![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
208 Cards in this Set
- Front
- Back
|
SE of Mg sulfate?
|
A therapeutic magnesium level is between 4-7 mEq/L. Loss of deep tendon reflexes occurs at a level of 7-10 mEq/L. Respiratory depression may occur at levels above 12 mEq/L. Cardiac arrest may occur at a level of 15 mEq/L. Seizures are prevented by the use of magnesium. Pulmonary edema can occur with magnesium therapy, but is not related to toxicity from the drug.
|
|
|
A 31-year-old G3P0 woman at 27 2/7 weeks is undergoing expectant management for severe preeclampsia remote from term. Her blood pressure is 155/100 on methyldopa 500mg three times a day. Her recent 24-hour urine had 6.6g of protein. An ultrasound revealed a fetus with adequate growth, having an estimated fetal weight in the 10th percentile. Her labs are normal, except for a uric acid of 8.0, hematocrit of 42% (increased from 37%,) and a platelet count of 97,000. Which of these findings necessitates delivery at this time?
|
Thrombocytopenia <100,000 is a contraindication to expectant management of severe preeclampsia remote from term (<32 weeks). Other contraindications include: inability to control blood pressure with maximum doses of 2 antihypertensive medications, non-reassuring fetal surveillance, liver function test elevated more than 2 times normal, eclampsia, persistent CNS (central nervous system) symptoms and oliguria. Delivery should not be based on the degree of proteinuria. Although elevated uric acid and hemoconcentration are markers of preeclampsia, they are not part of the diagnostic or management criteria
|
|
|
monitoring fetuses w/ IUGR?
|
While fetal kick counts may be of value, additional fetal testing such as twice weekly NST with AFI and weekly umbilical artery Doppler studies is indicated in monitoring fetuses with IUGR
|
|
|
In order to accurately confirm gestational age at term
|
one of the following criteria should be met: Fetal heart tones have been documented for 20 weeks by a non-electronic fetoscope or for 30 weeks by Doppler; it has been 36 weeks since a positive serum or urine HCG pregnancy test was performed by a reliable laboratory; an ultrasound measurement of the crown-rump length, obtained at six to twelve weeks, supports a gestational age of at least 39 weeks; and an ultrasound obtained at 13-20 weeks confirms the gestational age of at least 39 weeks, determined by clinical history and physical examination. The crown-rump length can reliably date a pregnancy within five to seven days.
|
|
|
IUGR risk factor for?
|
Subsequent development of cardiovascular disease, chronic hypertension, chronic obstructive lung disease and diabetes.
|
|
|
A 4th degree laceration
|
involves the rectal sphincter and rectal mucosa. Careful attention to identification and repair of the disrupted ends of the sphincter is important to try to minimize the risk of future fecal or flatus incontinence.
|
|
|
A 1st degree laceration
|
involves only the vaginal mucosa
|
|
|
A 2nd degree laceration
|
involves the vaginal fascia and perineum.
|
|
|
A 3rd degree laceration
|
involves the rectal partial or complete transection of the rectal sphincter
|
|
|
Forceps application requires
|
complete cervical dilation, head engagement, vertex presentation, clinical assessment of fetal size and maternal pelvis, known position of the fetal head, adequate maternal pain control and rupture of membranes
|
|
|
tubal ligation complication?
|
future pregnancy
|
|
|
CVS performed?
|
10 - 12 weeks - loss rate 1-3%
|
|
|
Amniocentesis?
|
15 weeks - loss rate = 0.5%
|
|
|
Squamous cell carcinoma is the most common vulvar malignancy and may arise in the setting of chronic irritation from lichen sclerosus. Tx?
|
Given the findings of obvious, moderately differentiated carcinoma, definitive treatment can be recommended with radical vulvectomy and groin node dissection.
|
|
|
Squamous cell carcinoma
|
accounts for approximately 90% of vulvar cancers. Patients commonly present with a lump and they commonly have a long-standing history of pruritus. The chronic itch-scratch cycle of untreated lichen sclerosus, or any other chronic pruritic vulvar disease, is thought to stimulate the development of squamous carcinoma. The mean age of squamous cell carcinoma is 65 years and smoking is known to increase the risk of development of vulvar cancer, especially in the setting of HPV infection
|
|
|
LIchen sclerosis
|
the skin appears thin, inelastic and white, with a “crinkled tissue paper” appearance
|
|
|
Paget's dz of the vulva
|
associated with white plaque-like lesions and poorly demarcated erythema, not a discrete mass; lacy white mottling of the surface
vulva is fiery red background mottled with whitish hyperkeratotic areas without a distinct lesion. No nodularity or tenderness is noted. |
|
|
Verrucous carcinoma
|
cauliflower-like lesions
|
|
|
Melanoma
|
presents as pigmented lesion
|
|
|
Molluscum, a poxvirus
|
characterized by multiple shiny non-pigmented papules with a central umbilication
|
|
|
Hidradenitis suppurativa
|
chronic, unrelenting skin infection causing deep, painful scars and foul discharge.
|
|
|
A 38-year-old G3P3 presents to the office because she has noted dark spots on her vulva. She states that the lesions have been present for at least two years and are occasionally itchy. She has a history of laser therapy for cervical intraepithelial neoplasia ten years ago, and has not had a pelvic exam since then. She has had multiple partners and uses condoms. Smoked since 14 yo. On examination, multicentric brown-pigmented papules are noted on the perineum, perianal and labia minora. No induration or groin nodularity is noted.
|
This presentation is classic for human papilloma virus (HPV) related VIN 3.
|
|
|
Post-menopausal. On examination, she is noted to have a somewhat firm and somewhat fixed, non-tender 4 cm mass in her labia majora at the level of the bartholin’s gland on the right. There is no associated erythema or discharge, and the remaining vulvar exam and pelvic exam are unremarkable.
|
The finding of a mass in the Bartholin’s gland is highly suspicious for malignancy and requires excision/biopsy, especially in a post-menopausal women. The histology is typically adenocarcinoma.
|
|
|
A 45-year-old G3P3 presents to the office because of a large dark spot on her vulva. She states that the lesion has been present for at least two years and is occasionally itchy. She has smoked since age 20.On examination, a 2.5 cm lesion is noted. No induration or groin nodularity is noted. The vagina and cervix appear normal. There are no additional lesions noted on colposcopic examination of the vulva. A biopsy of the lesion returns as vulvar intraepithelial neoplasia grade 3 (VIN 3).
|
VIN III should be treated with local superficial excision.
|
|
|
A 34-year-old G2P2 presents with biopsy-proven vulvar intraepithelial neoplasia, grade 2 (VIN 2). She is sexually active, and is concerned about the impact this will have on her sex life. Examination confirms multiple, whitish raised 0.5 – 1.5 cm papules throughout her labial minora, majora, clitoral hood and perineum. Which of the following is the most appropriate treatment option for this patient?
|
CO2 laser ablation of the lesions
|
|
|
if cervical biopsies show severe dysplasia, carcinoma in situ or if a patient has a positive ECC.
|
cervical conization
|
|
|
Indications for cervical conization
|
unsatisfactory colposcopy, including inability to visualize the entire squamocolumnar junction, positive endocervical curettage
|
|
|
A 28-year-old, has HSIL. She smokes one pack of cigarettes per day. Colposcopy is performed. The cervix is noted to have an ectropion and there is abundant aceto-white epithelium. Mosaicism, punctations and several disorderly, atypical vessels are noted. Several biopsies are obtained and sent to pathology. Which of the findings on this patient’s colposcopy is most concerning?
|
Atypical vessels usually represent a greater degree of angiogenesis and, thus, usually a more concerning lesion.
Punctations and mosaicism represent new blood vessels on end and on their sides, respectively. An ectropion is an area of columnar epithelium that has not yet undergone squamous metaplasia. It appears as a reddish ring of tissue surrounding the external os. Acetowhite epithelium can represent dysplasia but, in most cases, is less concerning than the above vascular changes. |
|
|
HIV women
|
Women with HIV have higher rates of cervical dysplasia and invasive cancer than do women without HIV. Treatment failures and recurrences are more frequent, and disease severity correlates with decreasing CD4 counts. A Pap smear should be obtained twice in the first year after diagnosis of HIV infection and, if the results are normal, annually surveillance can resume.
|
|
|
risks for cervical cancer
|
include early-onset sexual activity, multiple sexual partners, a sexual partner with multiple partners, history of HPV or other sexually transmitted diseases, immunosuppression, smoking, low socioeconomic status and a lack of regular Pap smears.
|
|
|
MC symptom of leiomyoma
|
menorrhagia
secondary to: 1) an increase in the uterine cavity size that leads to greater surface area for endometrial sloughing; and/or 2) an obstructive effect on uterine vasculature that leads to endometrial venule ectasia and proximal congestion in the myometrium/endometrium resulting in hypermenorrhea. Other relatively frequent symptoms include pain and pressure symptoms related to the size of the tumors filling the pelvic cavity, as well as causing pressure against the bladder, bowel and pelvic floor. |
|
|
Myomectomy (removal of the fibroid) during pregnancy is contraindicated.
|
Myomectomy at the time of Cesarean section should be avoided, if possible, secondary to the risk for increased blood loss. It is not necessary to follow the growth of fibroids during pregnancy, except for the rare cases when the fibroid is causing symptoms (primarily pain) or appear to be located in a position likely to cause dystocia
|
|
|
Which type of fibroid is more likely to cause subfertility?
|
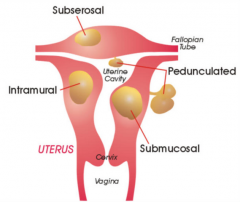
SUBMUCOSAL.
