![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
146 Cards in this Set
- Front
- Back
|
Half-life of mast cell tryptase? |
B
NICE Guidelines Anaphylaxis “Very low-quality evidence from six observational studies including 147 patients showed that the half-life of tryptase ranged from 30 minutes to 300 minutes (median 90 minutes)” Mayo Medical Laboratories After anaphylaxis, mast cell granules release tryptase; measurable amounts are found in blood, generally within 30 to 60 minutes. The levels decline under first-order kinetics with half-life of approximately 2 hours. |
|
|
Best single predictor of difficult intubation in obese patient? |
Pretracheal tissue Volume or Neck Circumference are best single predictors.
|
|
|
Endocarditis prophylaxis is appropriate in? |
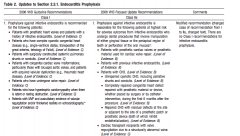
A |
|
|
Emergency caesarean section for foetal distress (and foetal acidosis on scalp probe?). what is best option to raise gastric pH preop: |
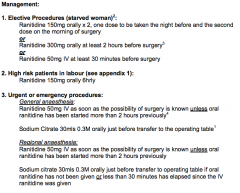
A
Given urgency of case. Most rapid acting. If 30min, consider Ranitidine iv 50mg. If 2hr, consider oral Ranitidine 300mg PPI require 12hrs
Ref: Obstetric Anaesthesists' Association UK |
|
|
Most common cause of mortality post transfusion? |
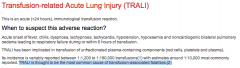
A
Ref: Transfusion.com.au |
|
|
Most common cause of awareness?
A. Failure to check apparatus |
Human error on many other versions of this question |
|
|
Apnoeic oxygenation in obese patient can be increased by
A. Sniffing position B. Prone C. Supine D. Lateral E. Head up |
E
|
|
|
Best renal protection for endoluminal AAA repair?
A. NaCl B. NAC |
A |
|
|
Indicator in sodalime? |
A |
|
|
Desflurane vaporiser heated because:
A. High SVP |
A
88.5 kPa at 20C |
|
|
What is NOT a disadvantage of drawover vaporizer?
A. Basic temperature compensation B. Basic flow compensation |
Previously remembered version included:
Can not use Sevoflurane |
|
|
FOB - can see a trifurcation. Where are you? |

A |
|
|
White cylinder with grey shoulder? |
A |
|
|
Photograph of an Arndt endobronchial blocker. Orifice labelled 'X'. What goes in 'X'?
A. Bronchoscope |

A
|
|
|
Intubating over a bougie. Rotate ETT?
A. 90 degrees anticlockwise B. 90 degrees clockwise C. 270 degrees anticlockwise D. 45 degrees either direction |
A
|
|
|
Air bubble leads to decreased: |
B |
|
|
All of the following may be associated with ulcerative colitis EXCEPT |
C
Psoriasis/Psoriatic Arthritis is associated with Crohn's, not UC |
|
|
At what valve area do you begin to get symptoms, at rest, with mitral stenosis? |
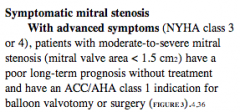
D |
|
|
75 year old with non-valvular AF usually on warfarin has their warfarin stopped for one week. What is their daily risk of stroke? |
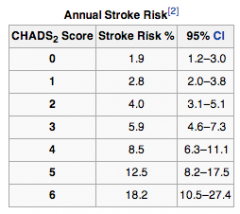
C |
|
|
Abnormal Q waves are NOT a feature of the ECG in |
D
Features Digitalis toxicity: arrhythmias, VEBs Digoxin effect on ECG: prolonged PR, sagging ST segment, VEB, arrhythmias, Short QT, T wave abnormality, U wave |
|
|
cTnI remains elevated for up to?
A. 5-14 days |
A |
|
|
With regard to Digoxin toxicity which of the following is NOT a feature? |
Clinical Features |
|
|
Inverted p-waves in lead II may be caused by? |
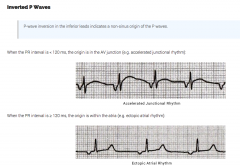
A
Junctional rhythm or ectopic pacemaker
Ref: LITFL |
|
|
Hb 80 g/L with reticulocyte 10%:
A. Hereditary spherocytosis |
A |
|
|
Pulsus paradoxus in constrictive pericarditis:
A. Decreased BP with inspiration B. Decreased BP with inspiration greater than normal |
B |
|
|
Which type of aortic dissection is typically managed non-operatively?
