![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
|
What are the basic functions of muscles?
|
1. Movement 2. Stability 3. Glycemic Control 4. Control of openings and passageways 5. Heat production |
|
|
Movement |
Movement of body parts and organ contents—includes moving fromplace to place, movement of body contents in breathing, circulation, feedingand digestion, defecation, urination, and childbirth—it has a role incommunication.
|
|
|
Stability |
Maintain posture andprevent unwanted movement—antigravity muscles resist the pull of gravity andprevent us from falling or slumping over—stabilizes joints. |
|
|
Glycemic control |
Regulation of blood glucose concentrations within its normal range.
|
|
|
Control of openings and passageways
|
Sphincters are internal muscular rings that control the movement of food, bile, blood, andother materials within the body
|
|
|
Heat production
|
From skeletal muscles, as much as 85% of our body heat comes from these
|
|
|
What are the endomysium, perimysium, and epimysium?
|
These are types ofconnective tissue found in skeletal muscle--they are attachments between muscle and bone. Collagen fibers of muscle are continuous with those in tendons and bone
matrix. |
|
|
Endomysium
|
It is the connective tissue surrounding individual muscle cells, composed of reticular fibers, external lamina (basal lamina) and a thin areolar tissue—it allows room forcapillaries and nerve fibers
|
|
|
Perimysium
|
It is thicker connective tissue that surrounds and defines fascicles (functional bundles of musclefibers).
|
|
|
Epimysium
|
It is dense connectivetissue that surrounds the entire muscle (it is a collection of fascicles)—it isinvesting fascia of gross anatomy.
|
|
|
What are the 3 different muscle types and whatare some basic histological differences between the three?
|
(1) Skeletal muscle: striated & voluntary
(2) Smooth muscle: not striated & involuntary (3) Cardiac muscle: striated & involuntary. |
|
|
Why are skeletal and cardiac muscle referred to as striated? |
Because at the light microscope level, the tissue appears to have a regular, repeating band structure
|
|
|
What type of muscle is voluntary? |
Voluntary striatedmuscle attaches to bones, attaches to skin on the face, found in the the tongueand upper esophagus (visceral striated). It includes muscle fibers that are under conscious control. Has alternating light and dark striations.
|
|
|
What type of muscle is involuntary? |
Under unconscious control. Examples are smooth and cardiac muscle |
|
|
What type of muscle is striated? |
Skeletal and cardiac muscle |
|
|
What are the developmental precursor cells toskeletal muscle cells?
|
Myoblasts are thedevelopmental precursor to skeletal muscle fibers. Myoblasts fuse to form askeletal muscle fiber. A satellite cellcomes to sit on/attach to the muscle fiber.
|
|
|
What cells, under the optimal conditions, giverise to skeletal muscle cells following injury?
|
Unfused satellitecells can multiply to produce a small number of new myo-fibers. Most muscle repair is by fibrosis rather thanregeneration of functional muscle.
|
|
|
What is the sarcolemma? What is the function oftransverse tubules?
|
Sarcolemma hastunnel-like infoldings or transverse T tubules that penetrate the cell. The T tubules carry electric current to thecell interior to trigger the release of Ca2+ by the sarcoplasmic reticulum.
|
|
|
What carbohydrate energy storage substance isfound in skeletal muscle?
|
Glycogen for stored energy isfound in the
sarcoplasm of skeletal muscle. |
|
|
What are the structures that make up the “triad” in skeletal muscle?
|
It includes a Ttubule and two terminal cisternae.
|
|
|
What are the 3 types of myofilaments and whatare the proteins that are found in each?
|
Thick: myosin and polypeptides Thin: fibrous actin, globular actin, troponin and tropomyosin Elastic: titin *each myofibril is abundle of parallel protein microfilaments called myofilaments. |
|
|
Details of thick filaments |
Thick filaments aremade of 200 to 500 myosin molecules and is two entwined polypeptides in theshape of a golf club. They are arrangedin a bundle with the heads directed outward in a spiral array around the bundledtails. The central area is a bare zonewith no heads.
|
|
|
Details of thin filaments |
Thin filaments aremade of two intertwined strands of fibrous (F) actin and globular (G) actinwith an active site. Grooves holdtropomyosin molecules which each can block active sites of G actins. There is one small, calcium binding troponinmolecule on each tropomyosin molecule. Know that F-actin, tropomyosin, and troponin are part of thin filaments.
