membrane that covers the eye and lines eyelidsVaccine:none Strictly aerobic coccobacillusAn inflammation the membrane that covers the eye and lines eyelidsVaccine:none An inflammation the membrane that covers the eye and lines eyelids Vaccine:none |
|
|
Brucella melitensis |
Brucellosis or undulant fever also known as Bangs disease, Malta fever, Rock fever of Gibraltar
Route of transmission: direct handling of infected animals
Nonmotile coccobacillus An obligate intracellular bacterium.
Zoonotic disease (non-human vertebrates are reservoirs, human are only accidental host)
Bacteria enter through skin or mucosa capable of surviving phagocytosis by macrophages Spread file limp to liver spleen or bone marrow
General weakness and tiredness ****HALLMARK*** known for abortion storms in pregnant cows
Vaccines: available for cattle and high-risk groups like Farmers ranchers beds and Meat Packers
treatment erythromycin and tetracycline |
|
|
Francisella tularensis |
Tularemia (rabbit fever) Route of transmission: spread to humans by handling infected meat or eating undercooked meat or deer fly bites. Respiratory route is less common
Plague like in animals Reservoir in small animals highly infectious ulceration at the site of entry then septicemia (bacteria in blood) swollen painful lymph nodes (buboe) and pneumonia Microbe resists phagocytosis
***HALLMARK**** Known for being zoonotic disease. Vaccine: live attenuated vaccine for high risk such as trappers. Ticks should be avoided. Streptomycin is drug of choice CANNOT be treated with Penicillin or cephalosporins |
|
|
Microaerophile |
An organism which requires reduced oxygen levels in carbon dioxide for growth. There are subtype of aerobe and absolutely require oxygen just in small amounts.
The best way to grow a microaerophile in the lab is in a Candle jar |
|
|
Gram-negative microaerophilic cocci |
Neisseria gonorrhoeae Neisseria meningitidis |
|
|
Neisseria gonorrhoeae |
Ophthalmia neonatorum, Gonorrhea and PID
Route of Transmission: via birth canal or sexually SYMPTOMS: Microbe is suceptible to drying and survives POORLY outside of human host. Transmission from female to infant during childbirth is seen as eye infection (opthalmia neonatorum) in newborns PID (pelvic Inflammatory disease) infection of uterus and uterine tubes. Incubation 2-7 days Binds to cells by fimbriae Males: Painful urination and pus discharge. ***HALLMARK** known as "drip" or "clap" Females: may be asymptomatic unless PID. may include salpingitis (uterine tube infection) and cervix infection. If left untreated endocarditis meningitis and arthritis can develop. |
|
|
BACTERIAL MENINGITIS |
More common than protozoan or fungal meningitis.
Progressive impairment of CNS leading to coma and death. Intense headaches photophobia fever and stiff neck Symptoms do not differ from viral fungal or protozoan meningitis BUT viral meningitis DOES NOT cause turbidity inCSF wheres as the others can.