A. Debakey Type I B. Debakey Type II C. Stanford A D. Stanford B E. Stanford C |
D |
|
|
Absolute CI to the sitting position in neurosurgical patient? |
A |
|
|
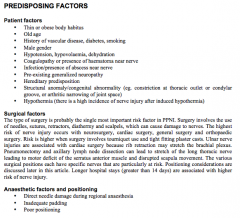
Acute visual loss after non-ocular surgery is most commonly caused by |
A
ION post common cause of post-operative blindness (Ant>Post) |
|
|
When do most patients with SAH rebleed?
A. 0-24 hours |
A
“Rebleeding after initial aneurysmal subarachnoid hemorrhage (SAH) can have substantial impact on overall patient outcome. While older studies have suggested rebleeding occurs in about 4% of patients during the first day after initial aneurysmal bleed” |
|
|
Unstable patient. Suspect aortic dissection. Most appropriate investigation? |
A
|
|
|
Contraindication to IABP?
A. AR |
A
|
|
|
During prolonged trendelenburg positioning there is:
A. No change in ICP B. No change in IOP C. Increased pulmonary compliance D. Increased myocardial work E. No increased pulmonary venous pressures |
D
|
|
|
During scoliosis surgery with monitoring of somatosensory evoked potentials, which tract are they mainly monitoring?
A: Dorsal column B: Spinothalamic tract C: Lateral Corticospinal tract D: Cerebrospinal tract E: Anterior horn cells |
A |
|
|
Estimate GCS post head-trauma. E - Response to pain V - Mumbling incoherently M - Withdraws to pain (attempted IV cannulation)
A. 8 B. 9 |
A |
|
|
Incidence of headache in first week post-partum?
39% |
CEACCP - Postpartum headache: diagnosis and management 2011
|
|
|
Oxycodone 20mg SR / Naloxone 20 mcg:
A. Decreased constipation B. Reduced risk of drug misuse/abuse |
A
|
|
|
Bowel surgery patient. Best method for intraoperative optimization of fluid therapy?
A. Arterial pulse pressure contour analysis B. CVP C. PAOP D. UO |
A
Perhaps SVV or oesophageal doppler would be better? Update in Anaesthesia - Enhanced recovery after surgery - current trends in perioperative care “Accurate fluid management and resuscitation requires regular reassessment of physiological parameters and, where available, invasive haemodynamic monitoring. Historically this has been provided by pulmonary artery catheters, but these are increasingly being replaced by targeted stroke volume optimisation with oesophageal Doppler probes. Given the relative simplicity and lack of complications, where available the latter is the recommended method of guiding fluid administration in the operating room” |
|
|
In what proportion of people is the AV node supplied by the R coronary artery?
|
Anatomy for Anaesthetist:
“The atrioventricular node is perfused by the right coronary artery in 80% of subjects” |
|
|
Epidural block to T2 causes all of the following EXCEPT:
A. Bradycardia B. Vasodilatation C. Reduced circulating catecholamines D. Dyspnoea E. Elevated PaCO2 |
E
|
|
|
Preoperative autologous blood donation results in less:
A. Cost B. Incompatible transfusion C. Less blood wastage D. Less unnecessary transfusion |
B
|
|
|
You see a patient in your clinic for a total knee replacement. He is 65 and has atrial fibrillation for which he takes dabigatran. He is otherwise well. A spinal anaesthetic is planned. What is the correct advice regarding his medication? |
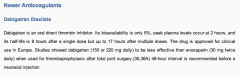
B
NYSORA |
|
|
Day 4 epidural. On 40 mg SC enoxeparin daily postoperatively (8 pm). When is the most appropriate time to remove the epidural? |
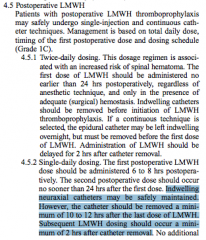
A
And at least two hours before next dose |
|
|
Penetrating injury to chest. What part of the heart most likely injured?
A. RV B. LV C. RCA |
A |
|
|
Regarding a Thallium scan:
A. High NPV B. Less useful in comparison to a DSE |
A
|
|
|
What is NOT a contraindication to MRI?