Submucosal myomas are most likely to cause infertility. Presumed mechanisms include: 1) focal endometrial vascular disturbance; 2) endometrial inflammation, and; 3) secretion of vasoactive substances. Submucosal fibroids are best treated by hysteroscopic resection. |
|
|
Her endometrial biopsy is negative. She is interested in the medical options for treating symptomatic uterine fibroids. What is the next best step in the management of this patient?
|
Growth of uterine fibroids is stimulated by estrogen. Gonadotropin-releasing hormone agonists inhibit endogenous estrogen production by suppressing the hypothalamic-pituitary-ovarian axis. They can result in a 40-60% reduction in uterine size. This treatment is commonly used for three to six months before a planned hysterectomy in an attempt to decrease the size of the uterus, which may lead to a technically easier surgery and decreased intraoperative blood loss.
|
|
|
A 50-year-old G3P3 complains of menorrhagia. Physical examination is notable for a 14-week size irregularly shaped uterus. Her hematocrit is 35%. Which of the following is the next most appropriate step in this patient’s management?
|
Endometrial sampling
The majority of patients with uterine fibroids do not require surgical treatment. If patients present with menstrual abnormalities, the endometrial cavity may be sampled to rule out endometrial hyperplasia or cancer. This is most important in patients in their late reproductive years or postmenopausal years. Particularly in a perimenopausal woman, it is important to first rule out an underlying endometrial malignancy with endometrial sampling. |
|
|
A 39-year-old G1P1 comes to see you because of increased bleeding due to her known uterine fibroids, especially during her menses. She reports that her bleeding is so heavy that she has to miss two days of work every month. She has been using oral contraceptives and NSAIDs. Her most recent hematocrit was 27%. She is undecided about having more children. You discuss with her short and long-term options to decrease her bleeding. What is the next best step in the management of this patient?
|
The goals of medical therapy are to temporarily reduce symptoms and to reduce myoma size. The therapy of choice is treatment with a GnRH agonist. The mean uterine size decreases 30-64% after three to six months of GnRH agonist treatment. Even though she is anemic, she is asymptomatic and able to work so a blood transfusion will not be indicated. Although uterine artery embolization and endometrial ablation effectively reduce bleeding, pain and fibroid size, they are contraindicated in a patient who desires future fertility. The failure rate is about 10-15%. A hysterectomy would obviously take care of her bleeding but would not be performed if she desires future fertility.
|
|
|
What can you inform her about the response of the fibroids after the cessation of GnRH agonist therapy?
|
Maximal response is usually achieved by three months of GnRH agonist treatment. The reduction in size correlates with the estradiol level and with body weight. Hot flashes are experienced by >75% of patients, usually in three to four weeks after start of treatment, although they should not persist for longer than one to two months from end of treatment. After cessation of treatment, menses return in four to ten weeks, and myoma and uterine size return to pretreatment levels in three to four months. The regrowth is consistent with the fact that reduction in size is not due to a cytotoxic effect. However, it is not true that secondary to the GnRH agonist withdrawal they will grow at a more rapid rate.
|
|
|
A 48-year-old G2P2 complains of progressively heavier and longer menstrual periods over the last year. Prior to this year the patient had normal periods. She denies any symptoms other than fatigue over the last few months. Physical examination is unremarkable except for the pelvic examination. The patient is noted to have an irregularly shaped 16-week size uterus. The patient’s hematocrit is 28%. What is this patient’s most likely diagnosis?
|
Uterine fibroids
The patient’s history and physical examination is typical for a perimenopausal woman with probable uterine fibroids. Although it is possible that she could have underlying endometrial hyperplasia, the most likely diagnosis is uterine fibroids. Uterine leiomyosarcoma should be considered in a postmenopausal woman with bleeding, pelvic pain coupled with uterine enlargement, and vaginal discharge, but it is exceedingly rare. Endometrial hyperplasia is more common in perimenopausal women who do not ovulate regularly and postmenopausal women. Endometrial carcinoma is typically a disease of postmenopausal women, although 5-10% of cases occur in women who are menstruating and 10-15% of cases occur in perimenopausal women. Adenomyosis may result in a symmetrically enlarged “boggy” uterus, but usually presents with dysmenorrhea in addition to menorrhagia. |
|
|
A 31-year-old G0 has been diagnosed with uterine fibroids. A fluid contrast ultrasound confirmed the presence of two intramural fibroids measuring 5 x 6 cm and 2 x 3 cm that appear to be distorting the patient’s uterine cavity. The patient has a two-year history of infertility. She has had a thorough infertility work up. No etiology for her infertility has been identified. Which of the following treatments is most appropriate for this patient?
|
Myomectomy is warranted in younger patients whose fertility is compromised by the presence of fibroids that cause significant distortion of the uterine cavity. A myomectomy may be indicated in infertility patients when the fibroids are of sufficient size or location to be a probable cause of infertility and when no more likely explanation exists for the failure to conceive.
|
|
|
Endometrial cancer risk factors
|
Endometrial cancer is a gynecologic malignancy that has easily identifiable risk factors and typically presents with symptoms that lead to an early diagnosis. Risk factors include nulliparity, obesity, late menopause, hypertension and exposure to unopposed estrogens.
|
|
|
Which of the following findings is most concerning for presence of endometrial cancer?
|
Vaginal bleeding.
The most common symptom is abnormal postmenopausal bleeding. However, other symptoms or clinical findings that may be seen include abnormal vaginal discharge and lower abdominal discomfort. Endometrial cancer can increase the size of the uterus as it grows, but is usually not the most common finding given the early diagnosis of this cancer. Unopposed estrogen replacement therapy does increase the risk, but not when taken in combination. Early menarche and late menopause are additional risk factors that may be related to endometrial cancer development. |
|
|
A 65-year-old G2P1 has been referred to you for further evaluation of postmenopausal bleeding. Similar episode 2 months ago. A transvaginal ultrasound showed a homogeneous endometrial lining measuring 3.5 mm. A subsequent office endometrial sample was obtained and returned scant tissue with rare atypical cells. What is the most appropriate next step in the management of this patient?
|
The incidence of endometrial cancer in postmenopausal women with irregular bleeding ranges from 4% to 25%. More importantly, of the women ultimately diagnosed with endometrial cancer, 90% report a history of vaginal bleeding. The diagnostic test of choice is the office endometrial sampling, which has a detection rate as high as 99% in postmenopausal women. In a woman who has persistent symptoms or findings suggestive of an underlying endometrial malignancy, as does this patient with atypical cells on endometrial biopsy, further investigation with dilation and curettage is warranted.
|
|
|
A 62-year-old G0 postmenopausal woman is being referred to your gynecologic oncology colleague after an office endometrial sample demonstrated a FIGO grade 1 endometrioid adenocarcinoma. The patient has no significant medical, surgical or other gynecologic history. She does not smoke and drinks only occasionally at social events. She takes a multivitamin. Her physical exam is unremarkable. Which of the following additional tests is indicated for this patient?
|
CXR.
Once a pathologic diagnosis is confirmed by biopsy, a basic clinical assessment should ensue in all patients to help define the extent of the disease. If a careful history and clinical gynecologic exam suggests that the carcinoma is likely of an early stage, minimal pre-treatment evaluation is necessary. Routine evaluation in this setting should include a chest x-ray as the lungs are the most common site of distant spread. A pelvic ultrasound is not indicated once a pathologic diagnosis has been established, although one may have been obtained as part of the initial evaluation of postmenopausal bleeding. When there is a low suspicion for advanced disease, a CT scan, MRI, PET scan, and other invasive and costly tests are not indicated. A CA-125 may be helpful in predicting those patients that may have extrauterine spread, but is not absolutely necessary. |
|
|
A 47-year-old G3P3 presents with a several month history of progressive abdominal bloating. She has had regular menses her entire life, but recently notes her bleeding to be heavier and occurring “twice a month.” She is otherwise healthy and does not smoke or drink. On examination, she is 5 feet 5 inches tall and weighs 130 pounds. Her abdominal exam is notable for some mild distension, but no palpable masses. Her pelvic examination is notable for a normal appearing cervix, a deviated, but non-enlarged uterus, and a 10 cm mobile, non-tender right adnexal mass. An office endometrial biopsy reveals complex endometrial hyperplasia without atypia. What is the most likely explanation for the adnexal mass and the findings seen on the endometrial biopsy?
|
Granulosa cell tumor
The finding of an adnexal mass in a perimenopausal woman raises the suspicion of a neoplastic process. Because of the new onset of irregular bleeding and the finding of hyperplasia, the most likely explanation would be that of a granulosa cell tumor, an estrogen-secreting tumor |
|
|
Postmenopausal bleeding or discharge accounts for the presenting symptom in 80-90% of women with endometrial cancer. Causes?