It is tested for first because bacterial meningitis is also a faster killer and should be evaluated right way
|
|
|
Gram stain and culture must be performed on CSF. The leading causes of bacterial meningitis are... |
All three are microaerophilic 1.Neisseria meningitidis 2. Streptococcus pneumoniae 3. Haemophilus Influenza- requires blood |
|
Neisseria meningitidis |
Meningococcal meningitis Route of transmission: Grows in throats of healthy carriers spread by respiratory droplets Symptoms Once in blood organism crosses blood-brain barrier Symptoms due to endotoxin Diagnosis based on cultures made on blood agar incubated at reduced oxygen tension Cells look like coffee beans microscopically
10 - 15% mortality 10 - 15% experience long-term complications deafness mental retardation *****Hallmark**** RASH differentiates it from other meningitis causes VACCINE: purified capsular polysaccharide for some strains type A and C not B
Penicillin or cephalosporin first treatment maybe along with chloramphenicol, rifampicin for prophylaxis |
|
|
Facultative anaerobic gram-negative rods The 3 families discussed are... |
Enterobacteriaceae (enterics) Vibrionaceae Pasteurellaceae |
|
|
Enterobacteriaceae or enterics |
Inhibit intestinal tract of animals and are usually active glucose fermenters Many are motile with peritrichous flagella and have fimbriae Endotoxin is found in the outer membrane of all members of this group. It causes high fever and shock and activation of complement blood clotting inflammation and stimulation of immune cells through the release of cytokines Most have sex pili which are involved in genetic exchange particularly antibiotic resistance |
|
|
Bacteriocins |
Proteins causing lysis of related species of bacteria |
|
|
Some of the most important Genera of enterics are... |
Escherichia Salmonella Shingella Klebsiella serratia proteus yersinia Erwinia enterobacter |
|
|
Escherichia coli
|
Urinary tract infections and travelers diarrhea Route of transmission: fecal/oral route Presence of E coli in water and Foods is often an indication of fecal contamination Although it is not pathogenic many pathogenic strains exist organism is very opportunistic Major contributor of UTI Many strains produce enterotoxin which is associated which is associated with travelers diarrhea Vaccine:NONE |
|
|
Enterotoxin |
A bacterial toxin that causes inflammation of the stomach and intestine |
|
|
Most commonly produce toxins or virulence factors |
|
|
|
E. coli (O157:H7) |
The deadliest strain (jack-in-the-box) |
|
|
Salmonella species |
Salmonellosis Route of transmission: fecal/oral route Symptoms ****HALLMARK*** Causes 70% of all foodborne diarrheal diseases in the US SalmonellosisRoute of transmission: fecal/oral routeSymptoms****HALLMARK***Causes 70% of all foodborne diarrheal diseases in the USSource is often uncooked eggsNausea and abdominal painDiarrhea 12 to 36 hours after ingestionFever from endotoxin treatment- rehydration therapy SalmonellosisRoute of transmission: fecal/oral routeSymptoms****HALLMARK***Causes 70% of all foodborne diarrheal diseases in the USSource is often uncooked eggsNausea and abdominal painDiarrhea 12 to 36 hours after ingestionFever from endotoxin treatment- rehydration therapy SalmonellosisRoute of transmission: fecal/oral routeSymptoms****HALLMARK***Causes 70% of all foodborne diarrheal diseases in the USSource is often uncooked eggsNausea and abdominal painDiarrhea 12 to 36 hours after ingestionFever from endotoxin treatment- rehydration therapy Source is often uncooked eggs Nausea and abdominal pain Diarrhea 12 to 36 hours after ingestion Fever from endotoxin treatment- rehydration therapy |
|
|
Note to self |
It requires a large dose of salmonella to make you sick You only have to swallow one shingella to get extremely sick |
|
Salmonella typhi |
Typhoid fever Fecal/ oral
2 week incubation High fever headache diarrhea and malaise for 1 - 2 weeks ***HALLMARK**** Harbored in gallbladder of carriers. Carriers are treated by gallbladder removal 10% mortality if untreated
Vaccine: killed vaccine, ampicillin, chloramphenicol , cotrimoxazol, Ciprofloxacin |
|
|
Shigella dysenteriae |
Bacillary dysentery or shigellosis & travelers diarrhea Fecal/oral route Small dose required Invasion of ileum and colon causes bloody mucus diarrhea Abdominal cramps fever intense inflammation Also produces a neurotoxin ( bacterial toxin that affects the nervous system) 20% mortality if untreated No vaccine& antibiotics avoided because of high degree of resistance Hand-washing is prophylactic |
|
Klebsiella pneumoniae |
Urinary and respiratory tract infections Route of transmission: normal flora or by direct contact
Survives very well on hands Major cause of septicemia in children and ammonia and alcoholics
On The Rise may replace current as number 1 bacterial pneumonia cause.