|
|
|
Details of elastic filaments |
Elastic filaments arespringy proteins called titin. Theyflank and anchor each thick filament to the Z disc. It helps to stabilize the thick filament,center it between the thin filaments, and prevents overstretching of thesarcomere. There are at least 7 otheraccessory proteins that are present in association with the thick and thinfilaments. These accessory proteins cananchor, and regulate length and alignment. The most clinically relevant one is dystrophin.
|
|
|
Describe the basic shape of a myosin molecule?
|
Myosin is made of twoidentical heavy chains and two pairs of light chains. The heavy chains contain a globular headprojecting from it an an angle (golf club shape)
|
|
|
What are the functional domains or “activesites” on this protein?
|
the head contains binding sites for actin and ATP, and the tails aggregate to form thick filaments.
|
|
|
What is tropomyosin and what is its functional role?
|
In thin filaments, a F-actin groove holds tropomyosin molecules that block active sites of G actins
|
|
|
What are the individual subunits of troponin andwhat are the unique functions ascribed to each?
|
It has three subunits.
(1) TnT which binds totropomyosin. (2) TnC which binds to Ca2+. (3) TnI which inhibits actin myosinbinding. |
|
|
What is the major protein of the elastic
filaments? |
springy proteinscalled titin
|
|
|
What is the function of elastic filaments?
|
Titin flank and anchoreach thick filament to the Z disc. Ithelps to stabilize the thick filament, center it between the thin filaments,and prevents overstretching of the sarcomere. There are at least 7 accessory proteins present in association withthick and thin filaments which anchor, regulate length, and alignment. The most clinically relevant is dystrophin.
|
|
|
What is dystrophin?
What is its function? |
Dystrophin is acytoskeletal protein located beneath the sarcolemma in the vicinity of each Iband and plays a role in linking F-actin through intermediate proteins tolaminin and then to the endomysium. Laminin is an extracellular matrix protein. Dystrophin is thecritical link between thin filament and muscle fibers, if it is removed, youwill no longer have connection, so you will no longer have muscle contraction.
|
|
|
What disease process is present when there is agenetic defect in dystrophin?
Are anti-inflammatory drugs used in treatment? |
Muscular dystrophy isfrom mutations in the dystrophin gene.
Yes. Some medications thatcan be used are anti-inflammatory corticosteroid medications (prednisone) tohelp improve muscle strength and delay the progression of the disease. |
|
|
Which proteins in muscle are considered
regulatory proteins? |
The regulatoryproteins are tropomyosin and troponin—they start and stop the shortening ofmuscle cells, contraction is activated by the release of calcium intosarcoplasm and its binding to troponin, troponin moves tropomyosin off theactin active sites.
|
|
|
Which proteins in muscle are considered
contractile proteins? |
The contractilemuscles are myosin and actin.
|
|
|
In skeletal muscle, what are the A, I, and H bands, and what are the Z discs?
|
A bands are dark(anisotrophic) thick filament region and affects polarized light.
I bands are lighter (isotropic) thin filamentregion and affects polarized light—it is bisected by the Z disc and anchors. |
|
|
Be able to recognize A, I, H bands and the Z discs in a micrograph of muscle
|

|
|
|
What is Duchenne's Muscular Dystrophy? |
Duchenne’s musculardystrophy is an X-linked disorder causing progressive muscle weakness. The onset is between 3 and 5 years of age andmost can’t walk by 12 years of age, and at 20 years of age require a respiratorto breath.
|
|
|
How is Duchenne's diagnosed? |
Duchenne’s is diagnosed by musclebiopsy, blood enzymes, EMG, and DNA testing. A child with this disease will have large muscular calves, but they continueto weaken due to focal fat replacement of muscle fibers in the biopsy.
|
|
|
Describe the histological tissue appearance of atypical biopsy specimen taken from a child suffering from Duchenne’s MuscularDystrophy.
|
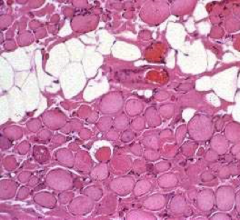
|
|
|
What is the treatment for Duchenne's? |
The current treatmentfor Duchenne’s Muscular Dystrophy is designed to help prevent or reducedeformities in the joints and spine and to allow the maintaining of mobilityfor as long as possible through physical therapy, medications, assistivedevices, and surgery.
