![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
42 Cards in this Set
- Front
- Back
|
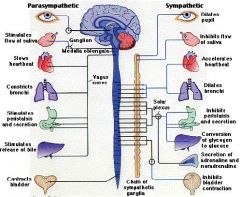
ANS overview
|
|
|
|
SNS Preganglionic Fibres Neurons to...
|
–Paravertebral ganglia; paired, bilaterally along vertebral column
3 cervical, 11 thoracic, 4 lumbar, 4 or 5 sacral –Prevertebral ganglia : midline, anterior to aorta, spinal column coeliac, aorticorenal and mesenteric –previsceral ganglia; small collections of sympathetic ganglia located close to target structures |
|
|
NTs in SNS
|

|
|
|
Parasympathetic nervous system
|
•Craniosacral outflow
•Cranial nerves III, VII, IX, X –CN III fibres Edinger-Westphal nucleus midbrain, periphery of CNIII, exit with nerve to IO, ciliary ganglion –Preganglionic fibres for VII from superior salivary nucleus, leave VII at geniculate ganglion –DMV in medulla preganglionic fibres to essentially all organ systems in chest and abdomen •Sacral cord levels 2,3,4 –Cell bodies intermediolateral cell column –Postganglionic fibres to bladder and bowel and reproductive organs |
|
|
Ganglia in ANS
|

|
|
|
Effects of ANS on organs
|

|
|
|
Horners Syndrome
- causes |
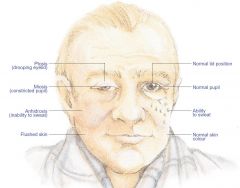
causes horners:
- vascular - physical damage to the sympathetics along the course (mesh along the carotid, lesion in the brain stem, along T1, or paravertebral length...) |
|
|
Course of Sympathetics to the eye
- lesion sites |

