![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
127 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Name 2 antibiotics that work by blocking Peptidoglycan synthesis |
Bacitracin Vancomycin name |
|
|
|
Name the drug that is a monobactam |
Aztreonam |
|
|
|
Which antibiotics belong to the carbapenem group |
Imipenem Doeipenem Ertapenem Meropenem |
|
|
|
Name 2 anti pseudomonal antibiotics that interfere with Peptidoglycan cross linking |
Ticarcillin Piperacillin |
|
|
|
Name the antibiotic that inhibits Peptidoglycan cross linking and are penicillinase resistant |
Oxacillin Nafcillin Dicloxacillin |
|
|
|
Name 3 classes of antibiotics that work by binding to the bacterial 30s ribosomal subunit |
Aminoglycosides Glycylcyline Tetracycline |
|
|
|
Name 5 antibiotics that work by binding to the bacterial 50s ribosomal subunits and blocking protein synthesis |
Chloramphenicol Clindamycin Linezolid Quinupristin Dalfopristin (streptogramins) Azithromycin Clarithromycin Erythromycin (macrolide) |
|
|
|
Which process does rifampin block to exert antimicrobial effects |
Inhibit synthesis of bacterial messenger RNA via inhibiting RNA polymerase |
|
|
|
Through inhibition of which enzyme do fluroquinolones and quinolones exert their antibacterial effects |
DNA guarded inhibition |
|
|
|
Which process do Sulfonamides and Trimethoprim effect to exert their antibacterial effects |
Folic acid synthesis and reduction (DNA methylation) Sulfonamides inhibit conversion of PABA to dihydrofolate TMP inhibit conversion of DHF to tetrahydrofolate |
|
|
|
What is the mechanism of action of metrinidazole for its antimicrobial effect |
Free radical induced damage to DNA integrity |
|
|
|
Which 2 antimicrobial act by disrupting membrane integrity |
Daptomycin Polymyxin |
|
|
|
Name the antibiotic that inhibit Peptidoglycan cross linking and are penicillinase sensitive |
Penicillin G and V Amoxicillin |
|
|
|
Which component of the cell wall is targeted by antibiotics acting at the level of the cell wall |
Peptidoglycans |
|
|
|
Penicillin G and V |
1- Penicillin G (IV and IM form), Penicillin V (oral form) 2- 1- D-ala D- ala structural analog 2- Bind to penicillin binding protein (transpeptidase) 3- Block transpeptidase cross linkage of Peptidoglycan in cell wall 4- Activate autolytic enzyme 3- 1- Gram positive bacteria 2- Gram negative bacteria (N. Meningitidis) 3- spirochete 4- Bacteriacidal (beta lactamase sensitive) 4- 1- Hypersensitivity reaction 2- Direct Coombs positive hemolytic anemia 3- Drug induced interstitial nephritis 5- 1- Beta lactamase cleave Beta lactam ring 2- Mutation of PBPs |
|
|
|
Penicillinase sensitive penicillin |
1- Amoxicillin, ampicillin, akinopenicillin 2- 1- Same as penicillin 2- Wide spectrum 3- Combined with clavulanic acid to protect against destruction by beta lactamase 4- Amoxicillin have better oral bioavailability than ampicillin 3- Extended spectrum- H. Influenza, E. Coli, L. Monocytogenes, Proteus, Salmonella, shegilla, enterococcus 4- 1- Hypersensitivity 2- Rash 3- Pseudomembranous colitis 5- Penicillinase (a type of beta lactamase) thy cleave beta lactam ring |
|
|
|
Penicillinase resistant penicillin |
1- Dicloxacillin, nafcillin, oxacillin 2- 1- Same as penicillin 2- Narrow spectrum 3- Penicillinase resistant because of bulky R group that block access of beta lactamase to beta lactam ring 3- S. Aureus (except MRSA) 4- 1- Hypersensitivity 2- Drug induce intestinal nephritis 5- MRSA has altered penicillin binding protein target site |
|
|
|
Anti pseudomonal penicillin |
1- Piperacillin, ticarcillin 2- 1- Same as penicillin 2- Extended spectrum 3- Penicillinase sensitive use of beta lactamase inhibitor 3- Pseudomonas spp. and gram negative rod 4- Hypersensitivity reaction |
|
|
|
To overcome bacterial resistance, what drug must be administered with extended-spectrum Beta- lactam (eg Piperacillin) for pseudomonal infection |