|
|
|
What can be used to treat myotonic dystrophy? |
Myotonic dystrophycan be treated with medications for muscle spasms, stiffness, and weaknessassociated with this condition including mexiletine (Mexitil), phenytoin(Dilantin, Phenytek), baclofen, dantrolene (Dantrium), and carbamazepine(Tegretol, Carbatrol).
|
|
|
Describe compartment syndrome.
|
Compartment syndromeis mounting pressure on the muscles, nerves, and blood vessels and it triggersa sequence of degenerative events. Possible can occur from a crush injury thatcauses a surge of blood flow in, but increases the pressure and collapses theveins. Blood flow to compartment is obstructed by pressure. If poor blood flow (ischemia) persists formore than 2 to 4 hours, nerves begin to die. After 6 hours, muscles begin to die. Nerves can regenerate after pressure is relieved, but muscle damage ispermanent. Myoglobin in urine indicatescompartment syndrome.
|
|
|
How is compartment syndrome treated? |
immobilization oflimb and fasciotomy
|
|
|
What are muscle cells capable of? |
Shortening and converting ATP into mechanical energy |
|
|
What are 5 characteristics of muscle? |
1. Excitability--responsiveness 2. Conductivity--leads to contraction 3. Contractility--shortens when stimulated 4. Extensibility--muscle can be stretched 5. Elasticity--muscle returns to original length after stretching |
|
|
What are deep and superficial fascia and where are they found? |
Deep: found between adjacent muscles Superficial (hypodermis): mostly adipose tissue and is between skin and muscles |
|
|
Where do the cell bodies of somatic motor
neurons reside? |
brainstem and spinal cord
|
|
|
What is a motor unit?
|
A motor unit is eachmotor neuron and all of the muscle fibers it innervates. Motor units aredispersed throughout the muscle, when contracted together it causes weakcontraction over a wide area, and it provides ability to sustain long termcontraction as motor units take turn resting—postural control.
|
|
|
What is the purpose of having some muscles withvery large motor units and others with many very small motor units? Whatstructure of the body has very small motor units that control its movement?
|
There are fine control motorunits called small motor units—they contain as few as 20 musclefibers per nerve fiber (eye muscles are an example). For strength and power, you use large motorunits which can contain 1000 muscle fibers per nerve fiber (gastrocnemius/calfmuscle is an example).
|
|
|
What is the neurotransmitter of neuromuscularjunctions (NMJ)?
|
Acetylcholine (ACh) |
|
|
What is the NMJ? |
It is the functional connection between the nervefiber and muscle cell. A neurotransmittercalled acetylcholine (ACh) is released from a nerve fiber to stimulate musclecell and initiate contraction. Itcontains synaptic knobs that are the swollen ends of nerve fibers.
|
|
|
What is the synaptic cleft? |
The synaptic cleft isthe tiny gap between nerve and muscle cells.
|
|
|
What does the muscle sarcolemma contain? |
The muscle sarcolemmahas junctional folds that increase surface area of ACh receptors—these containacetylcholinesterase that breaks down ACh and causes relaxation.
|
|
|
What is the basal lamina? |
The basal lamina is athin layer of collagen and glycoprotein surrounding the muscle fiber and theSchwann cell of the NMJ—it separates them from the surrounding connectivetissue and occupies the synaptic cleft.
|
|
|
What ion flows into the nerve terminal of theNMJ prior to the release of neurotransmitterto the synaptic cleft?
|
Ca2+ flows into the synaptic knob prior tothe
release of the neurotransmitter. |
|
|
What organelle is found in abundance in the nerve terminal near the neurotransmitter filled vesicles?
|
Mitochondria |
|
|
Whatis the difference between a ligand gated channel and a voltage gated channel of the postsynaptic membrane (what specifically triggers opening of the gate)?
|
Ligand gates require a compound to bind to it--opensfrom acetylcholine binding to it. Voltagegates open from a difference in membrane potential.
|
|
|
Where precisely are acetylcholine receptors ofthe NMJ located? Are these muscarinic or
nicotinic receptors? |
They are in thejunctional folds of the muscle cell and are nicotinic receptors.
|
|
|
What type of muscle impairment will be caused bypesticide poisoning that inhibits cholinesterase?