|
|
|
MVA horners syndrome + neck pain
|
think carotid dissection
|
|
|
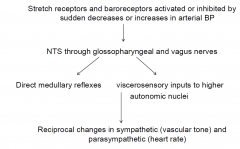
Cardiovascular reflexes: easily tested in clinical setting
|
Parasympathetic
•Heart rate response to deep breathing (vagal afferent and efferents) •Heart rate response to Valsalva (INC> thoracic pressure thus DEC. VR) Sympathetic •Blood pressure response to postural change (eg tilt-up) •Heart rate response to postural change •Blood pressure response to Valsalva |
|
|
Baroreceptor Reflex
|
|
|
|
Normal Tilt table test
|
Slight inc. in HR AND BP
|
|
|
COnvulsive Syncopy
|
if the BP is low for long enough
- eg faint and dont get flat quick enough |
|
|
Causes of Syncopy
|
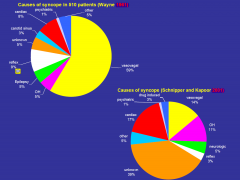
|
|
|
Vasovagal
|
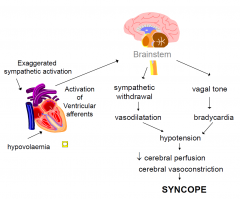
called a vasovagal due to bardycardic response BUT in fact the cause is due to the abrupt withdrawal of SNS that actually causes it and not the vagus
|
|
|
Key historical points in the evaluation of
syncope |
• Situation
• Prodrome – diaphoresis, warmth, lightheadedness – focal neurological deficit – chest pain, shortness of breath – Witness reports • Witness reports • Post event residua • Past history • Family history • Medications |
|
|
Current investigations used to assess syncope
|
• thorough history , examination and ECG yields a
diagnosis in 50% • Ambulatory ECG monitoring • ECHO • Exercise testing • EPS • Tilt table testing • Other – EEG – coronary angiography |
|
|
Tilt testing: indications
|
Established
• Recurrent unexplained syncope • Single episode in high risk individuals • Further evaluation where a cause is established but where NMS would affect treatment plans Debated • convulsive syncope vs seizures • recurrent unexplained falls • follow up evaluation to assess therapy of NMS Not warranted • single episode of syncope with clear vasovagal features • syncope with established cause where NMS would not effect therapy Much better test than active staning (using muscles) but not v.specific because some normal people will faint |
|
|
Tilt testing: method
|
• fasting vs non, IV hydration vs not
• beat to beat blood pressure recordings • 60-80% head up tilt • 30-45 min initial drug free tilt • ?? Role of provocative medication (isoprenaline, nitroglycerin, clomipramine) • reproducibility varies (35-85% most studies 65-85%) |
|
|
Tilt testing: optimum duration
|
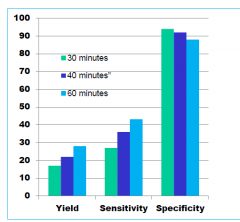
|
|
|
SNS Syncopy
|
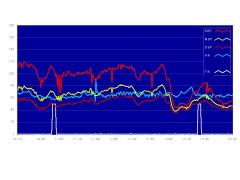
no drop in HR just abrupt withdrawal of SNS causing the syncopy
|
|
|
Mixed SNS and PSNS Syncopy
|
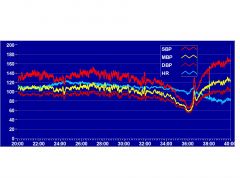
|
|
|
Treatment of neurally mediated syncope
|
•Nonpharmacologic: salt and water loading, resistance training lower limbs
•Beta blockade (blocks the INC. HR that initates the problem) •Fludrocortisone •SSRIs •Adrenergic agonists •cardiac pacing for refractory vasovagal (not vasodepresor) |
|
|
•48F
•20year history of diabetes •Lightheadedness on standing, presyncope with prolonged standing •Constipation, reflux, bloating after meals •Marked face sweating with minimal exertion, extreme fatigue in hot weather •Problems driving at night |
- baroreceptors not working
- GI dysmotility - can only sweat in her face (peripheral neuropathy and so the ANS is affected and always the long nerves are always affected first - chronotropic fibres still functioning, they are short fibres |
|
|
Autonomic neuropathy WITHOUT somatic neuropathy
|
–acute pandysautonomia (post infection)
–subacute autonomic neuropathy- autoimmune autonomic ganglionopathy, paraneoplastic autonomic neuropathy –Limited cholinergic neuropathy- chronic anhidrosis, chronic enteric neuropathy |
|
|
Autonomic Neuropathy + Somatic neuropathy
|
–Diabetes (danger is that these people lose the Sx recognition fro hypoglaceamic attacks)
–Amyloidosis (primary and secondary) –Guillain Barre Syndrome –Porhyria –Familial dyautonomia, hereditary sensory and autonomic neuropathy |
|
|
Autonomic neuropathy Sx
|
•Postural lightheadedness
•Heat intolerance •Erectile dysfunction •GI dysmotility- bloating, constipation, diarrhoea •Bladder dysfunction- retention, incontinence •Glare sensitivity |
|
|
Acute autonomic neuropathies
|
•Acute pandysautonomia
–paraneoplastic –idiopathic •Botulism •GBS •porphyria •drugs and toxins |
|
|
Acute pandysautonomia
|
•various restricted forms
–acute cholinergic neuropathy –postural tachycardia syndrome –GI motility disorders •many likely to be immune mediated •recovery usually only partial •reports of response to IVIG, PEx, steroids •may follow viral or other febrile illness (? 50%) •uncommon •acute or subacute onset •widespread sympathetic and parasympathetic failure •rarely pure autonomic but relative sparing of somatic fibres CASE: •24F •Well until July 2011 •Presumed viral illness with high fevers, myalgia •2 weeks later –severe abdominal bloating –Constipation –Sensitivity to light –Marked heat intolerance –Postural lightheadedness |
|
|
Subacute autonomic neuropathies
|
•paraneoplastic
•autoimmune •diabetes •drugs and toxins |
|
|
Chronic autonomic neuropathies
|
•amyloid
•Diabetes •chronic pandysautonomia (paraneoplastic,idiopathic) •sensory neuronopathy with autonomic failure (idiopathic, paraneoplastic, Sjögrens) •pure autonomic failure •familial dysautonomia |
|
|
Chronic autonomic neuropathies
PAtterns |
•Distal sympathetic
–small fibre neuropathy –other peripheral neuropathies •Cholinergic –LEMS –chronic idiopathic anhidrosis –Adie's, Chagas’ •Adrenergic –(inc DßH deficiency, NGF deficiency) |
|
|
Anhydrosis above T1
|