|
However, the most common causes of postmenopausal bleeding are atrophy of the endometrium (60-80%), hormone replacement therapy (15-25%), endometrial cancer (10-15%), polyps (2-12%), and hyperplasia (5-10%).
|
|
|
Risk factors for ovarian cancer?
|
The established risk factors include nulliparity, family history, early menarche and late menopause, white race, increasing age and residence in North America and Northern Europe. Smoking has not been demonstrated to be associated with an increased risk of ovarian cancer.
|
|
|
Tumor staging
|
Extent by which cancer has spread
|
|
|
TUmor grading
|
Appearance
|
|
|
A 61 year-old G3P3 is diagnosed with stage IIIA papillary serous adenocarcinoma of the ovary. She is concerned about her long-term prognosis. Which of the following factors would be most helpful in determining this patient’s prognosis?
|
TUMOR STAGE!!!!
|
|
|
A 25 year-old G1P1 comes in for her annual examination. She has intermittent left lower quadrant discomfort. She has regular menses every 30 days and uses a diaphragm for birth control. Her last menstrual period was approximately three weeks ago. Her physical examination is notable for a 3 x 5 cm left adnexal mass. Ultrasound shows a unilocular simple cyst. Which of the following is the most likely diagnosis in this patient?
|
Functional ovarian cysts are a result of normal ovulation. They may present as an asymptomatic adnexal mass or become symptomatic. Ultrasound characteristics include a unilocular simple cyst without evidence of blood, soft tissue elements or excrescences.
An endometrioma is an isolated collection of endometriosis involving an ovary. This would not classically appear as a simple cyst on ultrasound. Serous cystadenomas are generally larger than functional cysts and patients may present with increasing abdominal girth. Mucinous cystadenomas tend to be multilocular and quite large. Dermoid tumors usually have solid components or appear echogenic on ultrasound, as they may contain teeth, cartilage, bone, fat and hair. |
|
|
A 25 year-old G0 presents for a refill on her oral contraceptives. She has no significant medical or surgical history. Her grandmother was recently diagnosed with ovarian cancer and her mother is undergoing treatment for metastatic breast cancer. The patient is interested in assessing her risk for ovarian cancer susceptibility. Which of the following is the most appropriate next step in the management of this patient?
|
BRCA testing in mother.
BRCA1 and BRCA2 mutations are typically seen in cases of hereditary ovarian cancers. Overall, it has been estimated that inherited BRCA1 and BRCA2 mutations account for 5 to 10 percent of breast cancers and 10 to 15 percent of ovarian cancers among white women in the United States. Given this family history, it is highly likely that a mutation is present, and the affected individual (proband) should be tested if still alive. Because breast cancers are part of the BRCA mutation, the affected mother should be tested. Routine screening for ovarian cancer has not been established. |
|
|
A 44 year-old G0 status post tumor debulking for stage IIIB endometrioid adenocarcinoma of the ovary presents for post operative check. Her medical history is significant for diabetes, hypertension, obesity, hypercholesterolemia and major depression. Which of the following is the most appropriate next step in the management of this patient?
|
Chemo.
In all patients with advanced ovarian cancer, post-operative chemotherapy with a combination of a taxane and platinum adjunct is considered standard of care in the United States. Women who undergo surgical cytoreduction, followed by chemotherapy, have a better overall survival rate than those who undergo surgery alone. The overall response rate in women with advanced ovarian cancer following surgery and 4 to 6 cycles of combination chemotherapy with a taxane and platinum adjunct is 60-80%. The overall 5-year survival for women with Stage III and IV disease is approximately 30%. Second look laparotomy are no longer considered standard of care. |
|
|
An 18 year-old G0 presents to discuss contraception. Her best friend’s mother was just diagnosed with ovarian cancer. The patient is healthy and does not have any significant medical history. She does not have a family history of ovarian, breast or any other malignancies. She uses condoms for birth control. She would like to know what she can do to minimize her risk for developing ovarian cancer. Which of the following recommendations is the most appropriate for this patient
|
A woman’s risk for development of ovarian cancer during her lifetime is approximately 1%. Factors associated with development of ovarian cancer include low parity and delayed childbearing. Long-term suppression of ovulation appears to be protective against the development of ovarian cancer. Oral contraceptives that cause anovulation appear to provide protection against the development of ovarian cancer. Five years’ cumulative use decreases the lifetime risk by one-half.
|
|
|
The most recent consensus guidelines (2006) state that management of LSIL
|
is initial colposcopic examination (unless the woman is pregnant, postmenopausal or an adolescent).
An excisional procedure, such as cold knife biopsy or LEEP, is not warranted without a tissue diagnosis of dysplasia. |
|
|
A 34-year-old G2P2 who recently underwent colposcopy with biopsy following a Pap smear which showed low-grade squamous intraepithelial lesion, comes in to discuss her results. The biopsy results showed HSIL (CIN III). Endocervical curettage showed benign endocervical cells. What is the most appropriate next step in the management of this patient?
|
The LEEP procedure is usually done in the office under local intracervical anesthesia. It involves using an electrosurgical unit (similar to the Bovie in the operating room), along with a wire loop of varying sizes to remove the entire transformation zone and the dysplastic area(s) identified during colposcopy.
|
|
|
26-year-old G0 was found to have a low-grade squamous intraepithelial lesion (LSIL) on routine Pap smear. She underwent a colposcopy with cervical biopsy. Her colposcopy was adequate and biopsy results showed CIN-I. There was no endocervical glandular involvement. Endocervical curettage showed benign cells. Which of the following is the most appropriate treatment for this patient?
|
The patient should be followed with Pap smears at six and 12 months or undergo HPV DNA testing at 12 months. Excisional or ablative procedures are not indicated for LSIL.
Indications for cold knife conization (CKC) include: positive endocervical curettage, HSIL lesion too large for LEEP, patient not tolerant of examination in office, lesion extending into the endocervical canal beyond vision, or to rule out invasive cancer (classify the depth of invasion if biopsy shows invasion). It is unusual to manage low grade lesions by CKC. Indications for LEEP are similar to CKC. |
|
|
Tx for pain due to endometriosis?
|
A hysterectomy with bilateral salpingo-oophorectomy is the definitive treatment for a patient with pelvic pain due to endometriosis. In 60% of cases, when a patient with endometriosis undergoes a simple hysterectomy without bilateral salpingo-oophorectomy for pelvic pain, re-operation for continued pain will be necessary.
|
|
|
firm, painless, mobile mass of breast
|
fibroadenoma
|
|
|
Fibrocystic breast changes
|
are the most common type of benign breast conditions and occur most often during the reproductive years. Fibrocystic disease is often associated with cyclic mastalgia, possibly related to a pronounced hormonal response. Caffeine intake can increase the pain associated with fibrocystic breast changes, so recommending that she decrease her caffeine intake may be helpful.
|
|
|
presentation of breast cancer?
|
spontaneous bloody nipple discharge.
Even though the mass decreased in size after aspiration, the bloody discharge obtained obligates an excisional biopsy be performed to rule out breast cancer. If clear discharge is obtained on aspiration and the mass resolves, reexamination in two months is appropriate to check that the cyst has not recurred. |
|
|
manual vacuum aspiration?
|
99% effective in early pregnancy (less than 8 weeks).
|
|
|
Compared to surgical abortion, which of the following is increased in a woman undergoing a medical abortion?
|
Blood loss.
Early in pregnancy (less than 49 days) both medical and surgical procedures can be offered. Mifepristone (an antiprogestin) can be administered, followed by misoprostol (a prostaglandin) to induce uterine contractions to expel the products of conception. This approach has proven to be effective (96%) and safe. A surgical termination is required in the event of failure or excessive blood loss. Medical termination seems to be more desirable by some patients since they do not have to undergo a surgical procedure. It does not affect future fertility. Any termination of pregnancy, whether medical or surgical, can have psychological sequelae. |
|
|
Abortion
|
Abortion is legal until viability is achieved (24 weeks gestation) unless a fetal anomaly inconsistent with extrauterine life is identified. A dilation and curettage is performed if the fetus is less than 16 weeks, while dilation and evacuation can be performed after 16 weeks by those trained in the procedure. Inductions with hypertonic saline have a high morbidity, so are no longer performed.
|
|
|
The prolonged dilute Russell viper venom time leads one to suspect that the etiology of recurrent pregnancy loss is due to antiphospholipid antibody syndrome. TX?
|
The treatment is aspirin plus heparin. There is roughly a 75% success rate with combination therapy versus aspirin alone.
|
|
|
A 23 year-old G2P1 with 6 weeks amenorrhea presents with lower abdominal pain and vaginal bleeding. Her temperature is 102.0°F (38.9°C) and the cervix is 1 cm dilated. Uterus is 8-week size and tender. There are no adnexal masses. Urine pregnancy test is positive. What is the most likely diagnosis?
|
septic abortion
|
|
|
management of septic abortion?
|
broad-spectrum antibiotics and uterine evacuation
|
|
|
workup for antiphospholipid syndrome
|
ssessment of anticardiolipin antibody status, PTT, and Russell viper venom time.
