![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
Functions of Blood |
•Transportof gases, nutrients and waste products •Transportof processed molecules •Transportof regulatory molecules •Regulationof pH and osmosis •Maintenanceof body temperature •Protectionagainst foreign substances •Clotformation |
|
|
Characteristics of Blood |
•Typeof connective tissue •Sticky •Heavierthan water •O2content determines color •Temp.slightly higher than rest of body •Males(5-6 L), females (4-5 L) |
|
|
Composition of Blood |
Plasma Formed Elements |
|
|
Plasma |
- 55% of total blood - pale,yellow liquid that surrounds cells - 91%water, 7% proteins, and 2% other |
|
|
FormedElements |
- 45% of total blood - cellsand cell fragments - erythrocytes,leukocytes, thrombocytes |
|
|
Plasma Proteins |
•Albumin: - 58%of plasma proteins - helpsmaintain water balance •Globulins: - 38%of plasma proteins - helpsimmune system •Fibrinogen: - 4% ofplasma proteins - aidsin clot formation |
|
|
Erythrocytes
|
•Redblood cells (RBC) •Disk-shapedwith thick edges •Nucleusis lost during development •Livefor 120 days •Function: transport O2 to tissues |
|
|
Hemoglobin |
•Maincomponent of erythrocytes •TransportsO2 •Eachglobin protein is attached to a hememolecule •Each hemecontains one iron atom •O2binds to iron •Oxyhemoglobin: -hemoglobinwith an O2attached |
|
|
Production of Erythrocytes
|
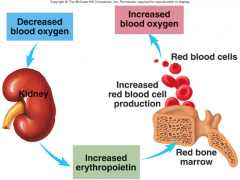
1.Decreasedblood O2levels cause kidneys to increase production of erythropoietin. 2.Erythropoietinstimulates red bone marrow to produce more erythrocytes. 3.Increasederythrocytes cause an increase in blood O2levels. |
|
|
Fate of Old Erythrocytes and Hemoglobin |
•Old rbc’s areremoved from blood by macrophages in spleen and liver •Hemoglobinis broken down •Globinis broken down into amino acids •Hemoglobin’siron is recycled •Heme isconverted to bilirubin •Bilirubinis taken up by liver and released into small intestine as part of bile |
|
|
Hemoglobin breakdown |

|
|
|
Leukocytes
|
•Whiteblood cells (WBC) •Lackhemoglobin •Largerthan erythrocytes •Containa nucleus •Functions: - fightinfections - remove dead cells and debris by phagocytosis |
|
|
Types of Leukocytes |
•Granulocytes: containgranules 1. Neutrophils 2. Eosinophils 3. Basophils •Agranulocytes: nogranules 1. Monocytes 2. Lymphocytes: |
|
|
Neutrophils |
- most common - remain in blood for 10-12 hours then move to tissues - phagocytes |
|
|
Eosinophils |
reduceinflammation |
|
|
Basophils |
- least common - releasehistamine and heparin |
|
|
Monocytes |
- largest - produce macrophages |
|
|
Lymphocytes |
- immuneresponse - several different types (T cells and B cells) - leadto production of antibodies |
|
|
Platelets
|
- bloodclotting cells - produced in red bone marrow |
|
|
Hematopoiesis |
•processof blood cell formation •In aninfant, occurs in liver, thymus gland, spleen, lymph nodes, and red bonemarrow. •Adultsoccurs mainly in red bone marrow. •Stemcell: originalcell line |
|
|
Blood Loss |
•Whenblood vessels are damaged, blood can leak into other tissues and disrupt normalfunction. •Bloodthat is lost must be replaced by production of new blood or by a transfusion. |
|
|
Preventing Blood Loss |
1.Vascularspasm : temporaryconstriction of blood vessel 2.Plateletplugs : canseal up small breaks in blood vessels
3.Bloodclotting (coagulation) |
|
|
Blood Clotting
|
•Bloodcan be transformed from a liquid to a gel •Clot: - networkof thread-like proteins called fibrin that trap blood cells and fluid - depends on clotting factors •Clottingfactors: - proteinsin plasma - onlyactivated following injury - madein liver - require vitamin K |