|
Pesticides can act ascholinesterase inhibitors and bind to acetylcholinesterase and prevent it fromdegrading ACh—this causes spastic paralysis and possible suffocation.
|
|
|
By what mechanism does Tetanus toxin affectmuscle?
|
Tetanus/lockjaw isspastic paralysis caused by toxin of clostridium bacteria—it blocks glycinerelease in the spinal cord and causes overstimulation. Glycine is an inhibitory neurotransmitter inthe spinal cord.
|
|
|
By what mechanism does curare toxin affect muscle? |
Flaccid paralysis(limp muscles) are due to curare (plant toxin used for blowgun darts) thatcompete with ACh at nicotinic ACh receptors. It can cause respiratory arrest.
|
|
|
By what mechanism does botulinum toxin affect muscle? |
Botulism is a type offood poisoning caused by a neuromuscular toxin secreted by the bacteriumClostridium botulinum. The toxin blocksthe release of ACh and causes flaccid muscle paralysis. It has been approved by the FDA for thetreatment of muscle spasticity and for the cosmetic treatment of wrinkles,headaches, and migraines.
|
|
|
Describe the resting membrane potential (RMP).
|
Resting membranepotential is due to the excess of Na+ and cations outside of the cell and anexcess of anions inside of the cell (making the cell negative). This difference in chargeacross the membrane is called resting membrane potential. The difference in electrical charge from onepoint to another is called an electrical potential or voltage.
|
|
|
Describe an action potential?
|
An action potentialis a quick up and down voltage shift. Anaction potential at one point on a plasma membrane causes another one to happenimmediately in front of it, triggering a wave of action potentials that spread.
|
|
|
What is depolarization and what is
repolarization? What ionic events are taking place during these components ofan action potential? |
Depolarization is achange inside of the plasma membrane when it briefly becomes positive. When it becomes negative again, it is calledrepolarization. This causes ion gates toopen allowing Na+ to rush into the cell, and K+ to rush out of the cell.
|
|
|
What is an end plate potential (EPP)?
|
Na+enters shifting, RMP goes from -90mV to +75mV, then K+ exits and RMP returns to -90mV. This quickvoltage shift is called an end-platepotential (EPP)
|
|
|
What is excitation-contraction coupling?
|
Excitation-contractioncoupling is action potentials on the sarcolemma activating myofilaments.
|
|
|
What is the power stroke of muscle contraction?
|
The power stroke is when myosinhead releases ADP and phosphate as it flexes, pulling the thin filament pastthe tick filament. With the binding ofmore ATP, the myosin head extends to attach to a new active site—half of theheads are bound to a thin filament at one time to prevent slippage—thin and thick filaments do not becomeshorter, they just slide past each other.
|
|
|
What are the four actions involved in the excitation-contraction coupling? |
1. Excitation (step 1 - 5) 2. Excitation-contraction coupling (step 6 - 9) 3. Contraction (step 10 - 13) 4. Relaxation (step 14 - 18) |
|
|
What happens during excitation? |
nerve action potentials lead to action potentials inmuscle fiber (steps 1 through 5)
|
|
|
What happens during excitation-contraction coupling? |
action potentials on the sarcolemma activatemyofilaments. This refers to the evensthat link the action potentials on the sarcolemma to activation of themyofilaments for contraction. (steps 6 through 9) |
|
|
What happens during contraction? |
shortening of muscle fibers (steps 10 through 13) |
|
|
What happens during relaxation? |
return to resting length (steps 14 through 18)
|
|
|
What happens during step 1 & 2 (excitation)? |
The nerve signal opens a voltage-gated calciumchannels in the nerve synaptic knob. Calcium enters the synaptic knob and stimulates exocytosis of ACh fromsynaptic vesicles—the vesicles are sent to and fuse with the membrane. ACh released into synaptic cleft and itdiffuses across.
|
|
|
What happens during step 3 & 4 (excitation)? |
Two ACh molecules bind to each receptor protein on thesarcolemma of NMJ, which opens Na+ and K+ channels. Na+ enters shifting RMP goes from -90mV to+75mV, then K+ exits and RMP returns to -90mV. This is a quick voltage shift and is called an end plate potential(EPP).
|
|
|
What happens during step 5 (excitation)? |
The voltage change (EPP) in the end plate region opensnearby voltage-gated Na+ and K+ channels, producing an action potential thatspread over muscle surface.
|
|
|
What happens during step 6 & 7? (excitation-contraction coupling) |
Action potential spreading over the
sarcolemma entersT tubules. Voltage gated channels openin T tubules causing calcium gates to open in SR. |
|
|
What happens during step 8 & 9?