no Vaccine. Very resistant to antibiotics aseptic technique and hand washing a prophylactic
Many Klebsiella infections are nosocomial and originated from objects like stethoscopes which are shared between patients without sanitizing. |
|
Yersinia pestis |
Bubonic plague and pneumonic plague
Route of transmission: flea bite and bubonic form, respiratory route for pneumonic form
SYMPTOMS W/ human-to-human transmission the LD50 is less than 1 Bruising and buboes Tet in streptomycin if administered promptly after exposure
Endemic in rodent populations
VACCINE: killed vaccine gives partial protection Prophylaxis by strict quarantine and rodent control and prophylactic antibiotics Zoonotic disease
In the pneumonic form, inhaling one cell results in death in 24 hours |
|
Yersinia enterocolitica |
Childhood diarrheal disease Route of transmission: contaminated water or foods, from dogs also possible
SYMPTOMS: Infect intestinal lining causing ulcerations spreads to lymph system. Where ulcerations also develop fever diarrhea and abdominal pain which may be mistaken for appendicitis arthritic symptoms May develop
VACCINE: self limits in 1 to 3 weeks antibiotics make speed recovery |
|
Vibrionaceae |
Comma shaped bacteria |
|
|
Vibrio cholerae |
Cholera Contaminated water or Foods
SYMPTOMS: Causes profuse watery diarrhea RICE WATER STOOLS Produces exotoxin a toxin secreted by bacteria which Alters membrane permeability of intestinal mucosa and causes massive watery diarrhea 3 - 5 gallons a day and vomiting Fever usually absent incubation 3 days symptoms last several days 50% mortality if untreated Death results from severe dehydration
300,000 people died of Cholera in Rwanda in 1995.
Vaccine: Tetracycline shortens the symptoms a whole cell vaccine is available but of limited use |
|
|
Vibrio parahaemolyticus |
Gastroenteritis (inflammation of stomach and intestine) Route of transmission: raw or uncooked shellfish SYMPTOMS: Produces excitotoxin in hemolysin Diarrheal disease with abdominal pain Burning sensation nausea vomiting watery stool prevented by cooking fish symptoms after 24 hours No vaccine, without treatment recovery in a few days, rehydration therapy rarely |
|
|
Pasteurellaceae |
Haemophilus influenzae capsular type B (Hib) Meningitis, ear aches, epiglottis, septic arthritis, bronchitis and pneumonia Airborne transmission Haemophilus species commonly inhabits mucous membranes of the upper respiratory tract, mouth, vagina and intestinal tract of humans. Acute otitis media is caused by this organism and often follows viral upper respiratory tract infections. Leading cause of epiglottis in children who are not vaccinated Epiglottis may swell and cause Airway obstruction H. Influenzae is now the 3rd most common bacterial meningitis in children Progressive CNS infection leading to blindness Karma deafness , paralysis, mental retardation (35%) and sometimes death. Species lack the cytochrome system necessary for respiration and must be supplied with blood hemoglobin in order to grow. Type B is most common (six types total) VACCINE: one directed against the capsular polysaccharide is available,HibTITER given to infants may also be given as Tetra immune vaccine which is diphtheria pertussis and tetanus combined ampicillin for non beta-lactamase producers cephalosporin or chloramphenicol as alternatives rifampicin recommended as prophylactic New convex vaccine provides children with protection against him and hepatitis B virus combined |
|
|
Gardnerella vaginalis |
Vaginitis( inflammation of the vagina) Normal floor and most women or their sexual partners SYMPTOMS Sensitivity to PH changes foul odor and discharge facultativly anaerobic Rod grouping Also classified with gram-negative facultative anaerobes in text consider a gram variable organism |
|
|
Coxiella burnetii |
Q fever Transmitted by Aerosoles from animals or by contaminated milk from cows
SYMPTOMS
*****HALLMARK*** Organism the only known gram-negative endospore producer
NOT transmitted by insects like other rickettsias Resistant to drawing heat and sunlight
VACCINE Two vaccine available for high-risk groups ,killed pasteurization, and antibiotic therapy available |
|
|
Rickettsia Prowazekii |
Epidemic typhus Transmitted in the feces of human lice Symptoms include rash prolonged high fever and stupor Treatable with antibiotics |
|
|
Rickettsia typhi |