A. Pulmonary artery catheter B. Arterial line C. Scissors D. Coiled ECG cable E. Laryngoscope |
B
Blue Book 2005 “Invasive blood pressure transducers: These are not ferromagnetic, and are safe to use. Transducer cables should be kept out of the magnet bore, so as to avoid imagedistortion” MRIsafety.com “There is at least one report of a cardiovascular catheter (Swan-Ganz Triple Lumen Thermodilution Catheter) that "melted" in a patient undergoing MR imaging. This catheter contained a wire made from a conductive material that was considered to be responsible for this problem. Thus, there are realistic concerns pertaining to the use of similar devices in patients undergoing MR examinations” |
|
|
The nerve supplying area of skin between greater trochanter and iliac crest: |

A
labelled as Last Thoracic nerve on diagram |
|
|
In infants with congenital pyloric stenosis |
D |
|
|
Preoperative assessment shows a Mallampati (ML) score of III and thyromental distance (TMD) of < 6cm. A grade 3 to 4 on Cormark and Lehane is predicted. Compared to the ML score, the TMD is |
B |
|
|
Recognised weaknesses of systematic reviews include all of the following EXCEPT
A. publication bias B. duplicate publication C. study heterogeneity D. inclusion of outdated studies E. systematic review author bias |
E
|
|
|
What drug should NOT be used for tocolysis in 32/40 female? |
A
Other remembered options include Clonidine, which would be more correct. |
|
|
Following an eclamptic seizure the dose of MgSO4 is?
A. 1 gram B. 4 grams |
B
The regimen recommended by the Collaborative Eclampsia Trial is 4-5 g MgSO4 intravenously over 5 min |
|
|
An indication for NON-operative management of blunt liver trauma in adults is
A. absence of peritoneal signs B. a haemodynamically stable patient C. a haemopertitoneum of LESS than 500 ml D. a LOW grade injury on CT scan E. severe chronic obstructive airway disease |
B
|
|
|
Initial dose of IV GTN to relax the uterus is?
A. 5 mcg B. 50 mcg C. 200 mcg |
B
|
|
|
Dilated CM (LVEF 30%). No dyspnoea with ADLs. Best management?
A. Start ACEI B. Stop beta-blocker |
A
|
|
|
CTG [pictured] demonstrating late decelerations. Most likely cause?
A. Fetal asphyxia B. Head compression C. Cord compression D. Uteroplacental insufficiency |
A
Perinatology.Com - Fetal Heart Rate Monitoring “Early decelerations appear to be caused by vagal discharge produced when the head is compressed by uterine contractions. The onset and depth of early decelerations mirror the shape of the contraction, and tend to be proportional to the strength of the contraction. Late decelerations occur when a fall in the level of oxygen in the fetal blood triggers chemoreceptors in the fetus to cause reflex constriction of blood vessels in nonvital peripheral areas in order to divert more blood flow to vital organs such as the adrenal glands, heart, and brain. Constriction of peripheral blood vessels causes hypertension that stimulates a baroreceptor mediated vagal response which slows the heart rate. The time consumed in this two step process accounts for the delay in the timing of the deceleration relative to the contraction” |
|
|
If a patient experiences parasthesia in the little finger during supraclavicular brachial plexus block, the needle is in proximity to the
A. posterior cord B. middle trunk C. Ulnar nerve D. lower trunk E. medial cord |
D
|
|
|
A diagnostic test has a sensitivity of 90% and a specificity of 99% in detecting a certain disease. From this we can conclude that
A. the false positive rate of this test is 1% B. the false negative rate of this test is 1% C. the positive predictive value of this test is 90% D. the negative predictive value of this test is 90% E. this test would be a useful screening test for this disease |
A
False Positive Rate = 1 - specificity False Negative Rate = 1 - sensitivity |
|
|
SVRI.