(excitation-contraction coupling) |
Calcium released by the SR binds to troponin. Troponin-tropomyosin complex changes shapeand exposes active sites on actin for the myosin head.
|
|
|
What happens during step 10 & 11 (contraction)? |
Myosin head must have an ATP bound to it. Myosin ATPase in myosin head hydrolyzes anATP molecule, activating the head and cocking it in an extended position. It binds to actin active site to form a crossbridge.
|
|
|
What happens during step 12 & 13 (contraction)? |
Power stroke, where a myosin head releases ADP andphosphate as it flexes pulling the thin filament past the thick filament. With the binding of more ATP, the myosin headextends to attach to a new active site. Half of the heads are bound to a thin filament at one time to preventslippage. Thin and thick filaments donot become shorter; they just slide past each other (sliding filament theory).
|
|
|
What happens during step 14 & 15 (relaxation)? |
Nerve stimulation declines or stops and AChrelease stops. AChE(acetylcholinesterase) breaks down ACh and the choline is reabsorbed intosynaptic knob for reuse. Stimulation ofmuscle by ACh stops.
|
|
|
What happens during step 16 (relaxation)? |
Active transport needed to pump calcium back into SR.Calsequestrin binds calcium in SR. ATP is needed for muscle relaxation as wellas muscle contraction.
|
|
|
What happens during step 17 & 18 (relaxation)? |
Loss of calcium from sarcoplasm movestroponin-tropomyosin complex over active sites. It stops the production or maintenance of tension. Muscle fiber returns to its resting lengthdue to recoil of series-elastic components and contraction of antagonisticmuscles.
|
|
|
What is the cause of rigor mortis? |
Rigor mortis: stiffening of the body about 3 to 4 hours after death. The deteriorating of sarcoplasmic reticulumreleases calcium. The calcium activatesmyosin-actin cross-bridging and then the muscle contracts, but it can’trelax. Since muscle relaxation requiresATP, and ATP production is no longer happening, it won’t relax. The fibers remain contracted untilmyofilaments decay.
|
|
|
Where is calsequestrin found and what is itsfunction?
|
It is found in thesarcoplasmic reticulum. It binds calciumto hold it in the sarcoplasmic reticulum during muscle relaxation.
|
|
|
Discuss the disease process of MyastheniaGravis.
|
It is characterizedby progressive weakness that remits with rest and is worsened by exercise. It is an autoimmune disease with antibodiesthat attack NMJ by binding ACh receptors on the post synaptic membrane inclusters.
|
|
|
What binds to ACh receptors in a person with myasthenia gravis? |
The antibodies bindto receptors to block ACh from binding—no muscle contraction can happen due tothe functioning receptor sites being reduced. They become less and less sensitive to ACh.
|
|
|
What are some of the signs of myasthenia gravis?
|
Drooping eyelids(ptosis) and double vision are some of the first signs—difficulty swallowing,weakness of the limbs, respiratory failure is possible, but most live normallifespans. It is common in women between20 and 40 years of age.
|
|
|
What treatments are available for myasthenia gravis? |
Cholinesterase inhibitors, thymus removal to dampen the immuneresponse, immunosuppressive agents like prednisone and azathioprine to suppressthe production of antibodies that destroy ACh receptors, and plasmapheresis toremove antibodies from the blood plasma.
|
|
|
What is the length-tension relationship? |
The amount of tension generated will depend on the length of muscle before it was stimulated. *Overly contracted: weak result *Too stretched: weak result *Optimum resting length: greatest force when contracted |
|
|
What is a twitch contraction?
|
It is a single brief stimulus at that voltageproducing a quick cycle of contraction and relaxation called a twitch. It lasts for less than 1/10 of a second andis not strong enough to do any useful work.
|
|
|
What is the effect of an increased stimulus
frequency on twitch contractions? |
Increased stimulusfrequency, closer stimuli,
produces stronger twitches. |
|
|
What is the effect of stimulating muscle with higher and higher voltages?
|
It causes stronger contractions because more motorunits are being recruited—called multiple motor unit summation. An example is lifting a glass of milk versusa whole gallon of milk.