|
|
|
recurrent preg losses
|
defined as >2 consecutive or >3 spontaneous losses before 20 weeks gestation
etiologies: anatomic causes, endocrine abnormalities such as hyper or hypothyroidism and luteal phase deficiency, parental chromosomal anomalies, immune factors such as lupus anticoagulant and idiopathic factors. |
|
|
A 23 year-old G1P0 at 6 weeks gestation undergoes a medical termination of pregnancy. One day later, she presents to the emergency room with bleeding and soaking more than a pad per hour for the last 5 hours. Her blood pressure on arrival is 110/60; heart rate 86. On exam, her cervix is 1 cm dilated with active bleeding. Hematocrit on arrival is 29%. Which of the following is the most appropriate next step in the management of this patient?
|
This patient is having heavy bleeding as a complication of medical termination of pregnancy. This is managed best by performing a dilation and curettage.
|
|
|
Baby size w/ T1DM
|
Small and hypoglycemic
|
|
|
Baby size w/ gestational diabetes?
|
Large and hypoglycemic
|
|
|
While in labor, a 24-year-old G1P0 woman spikes a temperature of 38.6°C and develops fetal tachycardia. Maternal labs: O+; RPR non-reactive; HBsAg, negative; HIV negative; GBS unknown. At delivery, you notice a foul smell. What will be the expected appearance of the baby?
|
Lethargic, pale with high temperature
This patient clearly has chorioamnionitis and the foul smell upon delivery is a warning sign that the infant can be septic. A septic infant will typically appear pale, lethargic and have a high temperature. |
|
|
infants of diabetic mothers at risk for?
|
hypoglycemia, polycythemia, hyperbilirubinemia, hypocalcemia and respiratory distress.
|
|
|
A flattened nasal bridge, small size and small rotated, cup-shaped ears may be associated with Down syndrome and should prompt a survey looking specifically for other features seen with Down syndrome that include: sandal gap toes, hypotonia, a protruding tongue, short broad hands, Simian creases, epicanthic folds, and oblique palpebral fissures.
|
Down syndrome
|
|
|
twin-twin transfusion syndrome
|
Polycythemia is a common complication for the plethoric twin. TTTS is a complication of monochorionic pregnancies. It is characterized by an imbalance in the blood flow through communicating vessels across a shared placenta leading to underperfusion of the donor twin which becomes anemic and overperfusion of the recipient which becomes polycythemic. The donor twin often develops IUGR and oligohydramnios, and the recipient experiences volume overload and polyhydramnios that may lead to heart failure and hydrops.
|
|
|
A 32 year-old G2P2 has just had a spontaneous vaginal delivery. She is concerned that no breast milk is yet being produced when she tries to feed her baby. You reassure her that colostrum is rich in protein and nutrients, and that her breast milk will come in 2-3 days when which of the following hormones have been cleared?
|
Estrogen and progesterone
With delivery, there is a rapid and profound decrease in the levels of progesterone and estrogen, which removes the inhibitory influence of progesterone on the production of alpha-lactalbumin by the rough endoplasmic reticulum. |
|
|
strategies to help w/ engorgement?
|
Strategies that may help include frequent nursing, taking a warm shower or warm compresses to enhance milk flow, massaging the breast and hand expressing some milk to soften the breast, wearing a good support bra and using an analgesic 20 minutes before breast feeding.
|
|
|
You tell her that more frequent suckling would be better as it will stimulate which of the following hormones?
|
While prolactin is responsible for milk production, oxytocin is responsible for milk ejection.
|
|
|
A 22 year-old G2P1 comes to your clinic today with her 3 month-old daughter. She was breastfeeding without problems until about 2 weeks ago, when she began to experience sore nipples. The nipples are very sensitive and there is a burning pain in the breasts, which is worse when feeding. The tips of the nipples are pink and shiny with peeling at the periphery. Which of the following is the underlying cause of these findings?
|
Candidiasis
|
|
|
Signs that a baby is getting sufficient milk
|
3-4 stools in 24 hours, 6 wet diapers in 24 hours, weight gain and sounds of swallowing.
|
|
|
A 30 year-old G1P1 with type 1 diabetes mellitus presents at 10 weeks gestation for a routine visit. She smokes a half a pack of cigarettes per day. Her hemoglobin A1C level is 9.7. What is the most likely structural anomaly to be detected on a second trimester fetal survey ultrasound?
|
Cardiac anomalies.
Women with poorly controlled diabetes immediately prior to conception and during organogenesis have a four- to eight-fold risk of having a fetus with a structural anomaly. The majority of lesions involve the central nervous system (neural tube defects) and the cardiovascular system. Genitourinary and limb defects have also been reported. |
|
|
Valproic acid
|
Increased risk for neural tube defects, hydrocephalus and craniofacial malformations.
|
|
|
MCC of inherited mental retardation
|
fragile x
|
|
|
Both parents are Ashkenazi Jew, what do you screen for?
|
Fanconi anemia, Tay-Sachs disease, Cystic Fibrosis, and Niemann-Pick disease
|
|
|
Both parents are black. What blood test screenings do you want to do?
|
Hgb electrophoresis, CBC - hemoglobin C trait, thalassemia, sickle cell
|
|
|
The risk of fetal loss associated with CVS
|
approximately 1%T
|
|
|
Most common genetic ABNL for Jews?
|
Tay Sachs
|
|
|
Intrauterine growth restriction is typically seen in women with pre-existing diabetes OR gestational diabetes?
|
pre-existing diabetes
|
|
|
REC DOSE OF FOLATE?
|
The recommended dose for non-high risk patients is 0.4mg/day.
The answer is D. In 1991, the Centers for Disease Control and Prevention recommended that all women with a previous pregnancy complicated by a fetal neural tube defect ingest 4 mg of folic acid daily before conception and through the first trimester. |
|
|
patient is told to report to the hospital for suspected labor if any of the following occurs
|
contractions every five minutes for one hour, rupture of membranes, fetal movement less than 10 per two hours or vaginal bleeding
|
|
|
Signs and symptoms of depression which last for less than two weeks after preg?
|
post partum blues
|
|
|
Which of the following signs or symptoms of postpartum depression are most useful to distinguish it from postpartum blues and normal changes that occur after delivery?
|
Ambivalence toward the newborn
|
|
|
Sheehan Syndrome
|
slow mental function, weight gain, fatigue, difficulty staying warm, no milk production, hypotension and amenorrhea. Treatment includes estrogen and progesterone replacement and supplementation with thyroid and adrenal hormones.
|
|
|
Among women with cardiac disease, patients with pulmonary hypertension are among the highest risk for mortality during pregnancy,
|
a 25-50% risk for death.
|
|
|
Which antidepressant is CI in preg?
|
PAXIL (paroxetine). One SSRI, Paroxetine (Paxil) has recently been changed to a category D drug because of the increased risk of fetal cardiac malformations and persistent pulmonary hypertension.
|
|
|
Renal infection is the most common serious medical complication of pregnancy.
|
Initially aggressive intravenous hydration is given to ensure adequate urinary output. Antimicrobials are begun promptly after diagnosis. The majority of patients are afebrile by 72 hours. If there is no clinical improvement by 72 hours, further evaluation is warranted including sonography to look for urinary tract obstruction (abnormal ureteral or pyelocaliceal dilatation) or calculi. Obstruction can be relieved by cystoscopic placement of a double-J ureteral stent unless long-term stenting is foreseen, then percutaneous nephrostomy is indicated. Surgical exploration is required in up to 2% of women if other conservative therapies are not successful.
|
|
|
Vulvar vestibulitis syndrome
|
constellation of symptoms and findings limited to the vulvar vestibule, which include severe pain on vestibular touch or attempted vaginal entry, tenderness to pressure and erythema of various degrees. Symptoms often have an abrupt onset and are described as a sharp, burning and rawness sensation. Women may experience pain with tampon insertion, biking or wearing tight pants, and avoid intercourse because of marked introital dyspareunia.
|
|
|
extreme vulvar pruritus and may also present with vulvar burning, pain and introital dyspareunia. Early skin changes include polygonal ivory papules involving the vulva and perianal areas, waxy sheen on the labia minora and clitoris, and hypopigmentation. The vagina is not involved. More advanced skin changes may include fissures and erosions due to a chronic itch-scratch-itch cycle, mucosal edema and surface vascular changes and, ultimately, scarring with loss of normal architecture, such as introital stenosis, and resorption of the clitoris (phimosis) and labia minora.
|
Lichen sclerosus
tx: steroids |
|
|
A common vulvar non-neoplastic disorder, results from chronic scratching and rubbing, which damages the skin and leads to loss of its protective barrier. Over time, a perpetual itch-scratch-itch cycle develops, and the result is susceptibility to infection, ease of irritation and more itching. Symptoms consist of severe vulvar pruritus, which can be worse at night. Clinical findings include thick, lichenified, enlarged and rugose labia, with or without edema. The skin changes can be localized or generalized
|
Lichen simplex chronicus
|
|
|
The majority of genuine stress incontinence is due to
|
urethral hypermobility (straining Q-tip angle >30 degrees from horizon
|
|
|
A 90-year-old G7P7 woman presents with severe vaginal prolapse. The entire apex, anterior and posterior wall are prolapsed beyond the introitus. She cannot urinate without reduction of the prolapse. Hydronephrosis was noted on ultrasound of the kidneys and it is thought to be related to the prolapse. She has a long-standing history of diabetes and cardiac disease. She is not a candidate for general or regional anesthesia. She has failed a trial of pessaries. Which of the following is the next best step in the management of this patient?