A. SVR x BSA B. SVR / BSA |
A
|
|
|
The features of Pierre Robin sequence include cleft palate, micrognathia and:
A. Glossoptosis B. Craniosynostosis C. Macroglossia D. Microstomia |
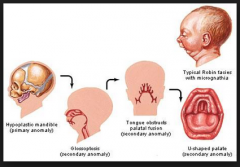
A |
|
|
What is the ratio of MAC awake:MAC of sevoflurance
a. 0.2 b. 0.34 c. 0.5 |
B
|
|
|
Essential diagnostic criteria on ECG for LBBB
A. Loss of septal Q's in V5 and V6 B. RSR in V1 C. Large slurred S in V6 D. T-waves opposite to direction of QRS E. QRS duration minimum 0.2 s |
A |
|
|
A pregnant lady is undergoing neuroradiological coiling of a cerebral aneurysm. At what gestation should intraoperative monitoring of the fetus occur? |
B |
|
|
When instructing ward staff on monitoring for respiratory depression in a patient using PCA (patient controlled analgesia) you would advise that early respiratory depression is best detected by monitoring |
E |
|
|
Trauma patient. CXR (not given): air fluid levels adjacent to heart/diaphragm/ribs.
A. Ruptured diaphragm B. Hiatus hernia |
A
B is also possible |
|
|
Intraoperative pediatric arrest during scoliosis surgery most likely due to? |
A |
|
|
Endocarditis prophylaxis in patient with MVR appropriate for? |
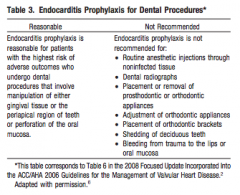
A
2008 Update - prophylaxis no longer required for GI/GU surgery. |
|
|
A man is working with electrical appliances at home with a residual current device. If he touches the active and the neutral (was it neutral or earth) wire he will suffer |
D
RCD would protect from macroshock within 40ms |
|
|
Severe asthma attack. Given continuous nebs & IV hydrocortisone but not responding. PaCO2 low. SpO2 low. Next appropriate treatment? |

A |
|
|
Atrial septal defect, where is the murmur heard the loadest? |
A |
|
|
Best position for IABP is 1-2 cm: |

A
Image courtesy of Radiopedia.org |
|
|
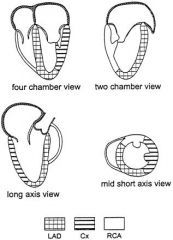
Blood flow across which of the following is used to estimate pulmonary artery pressures during echocardiography?
A. Tricuspid valve B. Pulmonary valve C. Mitral Valve |
A
|
|
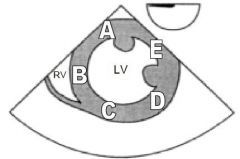
The diagram below is of a transgastric short axis view obtained during a transoesophageal echocardiography examination. Which letter corresponds to the area supplied by the right coronary artery? |
A |
|
|
Cephalothin doesn't cover:
a. Proteus b. E coli c. Staph d. Strep e. Pseudomonas |
E
|
|
|
CHADS2 score. Which is not a feature? |
B
CCF +1
However, gender is included in CHA2DS2-VaSc |
|
|
A 60kg female is given 50 mg of rocuronium, she is unable to be intubated, what dose of sugamadex is required to reverse the rocuronium
a. 240 b. 800 c. 960 |
C |
|
|
Periop clinic reviewing a patient with chronic/ end stage renal failure. Her calcium found to be low. He most certainly have
A. Primary hyperparathyroidism B. Secondary hyperparathyroidism C. Tertiary hyperparathyroidism |
B
|
|
|
Meconium stained liquour but neonate delivered is vigorous. Rationale for NOT suctioning the neonate? |
B |
|
|
Post CEA on ward, patient seizes. BP has been hard to control. What to do to prevent further seizures? |
A
Cerebral Reperfusion Syndrome: Triad of headache, seizures, focal neurology. |
|
|
National labelling standards endorsed by ANZCA. What colour should the label on a brachial plexus catheter infusion be?
A. Red B. Blue C. Beige D. Yellow E. Pink |
D |
|
|
Which of the following are feature of Conn’s syndrome? |
A
Hyperaldosteronism leads to increased Na reabsorption in exchange for K+. No effect on glucose. |
|
|
A patient has suffered flash burns of the upper half of the left upper limb, all of the left lower limb and the anterior surface of the abdomen. The approximate percentage of the body surface which has been burned is
A. 18% B. 23% C. 32% D. 41% E. 48% |
C |
|
|
Dural Sac ends at what level in a neonate?