|
|
|
What is the effect of stimulating muscle with higher and higher frequencies ofvoltage?
|
It generates gradually more strength of
contraction. |
|
|
What are treppe muscle contractions?
|
Treppe muscle contractions are when each twitch hastime to recover but develops more tension than the one before.
|
|
|
What is tetanus in muscle contraction?
|
If a muscle fiber isstimulated so rapidly that it does not relax at all between stimuli, a smooth,sustained contraction called tetanus occurs.
|
|
|
What is an isometric muscle contraction? |
Isometric muscle contraction develops tension withoutchanging the muscles’ length—it contracts at the cellular level but tension isabsorbed by the series of elastic components and is resisted by the weight ofthe load—it is important in postural muscle function and antagonistic musclejoint stabilization.
|
|
|
What is concentric muscle contraction? |
Concentric/isotonic contraction is the same tension whileshortening. It starts with internaltension building to the point that it overcomes the resistance. The muscle now shortens, moves the load, andmaintains essentially the same tension from then on.
|
|
|
What is eccentric muscle contraction? |
Eccentric/isotonic contraction is the same tension whilelengthening. The muscle lengthens, movesthe load, and maintains essentially the same tension from then on. A woman slows the decent of a dumbbell, theeccentric muscle contraction acts as a brake to keep from dropping the weight.
|
|
|
What are the sources of ATP for muscle
contraction during the first few seconds through 10 seconds of muscle contraction? |
Aerobic respiration using oxygen from myoglobin andthe phosphagen system.
|
|
|
What are the enzymes used in the phosphagen system?
|
Myokinase transfers Pi groups from one ADP to anotherforming ATP. Creatine kinase transfers Pi groups from a phosphate storagemolecule creatine phosphate to make ATP.
|
|
|
What is the Glycogen-lactic acid system?
|
The glycogen-lactic acid system takes over when thephosphagen system is exhausted. It worksuntil the cardiopulmonary function can catch up with the muscles oxygendemand. Glycolysis produces enough ATPfor 30 to 40 seconds of maximum activity (basketball or running around baseballdiamonds). There is a net gain of 2 ATPfor each glucose molecule consumed and converted to lactic acid.
|
|
|
What is the phosphagen system?
|
The phosphagen system supplies most ATP for briefexercise. The result is power enough fora 1-minute brisk walk or 6 seconds of sprinting.
|
|
|
How are long term energy needs provided for in muscle?
|
Aerobic respiration is needed for prolongedexercise. It produces 36 ATPs perglucose molecule. After 40 seconds ofexercise, respiratory and cardiovascular systems must deliver enough oxygen foraerobic respiration. Oxygen consumptionrates increase for the first 3 to 4 minutes and then levels off to a steadystate. For exercise lasting more than 10minutes, more than 90% of ATP is produced aerobically. Limits are set by depletion of glycogen andblood glucose, loss of fluid and electrolytes.
|
|
|
What are the processes that lead to muscle
fatigue? |
Fatigue isprogressive weakness from use. ATPsynthesis declines as glycogen is consumed. ATP shortage limits sodium-potassium pumps’ ability to maintain membranepotential and excitability. Lactic acid,lowering pH, inhibits enzyme function necessary for contraction. Accumulation of extracellular K+hyperpolarizes the cell. Each actionpotential releases K+ from the sarcoplasm to the ECF. Motor nerve fibers use up theiracetylcholine—this is termed junctional fatigue.
|
|
|
What is VO2 max?
|
It is the point at which the rate of oxygenconsumption reaches a plateau and does not increase further with an addedworkload. It is proportional to bodysize, peaks at age 20, is larger in trained athletes and males. This maximumoxygen uptake determines the ability to maintain high intensity exercise formore than 5 minutes.
|
|
|
What is exercise post oxygen consumption via heavy breathing used for?
|
It is repayment of oxygen debt. Aerobic respiration supported by cardiopulmonary function. Aerobic respiration produces more ATP,requires a continuous oxygen supply, produces water and carbon dioxide, themuscle uses glucose during activity, but mostly fatty acids during rest.