|
Colpocleisis - tx vaginal prolapse
|
|
|
Tubal ligation has not been shown to reduce the risk of
|
ovarian cancer - mech unknown
|
|
|
Contraindications to estrogen only pills
|
include a history of thromboembolic disease, women who are lactating, women over age 35 who smoke or women who develop severe nausea with combined oral contraceptive pills
|
|
|
Progestins should be used with caution with?
|
depression
|
|
|
Management of an endometrial polyp?
|
observation, medical management with progestin, curettage, surgical removal (polypectomy) via hysteroscopy, and hysterectomy. Observation is not recommended if the polyp is > 1.5 cm
|
|
|
postmenopausal. In addition to weight bearing exercise and vitamin D supplementation, what optimal daily calcium intake should she take?
|
postmenopausal women require a total of 1200 mg of elemental calcium per day.
|
|
|
effects of hormone therapy on serum lipid profiles?
|
DEC LDL cholesterol and the increase in HDL cholesterol.
|
|
|
How do oral contraceptives relieve primary dysmenorrhea?
|
The progestin in oral contraceptives creates endometrial atrophy. Since prostaglandins are produced in the endometrium, there would be less produced. Dysmenorrhea should be improved
|
|
|
Blue-black powder burn lesions are seen in the pelvis. A biopsy is performed and sent to pathology. Which of the following pathologic lesions would you expect to see in this patient?
|
The lesions described are classic for endometriosis. One would therefore expect to see endometrial glands/stroma with hemosiderin-laden macrophages.
|
|
|
exercise-induced hypothalamic amenorrhea
|
normal FSH and low estrogen levels
|
|
|
A clomiphene challenge test
|
giving clomiphene citrate days five to nine of the menstrual cycle and checking FSH levels on day three and day 10, will help determine ovarian reserve
|
|
|
Vit Def in which lead to PMS?
|
Vitamin deficiency of A, E and B6 have been associated with an increase in PMS. Replacement of these vitamins might improve PMS symptoms and avoid further medical therapy.
|
|
|
Risk factors for PMS
|
include a family history of premenstrual syndrome (PMS) and Vitamin B6, calcium, or magnesium deficiency
|
|
|
36 yo post partum (3 months ago). In the last month, she has noticed a large amount of hair on her brush each morning. Her father has male pattern baldness and her mother, who is postmenopausal, has had some thinning of her hair, as well. Testosterone and TSH levels are within the normal range. Which of the following is the most likely underlying cause for alopecia in this patient?
|
High estrogen levels during pregnancy.
High estrogen levels in pregnancy increase the synchrony of hair growth. Therefore, hair grows in the same phase and is shed at the same time. |
|
|
Rapid onset of hirsutism and virilizing signs are hallmarks of this disease, and include many of the findings in this patient including acne, hirsutism, amenorrhea, clitoral hypertrophy, and deepening of the voice.
|
The most likely diagnosis in this patient is a testosterone-secreting ovarian tumor. Sertoli-Leydig cell tumors are commonly diagnosed in women between the ages of 20-40, and are most often unilateral.
Abnormal laboratory findings include suppression of FSH and LH, marked elevation of testosterone, and presence of an ovarian mass |
|
|
hyperthecosis
|
more severe form of polycystic ovarian syndrome (PCOS). It is associated with virilization due to the high androstenedione production and testosterone levels. In addition to temporal balding, other signs of virilization include clitoral enlargement and deepening of the voice. Hyperthecosis is more difficult to treat with oral contraceptive therapy. It is also more challenging to achieve successful ovulation induction.
|
|
|
A 24-year-old G1P1 presents with a complaint of decreasing breast size and hirsutism noted the last three months. She also notes her skin feels oily and her husband has mentioned her voice seems to be getting deeper. She has no medical or surgical problems and takes no medications. Physical examination reveals oily skin, upper lip and chin terminal hair, and normal appearing breasts. Pelvic examination reveals her clitoris to be 2 cm in length and 1 cm wide. Which of the following is the most likely cause of her symptom constellation?
|
The likely cause of this patient’s sudden onset of symptom is an increase in androgens due to a tumor. Hirsutism is often the result of a benign condition, however, may be a sign of significant disease if sudden in onset and coupled with virilization. Virilization in the female may be manifested by frontal hair thinning, oily skin or acne, deepening of the voice, clitoral enlargement, menstrual irregularities, and increased muscle strength
|
|
|
Noonan’s syndrome
|
short stature, webbed neck, heart defects, abnormal faces and delayed puberty. Individuals with Noonan’s syndrome have a normal karyotype.
|
|
|
True precocious puberty is manifested by premature secretion of GnRH hormone in a pulsatile manner. Tx?
|
GnRH agonist to suppress pituitary production of follicular-stimulating hormone and luteinizing hormone.
|
|
|
A 17-year-old is brought to the physician because she has never had a menstrual cycle. She has normal breast and pubic hair development. Physical examination reveals a small vaginal opening with a blind pouch. Pelvic ultrasound reveals normal ovaries, but absence of uterus and cervix. Which of the following is the most appropriate next study in this patient?
|
Renal US. Renal anomalies occur in 25-35% of females with Mullerian agenesis. The uterus and cervix are absent, but the ovaries function normally and, therefore, secondary sexual characteristics are present. You would expect the karyotype in this patient to be 46,XX and testosterone levels in the female range.
|
|
|
postterm pregnancies associated w/?
|
placental sulfatase def, fetal adrenal hyperplasia, anencephaly, inaccurate/unkonwn dates, extrauterine preg, macrosomia, oligohydramnios, meconium aspiration, uteroplacental insufficiency, dysmaturtiy
|
|
|
benefits of amnioinfusion (normal saline infused into the intrauterine cavity)
|
dec repetitive variable decelrations
|
|
|
optimal management for pt w/ favorable cervix at greater than or equal to 41 weeks?
|
DELIVERY.
|
|
|
management for pt w/ unfavorable cervix at 42 weeks?
|
2x weekly NSTs w/ AFI.
|
|
|
infants w/ dysmaturity?
|
withered, meconium stained, long nailed, fragile and small placenta. Infants at risk for stillbirth
|
|
|
cervical ripening agents?
|
prostaglandin E1
|
|
|
endomyometritis tx?
|
ampicillin and gentamicin (gram negative)
|
|
|
exagerrated response to lymphatic and venous congestion associated w/ lactation. Milk letdown occurs on PPD #2 or 3. IF baby not feeding well, breast can becoem engorged and can cause low grade fever
|
breast engorgement
|
|
|
septic thrombophlebitis (thrombosis of venous system of pelvis) tx?
|
heparin. addition of anticoagulants to abx and resolution of fevers is fast.
|
|
|
reactive NST
|
TWO accels of 15 BPM for 15 seconds within 20 mins
|
|
|
contraction stress test
|
assesses uteroplacental insufficiency and looks for persistent late decels after contractions (3/10 minutes)
|
|
|
prolonged periods of fetal tachy due to?
|
maternal fever or chorioamnionitis
|
|
|
variable decels
|
umbilical cord compression
|
|
|
tx fetal hypoperfusion
|
change in maternal posn to left lateral posn, maternal supplemental O2, tx of maternal hypotension, d/c oxytocin, intrauterin resuscitation w/ tocolytics and IV fluids, fetal acid/base assessment w/ fetal scalp capillray blood gas or pH measurement
|
|
|
what uterotonic (Methergine, prostaglandins and oxytocin) agent should you AVOID in pts w/ chronic HTN and pre-eclamp?
uterotonic = inc contracttions |
Methylergonovine is an ergot alkaloid, which is a potent smooth muscle constrictor. It is also a vasoconstrictive agent and should be withheld from women with hypertension and/or preeclampsia.
|
|
|
what is assoc w/ retained placenta?
|
prior Cesarean delivery, uterine leiomyomas, prior uterine curettage and succenturiate lobe of placenta.
|
|
|
Postpartum hemorrhage is defined
|
bleeding in excess of 500 cc after a vaginal delivery or in excess of 1000 cc after a Cesarean delivery
|
|
|
RF for Uterine atony
|
precipitous labor, multiparity, general anesthesia, oxytocin use in labor, prolonged labor, macrosomia, hydramnios, twins and chorioamnionitis.
|
|
|
A 30 year-old G5P4 at 24 weeks gestation is found to have an anterior placenta previa. She has a history of three prior Cesarean deliveries. What is the most likely serious complication that can lead to obstetric hemorrhage in this woman?
|
Placenta accreta. in the presence of a low-lying anterior placenta in a patient with a history of multiple Cesarean births, the diagnosis of the placenta accreta must be entertained.Placenta accreta is an abnormally firm attachment of the placenta to the uterine wall.
|
|
|
A 37 year-old G4P3 presents in labor at term. Her medical history and prenatal course are uncomplicated. She delivers a 3500 gram infant spontaneously after oxytocin augmentation of labor. Immediately postpartum, there is excessive bleeding greater than 2000 cc. She has an IV in place. There are no lacerations and the uterus is found to be boggy. Which of the following is the most appropriate next step in the non-operative management of this patient?
|
Intramuscular prostaglandin F2.