Endemic Marine typhus (NOT the same as typhoid fever caused by salmonella) Route of transmission: rat fleas Symptoms are less severe disease is usually self-limiting |
|
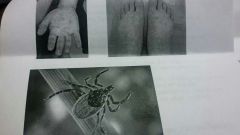
Rickettsia rickettsii |
Rocky Mountain spotted fever
Transmitted by tick bite Multiply inside host cell's cytoplasm
Damage to the permeability of capillaries and potential collapse of the cardiovascular system
Cause of rash similar to measles but also on the soles and Palms( viral infections do not produce rash here)
Death a result of kidney and heart failure
NO VACCINE: treatment Tet and Horan phenocal very effective early |
|
|
Chlamydia trachomatis |
Trachoma infection of the conjunctiva of the eye Karma non-gonococcal urethritis, PID and lymphogranuloma venereum
Route of transmission: STD or transmitted by direct contact
SYMPTOMS: Scar tissue forms on cornea the leading infectious cause of blindness in the world most commonly transmitted sexually transmitted leading cause of infertility 75% of females are often asymptomatic Advanced infections become LGV with buboes often ruptured strictures and fistulas
No vaccine treatment includes tetracycline and erythromycin fluoroquinolones useful |
|
|
Chlamydia pneumoniae |
Pneumonia , atherosclerosis? Transmitted by respiratory route Symptoms: Typical symptoms of pneumonia Organism found in 90% of coronary arteries with atherosclerotic plaque and only 4% of patience with no atherosclerosis |
|
|
Bacteria without cell walls Mycoplasma pneumonia
|
Primary atypical pneumonia Respiratory route
Known as "walking pneumonia" contains no peptidoglycan (hard to treat) but does have outer membrane cells attached to ciliated Repertory epithelium in the respiratory tract last four weeks but is usually not severe enough to require hospitalization
VACCINE:none, treat with Tet and erythromycin |
|
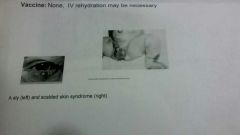
Staphylococcus aureus |
GRAM POSITIVE COCCI Folliculitis impetigo , sty, boils , carbuncles, post-operative infections, catheter infections
Scald Skin Syndrome TSS Staphylococcal food poisoning Route of transmission: normal flora and post-op infections |
|
|
Streptococcus pyogenes |
strep throat Ear, sinus and tonsil infections Puerperal sepsis Impetigo in older children and adults Erysipelas (red skin discoloration)
SCARLETT FEVER & RHEUMATIC FEVER
Respiratory route or direct contact
Beta hemolytic |
|
|
Alpha hemolytic |
Species produce Alpha hemolysis which reduces hemoglobin (red) to methoglobin (green) Resulting in a greenish Zone around the colonies |
|
|
Beta hemolytic |
Produce hemolysin which forms a clear Zone when blood cells are lysed |
|
|
Gamma hemolytic |
Have NO apparent hemolysis |
|
|
Scarlet fever versus rheumatic fever |
Scarlet fever toxic Gene carried on a prophage causes rash which is pinpoint and rough sandpaper to the touch strawberry tongue is red enlarged and roll followed by desquamation Rheumatic fever is caused by reactive antibodies between strep and heart. Endocarditis is infection of inner lining of the heart tissues acute glomerulonephritis inflammation of the kidney and inflammation streptococci are usually absent point anti-inflammatory drugs are given |
|
|
Streptococcus pneumoniae |
Pneumococcal pneumonia Respiratory droplet transmission
Symptoms Normal flora at sometimes . 4% of population are carriers Capsulated
Sickle Cell patients are more susceptible, increase susceptibility due to atrophy of the spleen 15% mortality Second most common cause of bacterial meningitis in children and young people but one of the fastest to kill can kill within 24 hours.
Most common cause of meningitis in adults
VACCINE: Capsular polysaccharide vaccine, penicillin treatment of choice for sensitive strains HALLMARK*** Rust colored sputum is a Hallmark feature of this organism. Of course blood-tinged sputum can be seen in other diseases such as TB but note that strep infections are more common than mycobacterium infections. Streptococcus pneumoniae can also kill in 24 hours especially if it transitions into meningitis |
|
|
Enterococcus faecium and faecalis |
urinary tract infections, endocarditis, post-op infectionsSYMPTOMSFrequent painful urination, difficulty voiding bladder, cloudy foul smelling urine, blood in urine, abdominal pain, feverDiagnosed by urine culture inflammation of heart liningNO VACCINE.Antibiotic therapy, many strains resistant to Vancomycin (VRE) |