Anaerobic fermentation produces limited ATP, without oxygen,and produces toxic lactic acid. |
|
|
Describe slow twitch muscle. |
Slow twitch=type I skeletal muscle fiber. They are slow oxidative, slow twitchfibers. They are deep red in color dueto an abundance in mitochondria, myoglobin, and capillaries. It is adapted for aerobic respiration and isresistant to fatigue. They exhibit arelatively long twitch in response to a single stimulus. For example, the soleus (calf muscle) andpostural muscles of the back (100msec/twitch) are composed of mainly these highendurance fibers.
|
|
|
Describe fast twitch muscle. |
Fast twitch=type II skeletal muscle fiber. These are fastglycolytic, fast twitch fibers. They arewhite in color due to having fewer mitochondria, capillaries, and lessmyoglobin. They are rich in enzymes forphosphagen and glycogen lactic acid systems. The sarcoplasmic reticulum releases calcium quickly so contractions arequicker (7.5msec/twitch). It produceslactic acid and fatigue more readily. Anexample is extraocular eye muscles, gastrocnemius, and biceps brachii.
|
|
|
Describe intermediate twitch muscle. |
Intermediate=type IIA muscle fiber. These combine fast twitch responses withaerobic fatigue resistant metabolism. They are relatively rare, except in some endurance trainedathletes. All fibers of one motor unitbelong to the same physiological type. All muscles are composed of both type I and type II, but the proportionsdiffer from one muscle to another. Proportions of muscle type are genetically determined.
|
|
|
Compare the proportion of slow oxidative and fast glycolytic fibers in the quadriceps muscle of athletes |
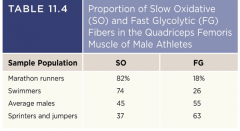
|
|
|
What are the 6 factors that determine the strength of muscle contraction? |
(1) Muscle size and fascicle arrangement (crosssectional area), (2) length-tension relationship—muscle at resting length canproduce more force than one excessively shortened or stretched, (3) size ofmotor units, (4) multiple motor unit summation—recruitment of many motor unitsbecomes more efficient with training and can also occur under extreme stress,(5) temporal summation from nerve impulses, and (6) fatigued muscle contractsmore weakly.
|
|
|
What changes take place in skeletal muscle
during resistance training versesendurance training? |
During endurance training, like aerobic exercise, slowtwitch fibers, increase of mitochondria, glycogen, and density ofcapillaries. During resistance training,like weight lifting, it stimulates cell enlargement due to synthesis of moremyofilaments.
|
|
|
Compare characteristics of cardiac muscle (stimulus for contraction, type of innervation, length of contraction, energy source, mitochondria number and size, vulnerability to oxygen deficit) with that of skeletal muscle.
|
Cardiac muscle has thick cells shaped and branched. They are linked to each other at intercalateddiscs. They have electrical gapjunctions that allow cells to stimulate their neighbors and mechanicaljunctions to keep cells from pulling apart. The sarcoplasmic reticulum is less developed, but large T tubules admitCa2+ from ECF. Damaged cells can berepaired by fibrosis.
T tubules are larger in cardiac muscle than skeletalmuscle. The T tubules are located at a Zdisc in cardiac muscle—in skeletal muscle they are at the A-I junction. Cardiac muscle has a diad (SR and Ttubule). Large mitochondria span thedistance between T tubules in cardiac muscle. 25% of cardiac muscle cell volume is occupied by mitochondria (it isonly 2% in skeletal muscle). Cardiac muscle is autorhythmic due to pacemaker cells. The heart also receives fibers from theautonomic nervous system that increase or decrease the rate and strength ofcontractility. It does not exhibit quicktwitches like skeletal muscle—instead, it will maintain tension for about 200 –250 milliseconds to allow the heart time to expel blood. Uses aerobic respiration almostexclusively. It has large mitochondriathat make it resistant to fatigue and it is very vulnerable to interruptions inoxygen supply. |
|
|
What occurs during a myocardial infarction? What can be measured in the blood to detectthis?
|
Cardiac muscle death is also called myocardialinfarction (MI). Death (necrosis) ofcardiac muscle cells due to prolonged ischemia (lack of blood). It can be repaired by fibrous connectivetissue, so function is lost in this region of the heart. Serum cardiac specifictroponin (cardiac enzymes) is measured to assess damage.