Neither prostaglandin F2-alpha (BRONCHOCONSTRICTION) nor methylergonovine (STROKE) should ever be administered IV, as they can lead to severe bronchoconstriction and stroke, respectively. |
|
|
A 23 year-old G1P0 presents in labor at term. Her prenatal course was uncomplicated. She delivers a 3500 gram infant spontaneously after oxytocin augmentation of labor. Immediately postpartum, there is excessive bleeding greater than 2000 cc. There are no lacerations and the uterus is found to be boggy. Her blood pressure is 70/30; pulse 144; and hematocrit is 20%. Conservative and medical management have failed and you proceed with an exploratory laparotomy. Which of the following is the most appropriate next step in the management of this patient?
|
Hypogastric artery ligation
|
|
|
management of postpartum hemorrhage
|
make sure the uterus is well-contracted, there is no retained placental tissue and to look for lacerations.
|
|
|
factors for uterine inversion (ones that lead to over distended uterus)
|
excessive (iatrogenic) traction on the umbilical cord during the 3rd stage of delivery, Grand multiparity, multiple gestation, polyhydramnios and macrosomia
|
|
|
Recs for weight gain in preg?
|
underweight (BMI < 18.5 kg/m2) total weight gain 28 – 40 pounds,
normal weight (BMI 18.5 – 24.9 kg/m2) total weight gain 25 – 35 pounds, overweight (BMI 25 – 29.9 kg/m2) total weight gain 15 - 25 pounds obese (BMI > 30 kg/m2) total weight gain 11 - 20 pounds. |
|
|
A 24 year-old G1P0 at 30 weeks gestation reports difficulty breathing, cough and frothy sputum. She was admitted for preterm labor 24 hours ago. She is a non-smoker. She has received 6 liters of lactated Ringers solution since admission. Urine output has not been calculated. She is receiving terbutaline. Pertinent physical exam findings: temperature 100.2°F (37.9°C), respiratory rate 24, heart rate 110, blood pressure 132/85, pulse oximetry on 100% non-rebreather mask 97%. She appears in distress. Lungs reveal bibasilar crackles. Uterine contractions are regular every 3 minutes. Uterus is tender to palpation between contractions. The fetal heart rate is 140 beats/minute. Labs: White blood cell count 17,500/mL with 94% segmented neutrophils. Potassium and sodium are normal. What is the most likely cause of this patient’s symptoms?
|
Tocolysis with terbutaline or other beta agonists increase the susceptibility to pulmonary edema, especially with the use of isotonic fluids.
|
|
|
17 year-old G1P0 at 32 weeks gestation complains of right flank pain that is “colicky” in nature and has been present for two weeks. She denies fever, dysuria and hematuria. Physical examination is notable for moderate right costovertebral angle tenderness. Pertinent labs: white blood cell count 8,800/mL, urine analysis negative for infection and blood. A renal ultrasound reveals no signs of urinary calculi, but there is moderate (15 mm) right hydronephrosis. Which of the following is likely cause of these findings?
|
Compression by the uterus and right ovarian vein
|
|
|
Which of the following is the correct statement regarding cardiovascular adaptation in pregnancy?
|
The cardiac output increases up to 33% due to increases in both the heart rate and stroke volume. The SVR falls during pregnancy. Up to 95% of women will have a systolic murmur due to the increased volume.
The systemic vascular resistance (SVR) is normally greater than the pulmonary vascular resistance |
|
|
Relative hemodilution of pregnancy
|
NORMOCYTIC anemia
|
|
|
Pulm changes in preg?
|
The respiratory rate does not change during pregnancy, but the TV is increased which increases the minute ventilation, which is responsible for the respiratory alkalosis.
|
|
|
signs of ruptured ectopic?
|
signs of hypovolemia (tachycardia, hypotension) with peritoneal signs (rebound, guarding and severe abdominal tenderness) and a positive pregnancy test lead to the diagnosis of ruptured ectopic pregnancy
NEXT STEP? Laparoscopy |
|
|
Certain conditions must be met prior to initiating methotrexate therapy for treatment of an ectopic pregnancy.
|
hemodynamic stability, nonruptured ectopic pregnancy, size of ectopic mass <4 cm without a fetal heart rate or <3.5 cm in the presence of a fetal heart rate, normal liver enzymes and renal function, normal white cell count, and the ability of the patient to follow up rapidly (reliable transportation, etc.), if her condition changes
|
|
|
diagnosis of ectopic pregnancy
|
1) a fetal pole is visualized outside the uterus on ultrasound; 2) the patient has a Beta-hCG level over the discriminatory zone (the level at which an intrauterine pregnancy should be seen on ultrasound, usually 2000 mIU/ml) and there is no intrauterine pregnancy (IUP) seen on ultrasound; or 3) the patient has inappropriately rising Beta-hCG level (less than 50% increase in 48 hours) and has levels which do not fall following diagnostic dilation and curettage.
|
|
|
A 26 year-old G2P0 presents for counseling following manual vacuum aspiration of an 8-week missed abortion. The patient asks whether an uncomplicated first trimester pregnancy termination three years ago might have predisposed her to the subsequent spontaneous abortion. What are the patient’s risks associated with the prior surgical abortion in the first trimester?
|
Does not predispose the patient to subsequent spontaneous abortion
|
|
|
A 22 year-old G1P0 presents to the emergency department at eight weeks gestation experiencing heavy vaginal bleeding. Pelvic examination demonstrates brisk bleeding through a dilated cervical os. The patient’s hemoglobin is 7 g/dL (hematocrit 21%.) Which of the following is the most appropriate next step in the management of this patient?
|
Dilatation and suction curettage. This patient is actively bleeding and is anemic. Although clinicians increasingly utilize both expectant management and various drug regimens to treat spontaneous abortion, a prerequisite for either is that the patient is hemodynamically stable and reliable for follow-up care.
|
|
|
Placement of a cervical cerclage at approximately 14 week’s gestation
|
Pregnancy loss in the late second trimester is not usually related to genetic abnormality of the conceptus and most clinicians delay placement of a cerclage until after the first trimester, given the high background prevalence of first trimester pregnancy wastage
|
|
|
A 35 year-old presents to the emergency department with heavy vaginal bleeding at 7 weeks gestation. On examination, she has a dilated cervix with blood and tissue present at the cervical os. Which of the following is the most likely chromosomal abnormality to be found in the karyotypic evaluation of the products of conception?
|
Autosomal trisomy.
Autosomal trisomy is the most common abnormal karyotype encountered in spontaneous abortuses, accounting for approximately 40-50% of cases. Triploidy accounts for approximately 15%, tetraploidy 5% of cases, and Monosomy X (45X, 0) identified in 15-25% of losses. |
|
|
A 27 year-old G2P0 is diagnosed with an early first trimester spontaneous abortion. She has a history of Type I Diabetes Mellitus, mild chronic hypertension and one prior termination of pregnancy. Which of the following is the most likely cause of this spontaneous abortion?
|
Diabetes mellitus
Systemic diseases such as diabetes mellitus, chronic renal disease and lupus are associated with early pregnancy loss. In women with insulin-dependent diabetes, the rates of spontaneous abortion and major congenital malformations are both increased. |
|
|
Which of the following non-invasive test can detect severe fetal anemia?
|
Middle Cerebral Artery peak systolic velocity.
Noninvasive diagnosis of fetal anemia has been performed with Doppler ultrasonography. The use of middle cerebral artery peak systolic velocity in the management of fetuses at risk for anemia because of red cell alloimmunization has emerged as the best test for the noninvasive diagnosis of fetal anemia. |
|
|
A 24-year-old G1P0 woman presents at 32-weeks gestation with vaginal bleeding, most likely caused by placental abruption. You want to give the patient an appropriate RhoGAM dose and determine the presence and degree of fetal-maternal hemorrhage. How can you accurately and immediately estimate the degree of fetal-maternal hemorrhage?
|
Kleihauer-Betke test.
The Kleihauer-Betke test is an accurate and sensitive acid elution test. It has great value in determining the incidence and size of fetal transplacental hemorrhage. In this test, using acid elution, the mother’s red blood cells become very pale, while fetal cells, which contain a different form of hemoglobin, remain stained. Simple comparative counts allow an estimate of whether a significant feto-maternal transfusion has occurred. |
|
|
A 28-year-old G2P1 woman presents at 20 weeks gestation transferred from her general practitioner. As an obstetrician-gynecologist, you are asked to evaluate and care for this patient who has an anti-D titer of 1:64. This pregnancy has been complicated by scant vaginal bleeding at 7 weeks and an abnormal maternal serum alpha fetoprotein (MSAFP), with increased risk for Down syndrome, but had a normal amniocentesis: 46, XX. Her previous obstetric history is significant for a Cesarean section at 34-weeks due to placental abruption and fetal distress. Prenatal labs at 6 weeks: Rh-negative. Antibody screen positive: anti-D 1:64. Which is the most likely source of the Rh sensitization?
|
Placental abruption.