A. L1 B. L3 C. L5 D. S1 E. S3 |
E |
|
|
SpO2 90%. No IV access. Place LMA and laryngospasm. Most appropriate course of action? |
B
|
|
|
Incarcerated inguinal hernia in a child with a mild URTI. Most appropriate course of action? |
C
|
|
|
What is the half life of clopidogrel? |
A
|
|
|
Patient with subdural hematoma and PPM for ?AV ablation. PPM technician >1 hour away. Surgeon wishes to proceed immediately. Do you? |
E |
|
|
Which of the following does NOT occur following bilateral lung transplant?
A. Impaired mucociliary clearance B. Impaired lymphatic drainage C. Impaired HPV |
C
“Hypoxic pulmonary vasoconstriction is intact in the pulmonary allograft so during an episode of rejection, pulmonary blood flow may be directed away from the transplanted lung” |
|
|
20 kilogram child suffered 15% full thickness burns 6 hours ago. Optimum crystalloid fluid volume resuscitation for the first hour is
A. 160 ml B. 260 ml C. 360 ml D. 460 ml E. 660 ml |
E
half in first 8 hours and half in 16 hours
Plus need to give maintenance fluid via 4/2/1 rule = 60ml/hr
600 + 60 = 660ml |
|
|
Complications of mediastinoscopy include all of the
following EXCEPT A. air embolism B. cardiac laceration C. pneumothorax D. recurrent laryngeal nerve palsy E. tracheal compression |
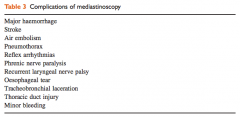
B |
|
|
What sign most suggests a significant murmur in a child?
A. 4/6 loudness B. ????vibratory/flutter sound |
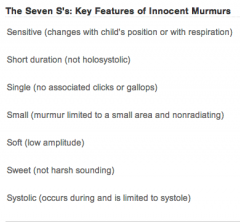
A |
|
|
Thoracodorsal nerve arises from?
|
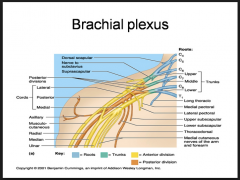
The thoracodorsal nerve is a branch of the posterior cord of the brachial plexus, and is made up of fibres from the posterior divisions of all three trunks of the brachial plexus. |
|
|
Perform a brachial plexus block however the medial forearm is NOT numb. Which nerve has been missed?
A. Medial brachial cutanous nerve |
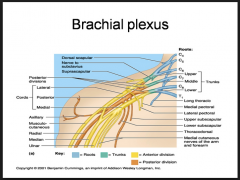
Medial cutaneous nerve of forearm actually (= median antebrachial nerve) |
|
|
Thermoneutral zone in 1 month old infant ? |
D |
|
|
Indicative of severe AS? |
C |
|
|
Risk factor for PPH? |
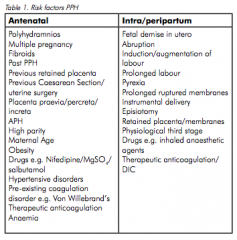
A
Ref: RANZCOG |
|
|
When stimulating the ulnar nerve with a nerve stimulator, which muscle do you see twitch?
A. opponens abducens B. abductor pollicis brevis C. adductor pollicis D. extensor pollicis E. flexor pollicis brevis |
C |
|
|
Fat:blood coefficients?
A. N2O~Des > Sevo > Iso B. N2O > Des > Sevo~Iso |
B |
|
|
18/12 old undergoing routine SV GA under LMA. Sudden onset SVT with HR 220 BP 84/60 ETCO2 32 SpO2 98.Management:
A. Adenosine 100mcg/kg B. DCR 2J/kg C. DCR 4J/kg D. Amiodarone 5mg/kg E. CPR |
A |
|
|
Clinically the most significant murmur in pregnancy is?