|
|
|
What are some characteristics of smooth
muscle? |
It is fusiform cells with one nucleus. It is about 30 to 200 microns long and about5 to 10 microns wide. There are nostriations, sarcomeres, or Z discs. Thin filaments attach to dense bodiesscattered throughout the sarcoplasm and on sarcolemma. SR is scanty and has no T tubules. Calcium for contraction comes fromextracellular fluid. If present, nervesupply is autonomic, like the release of ACh or norepinephrine. It is capable of mitosis and hyperplasia, forexample, a pregnant uterus grows by adding more myocytes.
|
|
|
What are dense bodies in smooth muscle? From where does the predominant source of calcium required for smooth muscle contraction come?
|
Calcium for contraction comes from extracellularfluid. Thin filaments attach to densebodies scattered throughout the sarcoplasm and on the sarcolemma. Dense bodies are considered the substitutionfor Z discs.
|
|
|
Describe multi-unit smooth muscle. Where is it typically found?
|
It is typically found in the largest arteries, iris, pulmonary airpassages, and arrector pili muscles of hair follicles. The terminal nerve branches synapse on individual myocytes andform a motor unit. Each motor unitcontracts independently of the other motor units.
|
|
|
Describe single-unit smooth muscle. Where is it typically found?
|
They are widespread and typically found in most blood vessels, and thedigestive, respiratory, urinary, and reproductive tracts. It is often called visceral smoothmuscle. In many hollow viscera there aretwo or more layers—with an inner circular and outer longitudinal musclelayer. They are electrically coupled bygap junctions. A large number of cellscontract as a unit.
|
|
|
Which type of smooth muscle uses gap junctions and which uses nerve terminals on individual muscle cells?
|
Single unit smooth muscle uses gap junctions. Multi unit smooth muscle uses nerve terminalson individual muscle cells.
|
|
|
What is the calcium binding protein in smooth muscle?
|
It is called Calmodulin and it binds Ca2+. There is no troponin. It is typically found in the walls of holloworgans and blood vessels.
|
|
|
What is the major intermediate filament protein in all smooth muscle cells?
|
Thin filaments are in all smooth muscle cells.
|
|
|
Describe the various methods by which calcium channels can be triggered to open insmooth muscle?
|
Calcium channels triggered to open by voltage, hormone/ligandgated channels, neurotransmitters, or cell stretching. Calcium ions bind to calmodulin associatedwith thick filaments. This activateslight-chain myokinase, which transfers a phosphate group from ATP to the headof the myosin, this then activates myosin ATPase and enables it to bind toactin. Power stroke occurs when ATP ishydrolyzed.
|
|
|
Are there smooth muscle pacemaker cells in
certain organs? |
Yes. Pacemaker cells in the GI tract areauto-rhythmic, meaning they spontaneously depolarize. This sets off waves of contraction throughoutan entire layer of muscle. It contractsslower than cardiac muscles. It isinvoluntary and contracts without nerve stimulation—can be stimulated byhormones, CO2, low pH, stretching, and O2 deficiency.
|
|
|
Comparethe efficiency of ATP usage between smooth muscle and skeletal muscle. Comparecontraction and relaxation rate.
|
Thick filaments pull on the thin ones, the thinfilaments pull on the dense bodies and membrane plaques. Intermediate filaments of cytoskeletonattached to dense bodies to the plasma membrane. It shortens the entire cell in a twistingfashion, like wringing out a wet towel. Contraction and relaxation are very slow in comparison because of slowmyosin ATPase enzyme and slow pumps that remove Ca2+. It uses 10 to 300 times less ATP to maintainthe same tension. (latch-bridgemechanism)
|
|
|
Describethe latch-bridge mechanism.
|
This mechanism maintains tetanus (muscle tone) for aprolonged time without consuming ATP. Itkeeps arteries in a state of partial contraction (vasomotor tone). A loss ofthis tone can cause a dangerous drop in blood pressure. It keeps intestines partially contracted.
|
|
|
How does stretch affect an organ that contains smooth muscle in its walls?
|
Stretch opens mechanically gated calcium channelscausing muscle response. For example,food entering the esophagus brings on peristalsis. Stress relaxation response is necessary forhollow organs that gradually fill, like the urinary bladder—when it isstretched, tissue briefly contracts then relaxes. It must contract forcefully when greatlystretched, thick filaments have heads along their entire length and no orderlyfilament arrangement, and no Z discs. Plasticityis the ability to adjust tension to degree of stretch such as an empty bladdernot being flabby.
|