horners
|
|
|
Sweating on one side of the face
|
classic medullary stroke
- vertigo - hiccups - slurred speech - horners syndrome |
|
|
Multiple Systems Atrophy
|
•Striatonigral
•Olivopontocerebellar •Pyramidal •Natural history: usually do not survive more than 6-8 years •Prevalence 5-15 per 100,000 •Onset middle to old age (two large series median 53, range 33-76) •M:F 2:1 •Most common presentation autonomic failure and parkinsonism Rigidity and bradykinesia> tremor No, poor or poorly sustained response to l-dopa (?29% respond at some stage, maintained in only 13%) Mild cerebellar or pyramidal signs may be present •OH is the rule: present at first evaluation or within a year of development of parkinsonism |
|
|
Orthostatic Hypotension
|
Symptoms
–Often vague : blurred vision, neck ache , muddled thinking etc –Worse on first arising (esp after excessive nocturia), after meals (always worse after meals or EtoH due to excess vasodilation) , in heat, with exercise, with duration of standing Treatment: •non pharmacological measures –elevation of head of bed (brain gets used to the lower BP thus in the morning there isnt the big drop) –physical manoeuvres –compression garments •Fludrocortisone •sympathomimetic agents –ephedrine, psuedoephedrine – midodrine (selective alpha agonist) •non specific pressor agents – caffeine, ergot derivatives, somatostatin analogs •prostaglandin synthetase inhibitors, indomethacin, ibuprofen |
|
|
Pure Autonomic Failure DDx
|
•Major differentials MSA and Parkinsonism
•Absence of neurological findings (NB autonomic features may be the first signs in MSA too so serial assessment needed):No cerebellar, pyramidal or extrapyramidal features •Low supine plasma NA with little increase on standing and marked response to infusion •PAF less progressive and generally less disabling, slow if any progression over 10-15 years • Disease of peripheral (postganglionic, predominantly sympathetic) ANS |
|
|
Carotid Sinus Hypersensitivity
|
more common in elderlydue to atherosclerosis changes
- in young people the have to have a more toght collar or something else to provoke it - massage of caotids drops BP and HR |
|
|
small fibre neuropathy: causes
|
•idiopathic
•impaired glucose tolerance •diabetes •HIV neuropathy •amyloid •paraneoplastic neuropathy •paraproteinaemic neuropathy •hereditary neuropathies |
|
|
small fibre neuropathy: symptoms
|
•characteristically constant burning pain: superficial, mainly soles of feet, worse at night (or at rest- when there are no other inputs))
•prickling sensations, sometimes itch •lancinating pains usually starting in feet and shooting up legs •dull, deep seated aching pain in the feet •episodic abnormal heat/cold sensation •allodynia (light touch becomes painful) |
|
|
small thinly myelinated Ad and unmyelinated C fibre dysfunction
|
–disturbed pain and temperature sensation
–dysesthesia, burning pain –disturbed autonomic function |
|
|
•large myelinated fibre (Aa, Ab) dysfunction
|
–numbness, hypoesthesia, reduced proprioception and vibration
–reduced deep tendon reflexes –variable motor deficit |