A. MS |
A
|
|
|
Required for diagnosis of Neuroleptic Malignant Syndrome
A. Diaphoresis B. ↑ CK C. Rigidity D. Hypertenion E. ↑ HR |
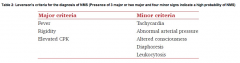
C |
|
|
2 yo 15kg child following seizure on surgical ward. Admitted with appendicitis and perforation. 60ml/hr of ½ N. Saline 5%dextrose |
C
Symptomatic hyponatraemia - treat with hypertonic saline. |
|
|
32 y/o male. Weakness distal and prox muscles, infection 10 days ago, no sensory involvement, temp 37.8, facial weakness. Cause: |
A |
|
|
70 y/o postop in recovery following hip surgery. Develops severe chest pain, ST elevation. Immediate mx: |
B |
|
|
Circuit disconnection during spontaneous breathing anaesthesia |
D
|
|
|
A 23 year old man takes his buprenorphine patch off prior to surgery. When can you expect the plasma level to be half?
a. 6 hours b. 12 hours c. 24 hours d. 36 hours e. 48 hours |
B |
|
|
How do you calculate the inspiratory time constant for lungs
A. resistance multiplied by compliance B. resistance divided by compliance C. compliance divided by resistance D. resistance minus compliance E. resistance plus compliance |
A
|
|
|
In a neonate the main resistance in a circle system with CO2 absorber
A. APL valve B. expiratory and inspiratory unidirectional valves C. tubing D. ETT E. HME filter |
D
|
|
|
Iron deficiency anaemia:
A. Low ferritin, low serum iron B. Low ferritin, low TIBC C. Elevated ferritin, low marrow iron D. Elevated ferritin, ? E. Elevated ferritin, ? |
A
|
|
|
Long-standing T6 paraplegia. Which is INCORRECT?
A. Flaccid paralysis B. Poikilothermia C. Labile BP |
A
|
|
|
You see a patient in the pre-op clinic. He is on propranolol for treatment of long QT syndrome. Which of the following will give the best reassurance that his treatment is effective? |
B |
|
|
Lap chole on citalopram. What is NOT relatively contraindicated? |
B |
|
|
Most effective treatment for post-sevoflurane agitation following grommets in a 4yo child?
A. 1 mg/kg propofol B. 1 mcg/kg fentanyl C. 1 mcg/kg clonidine D. ?dose midazolam E. Sucrose |
B
Reference from paeds textbook (coats,) says opioids are most effective |
|
|
What is NOT useful in the treatment of Torsades?
A. Isoprenaline B. Procainamide C. DCCV D. Electrical pacing (Amiodarone was not an option) |
B
Procainamide prolongs the QT interval |
|
|
Incidence of fat embolism following closed femoral fracture?
A. 0 -3% B. 4 – 7% C. 8 -11% D. 12 – 15% E. 16 - 19% |
A
Fat Embolism - CEACCP 2007 |
|
|
Middle-aged male with severe MS having general anaesthesia for repair of fractured ulna / radius. 10 minutes into the case you notice a tachyarrythmia with his HR 130 and BP 70. He is normally in sinus. What do you do?
A. Adenosine B.Amiodarone C. Shock D. Volume E. Metaraminol |
C
|
|
|
Little space between epiglottis and posterior pharyngeal wall. Modified C&L classification?
|
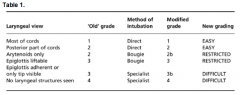
IIIa |
|
|
involving: Numb tongue and impaired taste sensation post LMA anaesthesia. |
C |
|
|
Lateral approach to popliteal block. |
B & E (Preferably tibial stimulation observe as it is more medial) |
|
|
Factors associated with post-operative ulnar nerve palsy |
C |
|
|
In a rotameter the
A. bobbin spins inside a tube that has parallel sides B. flow is laminar at high flow rates C. height of the bobbin is proportional to the pressure drop across the bobbin D. pressure drop across the bobbin is constant at varying flows E. resistance increases with increasing gas flow |
D |
|
|
Appropriate postoperative maintenance fluid in a child [can't recall situation, but something to do with head injury]:
A. 3% and 1/3 NS B. 1/2 NS C. Normal Saline D. Hartmanns E. Hartmanns with glucose |
C
|
|
|
Young woman with subarachnoid haemorrhage, hyponatraemia and increased urinary sodium (did not specify if high sodium concentration or total amount lost). What is likely cause? |
B |
|
|
Regarding mixed venous blood oxygen saturation, which statement is correct?
a. it is collected from the right atrium b. it is used to calculate cardiac output c. it can be used to accurately measure the mixed venous pO2 d. it has no impact on the A-a gradient e. it is usually 40% |
B |
|
|
Cerebral oximetry measures?