|
|
platelet adhesion occurs ? |
1. platelet adhesion occurs when von Willebrand factor connects collagen and platelets 2. during the platelet release reaction, ADP, thromboxanes, and other chemicals are released and activate other platelets 3. platelet aggregation occurs when fibrinogen receptors on activated platelets bind to fibrinogen, connecting the platelets bind to fibrinogen, connecting the platelets to one another. the accumulating mass of platelets forms a platelet plug. |
|
|
Steps in Clot Formation |

1.Injuryto a blood vessel causes inactive clotting factors to become activated due toexposed conn. tissue or release of thromboplastin
2.Prothrombinase(clottingfactor) is formed and acts upon prothrombin
3.Prothrombinisswitched to its active form thrombin
4.Thrombinactivatesfibrinogen intoits active form fibrin
5.Fibrinformsa network that traps blood (clots) |
|
|
Control of Clot Formation |
•Clotsneed to be controlled so they don’t spread throughout the body •Anticoagulants: - preventclots from forming - Ex. Heparin and antithrombin •Injurycauses enough clotting factors to be activated that anticoagulants can’t workin that particular area of the body |
|
|
Clot Retraction and Fibrinolysis |
•Clotretraction: - condensingof clot - serumin plasma is squeezed out of clot - helpsenhance healing •Fibrinolysis: - process of dissolving clot - plasminogen(plasma protein) breaks down clot (fibrin) |
|
|
Blood Reactions |
•Injuryor surgery can lead to a blood transfusion •Transfusionreactions/Aggulination: clumpingof blood cells (bad)
•Antigens: moleculeson surface of erythrocytes
•Antibodies: proteinsin plasma
•Bloodgroups: namedaccording to antigen (ABO) |
|
|
blood |
•O areuniversal donors because they have no antigens •TypeA can receive A and O blood •TypeB can receive B and O blood •TypeAB can receive A, B, AB blood •TypeO can only receive O blood |
|
|
Rh Blood Group |
•Rhpositive means you have Rh antigens •95-85%of the population is Rh+ •Antibodiesonly develop if an Rh- person is exposed to Rh+ blood by transfusion or frommother to fetus |
|
|
Example of Rh Reaction |
•Ifmother is Rh- and fetus is Rh+ the mother can be exposed to Rh+ blood if fetalblood leaks through placenta and mixes with mother’s blood. •First timethis occurs mother’s blood produces antibodies against antigens. •Anyrepeated mixing of blood causes a reaction. |
|
|
Hemolytic Disease of Newborn |
•Whatis it? - occurs when mother produces anti-Rh antibodies that cross placenta andagglutination and hemolysis of fetal erythrocytesoccurs - canbe fatal to fetus - prevented if mother is treated with RhoGAM which contains antibodies against Rhantigens |
|
|
Diagnostic Blood Tests |
•Completeblood count: provides information such as RBC count,hemoglobin, hematocrit, and WBC count •Hematocrit: % oftotal blood volume composed of RBC •Hemoglobin: - determinesamount of hemoglobin - indicate anemia •Prothrombintime: timeit takes for blood to begin clotting (9-12 sec.) •Whiteblood cell count: total number of wbc •Whiteblood cell differential count: - Determines the % of each 5 kinds of leukocytes - neutrophils: 60-70% - lymphocytes: 20-25% - monocytes: 3-8% - eosinophils: 2-4% - basophils: 0.5-1% |
|
|
White Blood Cell Disorders |
Leukopenia Leukocytosis |
|
|
•Leukopenia |
- low wbc count - caused by radiation, chemotherapy drugs, tumors, viral infections |
|
|
Leukocytosis |
- high wbc count - caused by infections and leukemia |