This patient was sensitized during her first pregnancy that was complicated by abruption and required Cesarean delivery. Transplacental hemorrhage of fetal Rh-positive red blood cells into the circulation of the Rh-negative mother may occur following a number of obstetric procedures and complications, such as amniocentesis, chorionic villus sampling, spontaneous/threatened abortion, ectopic pregnancy, dilation and evacuation, placental abruption, antepartum hemorrhage, preeclampsia, cesarean section, manual removal of the placenta and external version. |
|
|
A 24-year-old G2P1 woman has a fetus that is affected by Rh disease. At 30 weeks gestation, the delta OD450 (optical density deviation at 450 nm) results plot on the Liley curve in Zone 3. Which of the following is the most appropriate next step in the management of this patient?
|
Values in Zone 3 of the Liley curve indicate the presence of severe hemolytic disease, with hydrops and fetal death likely within 7-10 days, thus demand immediate delivery or fetal transfusion. At 30 weeks gestation, the fetus would benefit from more time in utero. Thus, an attempt should be made to correct the underlying anemia. Intravascular transfusion into the umbilical vein is the preferred method.
|
|
|
A 24-year-old G2P1 woman has a fetus that is affected by Rh disease. At 28 weeks gestation, an amniocentesis was performed. The amniotic fluid sample was sent for a delta OD450 (optical density deviation at 450 nm) measurement. What does this value represent in the amniotic fluid?
|
Bilirubin.
In the presence of a severely erythroblastotic fetus, the amniotic fluid is stained yellow. The yellow pigment is bilirubin, which can be quantified most accurately by spectrophotometric measurements of the optical density between 420 and 460nm, the wavelength absorbed by bilirubin. The deviation from linearity of the optical density reading at 450nm is due to the presence of heme pigment, an indicator of severe hemolysis. |
|
|
A 24-year-old G2P1 Rh-negative female patient is found at 10 weeks gestation to have anti-D antibodies. You follow her closely during this pregnancy and order serial ultrasound examinations. Which of the following fetal ultrasound findings would be most explained by the presence of Rh disease?
|
Pericardial effusion.
Fetal hydrops is easily diagnosed on ultrasound. It develops in the presence of decreased hepatic protein production. It is defined as a collection of fluid in two or more body cavities, such as ascites, pericardial and/or pleural fluid and scalp edema. On occasion, when extramedullary hematopoiesis is extensive, there will be evidence of hepatosplenomegaly. Placentomegaly (placental edema) and polyhydramnios are also seen on ultrasound. |
|
|
A 24-year-old G1P1 Rh-negative woman has just delivered a healthy term infant who is Rh-positive. She is concerned about her risk for Rh sensitization. What is the most likely volume of feto-maternal hemorrhage that occurred during this pregnancy?
|
<0.1 cc.
While 75% of all gravidas have evidence of transplacental hemorrhage during pregnancy or immediately after delivery, 60% of these patients have <0.1 cc of fetal blood in the maternal circulation |
|
|
when to administer Rhogam?
|
The current recommendations for Rh-negative women without evidence of Rh immunization is one prophylactic dose of RhoGAM intramuscularly within 72 hours of delivering an Rh-positive baby, following spontaneous or induced abortion, following antepartum hemorrhage, following amniocentesis or chorionic villus sampling, and prophylactically at 28-weeks gestation (after an indirect Coombs’ test)
|
|
|
A 24-year-old G1P0 woman presents at 32 weeks gestational age with vaginal bleeding most likely caused by placental abruption. She receives a standard dose of 300 micrograms of RhoGAM. What amount of fetal blood is neutralized by this dose?
|
30 cc of fetal blood is neutralized by the 300ug dose of RhoGAM
|
|
|
A 33-year-old G2P1 woman at 29 weeks gestation presents with confirmed preterm rupture of membranes. She denies labor. She takes prenatal vitamins and iron. She denies substance abuse, smoking or alcohol use. Her prior pregnancy was delivered vaginally at 41 weeks after spontaneous rupture of membranes. Her blood pressure is 110/70; pulse 84; temperature 99°F. Which of the following will prolong the latency period by approximately 7 days?
|
Antibiotic therapy given to patients with preterm premature rupture of the membranes has been found to prolong the latency by up to 5-7 days, as well as reduce the incidence of maternal amnionitis and neonatal sepsis
|
|
|
The primary risk factor for preterm rupture of membranes
|
genital tract infection, especially associated with bacterial vaginosis.
|
|
|
A 19-year-old G2P1 woman at 30 weeks gestation presents with preterm rupture of membranes, 6 hours ago. She denies labor. She takes prenatal vitamins and iron. She denies substance abuse, smoking or alcohol use. Her prior pregnancy was delivered vaginally at 41 weeks after spontaneous rupture of membranes. Her blood pressure is 110/70; pulse 84; temperature 98°F. Pertinent sonographic findings reveal a cervical length of 34mm and an amniotic fluid index of 3. What is the likelihood she will deliver within a week?
|
80%
The time from premature rupture of membranes to labor is inversely related to gestational age. While at term, 90% will go into labor within 24 hours of PROM, in those pregnancies at 28 weeks to 34 weeks; 50% labor within 24 hours and 80% within 48 hours. |
|
|
SE of terbutaline?
|
Terbutaline is a beta-adrenergic agent. Side effects include tachycardia, hypotension, anxiety and chest tightening or pain
|
|
|
A 26-year-old G2P1 woman presents in preterm labor at 33 weeks gestation. She has a history of a prior preterm birth at 32-weeks gestation. She has insulin dependent diabetes and has a history of myasthenia gravis. She has regular contractions every 3 minutes and fetal heart tones are reassuring. Cervix is 3cm dilated and 0 station. Her blood pressure is 140/90, which of the following is the most appropriate tocolytic to use in this patient?
|
Calcium channel blocker.
Terbutaline and ritodrine are contraindicated in diabetic patients, magnesium sulfate is contraindicated in myasthenia gravis, and indomethacin is contraindicated at 33 weeks due to risk of premature ductus arteriosus closure. |
|
|
What is a possible fetal effect associated with Betamethasone therapy?
|
Treatment with Betamethasone from 24 to 34-weeks gestation has been shown to increase pulmonary maturity and reduce the incidence and severity of RDS (respiratory distress syndrome) in the newborn. It is also associated with decreased intracerebral hemorrhage and necrotizing enterocolitis in the newborn
|
|
|
MOA of Mg sulfate?
|
Competes with calcium for entry into cells
|
|
|
Smoking increases the risk of several serious complications of pregnancy
|
including placental abruption, placental previa, fetal growth restriction, preeclampsia and infection
|
|
|
Which of the following is associated with breech presentation?
|
Prematurity, multiple pregnancy, genetic disorders, polyhydramnios, hydrocephaly, anencephaly, placenta previa, uterine anomalies and uterine fibroids
|
|
|
A 34-year-old G2P1 woman at 40 weeks gestation, with a history of one prior vaginal delivery, strongly desires an induction of labor, as she is unable to sleep secondary to severe back pain. Her cervical exam is closed, 20% effaced and -2 station. The cervix is firm and posterior. Which of the following is the most appropriate next step in the management of this patient?
|
Cytotec (misoprostol)
The patient is multiparous at term and waiting until she reaches 42 weeks may increase the risk of perinatal mortality. Since she is uncomfortable with back pain, she may be undergo labor induction. Her cervix is unfavorable; therefore, cytotec administration is appropriate prior to pitocin induction. |
|
|
A 20-year-old G1 woman at 40-weeks gestation presents to Labor and Delivery at 10:00 am, complaining of painful contractions every 3 to 4 minutes since midnight. Her exam on admission was 2 centimeters dilated, 90% effaced and 0 station. Three hours later, her exam is unchanged. The patient is still having contractions every 3 to 4 minutes. She is discouraged about her lack of progress. Which of the following is the most appropriate next step in the management of this patient?
|
Counseling about latent phase of labor and rest.
The patient is in the latent phase of labor and has not yet reached the active phase (more than 4 cm). A prolonged latent phase is defined as >20 hours for nulliparas and >14 hours for multiparas, and may be treated with rest or augmentation of labor. It is premature to proceed with a C-section. |
|
|
At what gestational age would the fetus be most susceptible to developing mental retardation with sufficient doses of radiation?
|
The risk of developing microcephaly and severe mental retardation is greatest between eight and 15 weeks gestation
|
|
|
A 39-year-old G4P1 at 36 weeks gestation presents to labor and delivery. Upon initial evaluation, no fetal heart tones were noted on Doptone. Ultrasound confirms a stillbirth. Problems during the pregnancy include diagnosis of an open neural tube defect, estimated fetal weight >90th percentile, polyhydramnios and a nonreactive NST (non-stress test) the week prior to admission. What is the most likely etiology of this stillbirth?
|
Diabetes
Uncontrolled diabetes during organogenesis is associated with a high rate of birth defects. The most common sites affected are the spine and the heart of the fetus, although all birth defects are increased. Fetuses in utero exposed to high levels of glucose transplacentally have increased growth and polyuria resulting in an increase in the amniotic fluid. |
|
|
A 26-year-old G1 with last menstrual period 10 weeks ago presents to your office for her first prenatal visit. She reports vaginal spotting for the last two days. You perform an ultrasound that shows an intrauterine pregnancy consistent with nine weeks gestation with no cardiac activity. She denies cramping or abdominal pain. What is the most important laboratory test to check for this patient?
|
Maternal blood type
A maternal blood type should be checked on all women with vaginal bleeding during pregnancy, unless it was documented earlier in the pregnancy. If the patient’s blood type is Rh-negative, RhoGAM would be indicated to prevent Rh sensitization. |
|
|
A 33-year-old G2P1 with a known twin gestation presents to your office at 23 weeks gestation and notes that two days prior she had a nosebleed. She has not been seen in your office for the last seven weeks. Ultrasound today shows a demise of one twin that has measurements consistent with 21 weeks gestation. What is the next step in the management of this patient?
|
Maternal fibrinogen level.