A. Arterial saturation B. Mostly arterial saturation and some venous saturation C. Capillary saturation D. Mostly venous saturation and some arterial saturation E. Venous saturation |
D |
|
|
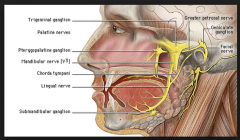
Ciliary ganglion
A sympathetic from inferior cervical ganglion B located inferiorly within orbit C may be damaged during a peribulbar block D preganglionic parasympathetic supply from the supra trochlear nerve E preganglionic parasympathetic originates from the Edinger Westpal nucleus |
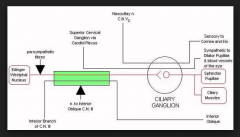
E |
|
|
Normal systolic BP at birth?
A. Something less than 70 mmHg B. 70 mmHg C. 85 mmHg D. Something more than 85 mmHg E. 115 mmHg |
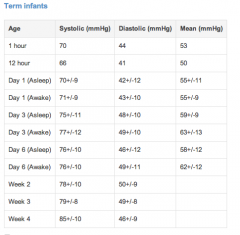
B |
|
|
Urgent reversal of INR 4.5. Intern already gave vitamin K.
A. FFP B. Prothrombinex C. Prothrombinex AND FFP |
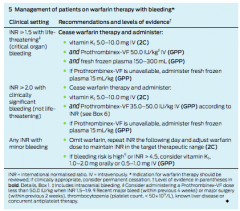
C |
|
|
Major cause of death following difficult intubation with perforated oesophagus? |
A |
|
|
Which is a specific PDE inhibitor? |
C |
|
|
Maximum dose of local infiltration of 0.5% bupivacaine in an x kg child?
A. dose corresponding to 2.5 mg/kg; there was no option corresponding to 2 mg/kg |
A |
|
|
Loading dose of IV paracetamol in x kg child?
A. dose corresponding to 20 mg/kg |
A
|
|
|
Performing a caudal block in a child. What is the first sign of a total spinal anaesthetic?
|
hypotension and bradycardia are rare
desaturation usually first signs |
|
|
Performing a caudal block in a child and add clonidine to prolong duration of block. What significant complication is increased?
A. Sedation B. Urinary retention |
A
|
|
|
New onset AF. For what period of time is it safe to perform DCCV without prior TOE to exclude thrombus?
A. <24 hours B. <48 hours |
B |
|
|
Regarding remifintanil, which is incorrect?
a. high potency b. metabolised by pseudocholinesterase c. muscle rigidity in high doses d. weakly active metabolite e. short context sensitive half time |
B |
|
|
Off-label use of a drug refers to all of the following EXCEPT: |
C
Off-label use of medicines: consensus recommendations for evaluating appropriateness. MJA 2006; 185 (10): 544-548 |
|
|
Labour epidurals increase maternal and foetal temperature. This results in neonatal
A. Increased sepsis B. Increased investigations for sepsis C. increased non shivering thermogenesis D. Increased need for resuscitation E. Cerebral palsy |
B
|
|
|
ASA grading was introduced to
A. predict intraop anaesthetic risk B. Predict intraop surgical and anaesthetic risk C. Standardise the physical status classification of patients D. Predict periop anaesthetic risk E. Predict periop anaesthetic and surgical risk |
C
|
|
|
Compared to lignocaine, bupivacaine is |
C |
|
|
Best agent to decrease both gastric volume and gastric acidity?
A. Omeprazole B. Ranitidine C. Metoclopramide D. Cisapride E. Na citrate |
B
|
|
|
Young female having cholecystectomy. Venous air embolus: |
B |
|
|
Diastolic dysfunction is NOT caused by:
A Adrenaline B Aortic stenosis C Hypertension D myocardial fibrosis E ? |
A
Also increases lusitropy (active relaxation) |
|
|
Amniotic fluid embolism. Cause of death in first half hour ?
A. Pulmonary hypertension B. Malignant arrhythmia C. Pulmonary oedema D. Hypovolaemic shock E. |
A |
|
|
Nerve block for anaesthesia over anterior 2/3 of ear? |
B
Auriculotemporal Nerve supplies anterior 2/3 Branch of the Mandibular Nerve |
|
|
Central anticholinergic syndrome, which is NOT true:
A. Will improve with neostigmine B. Peripheral anticholinergic symptoms C. Caused by Anti-Parkinson drugs D. CNS depression E. Associated with agitation, delirium, and ??? |
A |
|
|
In an acute malignant hyperthermia episode |
E
|