When a dead fetus has been in utero for three to four weeks, fibrinogen levels may decrease, leading to a coagulopathy. The patient’s nosebleed may be a common pregnancy finding or be related to the demise, and a coagulopathy must be ruled out. Induction should be considered, but may be delayed after the death of a twin in order to allow the viable twin to mature. In these cases, fibrinogen levels should be monitored to detect a progressive coagulopathy. Usually this is performed weekly or biweekly, depending on the levels obtained. |
|
|
A 29-year-old G4P2 woman was diagnosed with twin-twin transfusion syndrome when an ultrasound was performed at 24 weeks gestational age. Which of the following is a complication of twin-twin transfusion syndrome?
|
Neuro sequelae in survivors.
Untreated severe twin-twin transfusion syndrome has a poor prognosis, with perinatal mortality rates of 70-100%. Death in utero of either twin is common. Surviving infants have increased rates of neurological morbidity, with increased risk of cerebral palsy for the surviving twin. The donor twin becomes anemic and hypovolemic, and growth is retarded. The recipient twin becomes plethoric, hypervolemic and macrosomic. |
|
|
Ultrasound markers suggestive of dizygotic (non-identical) twins
|
dividing membrane thickness greater than 2 mm, twin peak (lambda) sign, different fetal genders and two separate placentas (anterior and posterior)
|
|
|
causes of oligohydramnios
|
renal agenesis, polycystic kidney dz, obstruction of genitourinary system.
dx: AFI < 5 causes: dec placental perfusion, dec fluid production by fetus, rupture of membranes |
|
|
polyhydramnios
|
AFI > 20-25, assoc w/ congenital anomalies, diabetes, multiple gestations, hydrops
management: careful verification of presentation and close observation for cord prolapse |
|
|
danazol
|
suppresses midcylce LH/FSH surge
|
|
|
GNRH agonist
|
suppress HPA
|
|
|
sinusoidal pattern
|
regular,smooth, undulating form typical of a sine wave that occurs with a frequency of two to five cycles/
minute and an amplitude range of five to 15 beats/minute. It is also characterized by a stable baseline heart rate of 120 to 160 beats/minute and absent beat-to-beat variability. |
|
|
Uterine hyperstimulation on fetal heart recordings?
|
prolonged bradycardia
|
|
|
methergine and prostaglandin ADMINISTRATION?
|
Neither prostaglandin F2-alpha nor methylergonovine should ever be administered IV, as they can lead to severe bronchoconstriction and stroke, respectively. Oxytocin is administered as a short time, rapid infusion of a dilute solution (20-80 units in a liter) and not as an IV push
|
|
|
G1P0 at 16 weeks gestation was admitted 4 days ago because of back pain, chills and fever. She has been receiving aggressive hydration and taking broad-spectrum antibiotics but continues to have spiking fever up to 102.0°F (38.9°C). Work-up reveals a right ureteral obstruction secondary to calculi. Which of the following is the most appropriate next step in the management of this patient?
|
Pass a double-J ureteral stent.
Initially aggressive intravenous hydration is given to ensure adequate urinary output. Antimicrobials are begun promptly after diagnosis. The majority of patients are afebrile by 72 hours. If there is no clinical improvement by 72 hours, further evaluation is warranted including sonography to look for urinary tract obstruction (abnormal ureteral or pyelocaliceal dilatation) or calculi. Obstruction can be relieved by cystoscopic placement of a double-J ureteral stent unless long-term stenting is foreseen, then percutaneous nephrostomy is indicated. |
|
|
A 39-year-old G1 presents in labor at term. The estimated fetal weight is 3200 g. She is 10 cm dilated with left sacrum anterior at +2 station. Which of the following is the most appropriate next step in the management of this patient?
|
Recommend a Cesarean section.
Most recent data suggests that breech infants delivered vaginally are at higher risk for neonatal complications. Therefore, it would be recommended that this patient undergo a Cesarean section, especially since this is her first pregnancy. External cephalic version is contraindicated in active labor!!!! |
|
|
pregnant pt come to hospital if:
|
contractions every five minutes for one hour, rupture of membranes, fetal movement less than 10 per two hours or vaginal bleeding
|
|
|
A 36 year-old G2P0 at 11 weeks gestational age requests a surgical termination of pregnancy. She had a manual vacuum aspiration last year and would like to undergo the same procedure again. She has chronic hypertension and diabetes well controlled on medications. Vital signs reveal a blood pressure of 120/80 and fasting blood glucose of 100. Which of the following is a contraindication for manual vacuum aspiration of this patient?
|
gestational age.
Manual vacuum aspiration is more than 99% effective in early pregnancy (less than 8 weeks). |
|
|
Which of the following has the strongest association with premenstrual syndrome?
|
Positive family history
|
|
|
Acanthosis nigricans associated w/?
|
elevated androgen levels and hyperinsulinemia
|
|
|
A 24 year-old G0 presents with a one-year history of introital and deep thrust dyspareunia. She also has a 2-year history of severe dysmenorrhea, despite the use of oral contraceptives. She underwent a diagnostic laparoscopy 6 months ago that showed minimal endometriosis with small implants in the posterior cul de sac only, which were ablated with a CO2 laser. On further questioning, she reports significant urinary frequency, urgency and nocturia. A recent urine culture was negative. What is the most likely diagnosis in this patient?
|
interstitial cystitis.
Interstitial cystitis (IC) is a chronic inflammatory condition of the bladder, which is clinically characterized by recurrent irritative voiding symptoms of urgency and frequency, in the absence of objective evidence of another disease that could cause the symptoms. Pelvic pain is reported by up to 70% of women with IC and, occasionally, it is the presenting symptom or chief complaint. Women may also experience dyspareunia. The specific etiology is unknown, but IC may have an autoimmune and even hereditary component. |
|
|
abortion < 16 weeks
|
D&C
|
|
|
abortion > 16 weeks
|
dilation and evacuation
|
|
|
chlamydia and gonorrhea screening
|
The U.S. Preventive Services Task Force recommends chlamydia and gonorrhea screening for all sexually active patients, age 25 and younger
|
|
|
Central and lateral cystoceles are repaired
|
fixing defects in the pubocervical fascia or reattaching it to the sidewall, if separated from the white line
|
|
|
rectocele repair
|
Defects in the rectovaginal fascia are repaired
|
|
|
Enteroceles are repaired by
|
either vaginal or abdominal enterocele repairs.
|
|
|
Vaginal vault prolapse tx
|
supporting the vaginal cuff to the uterosacral ligaments, sacrospinous ligament or sacrocolpopexy
|
|
|
how to tx breast cancer during preg?
|
Surgical treatment may be definitive for breast carcinoma during pregnancy and in the absence of metastatic disease a wide excisional biopsy, modified radical mastectomy, or total mastectomy with axillary node staging can be performed. Non-pregnant women receive adjunctive radiotherapy with breast-conserving surgery. However, this is not recommended during pregnancy due to sizeable abdominal scatter placing the fetus at significant risk for excessive radiation.
|
|
|
A 39 year-old G5P4 is referred to you at 36 weeks for polyhydramnios. The estimated fetal weight is 1900 g, fetal measurements are symmetric and the amniotic fluid index is 28. Her prenatal course was uneventful; however, she declined genetic testing. She is not in labor, nor does she report any respiratory difficulty. Which of the following would yield the most information to plan the delivery?
|
Fetal karyotype.
Symmetric fetal growth restriction in the presence of polyhydramnios may be associated with Trisomy 18. |
|
|
A patient with a known history of endometriosis who is unable to conceive and has an otherwise negative workup for infertility. TX?
|
Ovarian stimulation with Clomiphene Citrate
A GnRH agonist is used to control pelvic pain in endometriosis patients unresponsive to other hormonal treatments. A laparoscopy with treatment of endometriosis can increase fertility rates but, in this patient, is better reserved if she fails medical treatment. |
|
|
A 20-year-old G2P1 woman at 32 weeks gestation presents to Labor and Delivery with contractions every 4 minutes. On physical examination, her vital signs are: temperature 38.1; heart rate 120; respiratory rate 18, and blood pressure 110/65. Her fundus is non-tender and the rest of the physical exam is benign. Her cervix is dilated 2 cm and is 50% effaced. Fetal heart tones are in the 140s and are reassuring, overall. Her white blood cell count (WBC) is 18,000. Which of the following is the most appropriate next step in the management of this patient?
|
Perform amniocentesis!
An amniocentesis should be performed to rule out an intra-amniotic infection. This patient has an unexplained fever and elevated white blood cell count, which are concerning for an intra-amniotic infection. Delivery is not warranted at this time, as it is possible that the fever and elevated white blood cell count are from another source. Steroids should not be used until an intra-amniotic infection has been ruled out. |