Beta lactamase inhibitor because of sensitivity of pseudomonas spp to penicillin |
|
|
|
Cephalosporin |
1- Beta lacatam drug that inhibits cell wall synthesis but is less susceptible to penicillinase 2- 1st generation (cefazolin, cephalexin)- gram positive bacterial and PEcK gram negative 3- 2nd generation (cefaclor, cefoxitin, cefuroxime, cefotetan) gram positive bacteria and HENS PEcK gram negative 4- 3rd generation (ceftriaxone, cefotaxime, cefpodoxime, ceftazidime) gram negative bacteria 5- 4th generation (cefepime)- gram negative bacteria and pseudomonas 6- 5th generation (ceftaroline) gram negative, MESA , enterococcus does not cover pseudomonas |
|
|
|
Bacterial killed by cephalosporin |
1- Listeria, atypical (chlamydia and mycoplasma), MRSA , enterococcus not covered by 1st-4th generation 2- 1st generation 1- Proteus 2- E. Coli 3- Klebsiella (PEcK) 3- 2nd generation 1- H. Influenza 2- Enterobacter 3- Neisseria spp 4- Serratia 5- PEcK |
|
|
|
Adverse effects of cephalosporin |
1- Hypersensitivity reaction 2- Autoimmune hemolytic anemia 3- Disulfiram like reaction 4- Vitamin K deficiency 5- low rate of cross reactivity seen in penicillin allergic patient 6- Increase Nephrotoxicity of Aminoglycosides |
|
|
|
Mechanism of resistance of cephalosporin |
1- Cephalosporinase (type of beta lactamase) 2- Structural change of penicillin binding protein |
|
|
|
Which drug is effective in treatment of both disseminated Lyme disease and gonorrhea |
Ceftriaxone |
|
|
|
What antibiotic is most commonly used preoperativly to protect against staphylococcus aureus wound infection |
Cefazolin |
|
|
|
Beta lactamase inhibitor |
1- Include 1- Clavulanic acid 2- Avibactam 3- Sulbactam 4- Tazabactam 2- Added to penicillin antibiotics to protect against destruction from beta lactamase |
|
|
|
Name 4 combinations of penicillin antibiotics with beta lactamase inhibitors commonly used to treat bacterial infection |
1- Amoxicillin- clavulanate 2- Ceftazidime- Avibactam 3- Ampicillin- sulbactam 4- Piperacillin- tazobactam |
|
|
|
Carbapenems |
1- Doripenem, Imipenem, Meropenem, Ertapenem DIME (use when all other antibiotics fail and life threatening infection) 2- Imipenem is a broad spectrum beta lactamase resistant carbapenem used with cislastatin( inhibitor of renal dehydropeptidase I) to decrease inactivation of drug at renal tubule 3- Use gram positive and negative bacteria and anaerobes 4- Adverse effect 1- GI distress 2- Rash 3- CNS toxicity (seizure) with high dose 5- Mechanism of resistance- inactivated by Carbapenemase produced by E. Coli, Enterobacter and K. Pneumonia |
|
|
|
Which of the carbapenem antibiotics has a lower risk of seizures |
Meropenem |
|
|
|
Which carbapenem has limited pseudomonas coverage |
Ertapenem |
|
|
|
Which carbapenem is not affected by renal dehydropeptidase I |
1- Meropenem |
|
|
|
Monobactam |
1- Aztreonam 2- Mecahnism 1- Less susceptible to beta lactamases 2- Prevent Peptidoglycan cross linkages by binding to penicillin binding protein 3 3- Synergistic with Aminoglycosides 4- No cross allergicity with penicillin 3- Use - gram negative rods and patients with penicillin allergies or renal insufficiency who cannot tolerate Aminoglycosides 4- Adverse effect 1- Occasional GI upset |
|
|
|
Vancomycin |
1- Mechanism 1- Inhibit Peptidoglycan cell wall formation by binding to D-ALA-D-ALA of cell wall precursor 2- Not susceptible to beta lactamase 3- Bacteriocidial to most bacteria 4- Bateriostatic to C. Difficle 2- Use 1- Gram positive bacteria 2- MRSA 3- S. Epidermidis 4- Enterococus 5- Clostridium difficle |
|
|
|
Adverse effect of vancomycin |
1- Nephrotoxicity 2- Ototoxicity 3- Thrombophlebitis 4- Diffuse flushing (redman syndrome) 5- DRESS syndrome |
|
|
|
Adverse effect of vancomycin |
1- Nephrotoxicity 2- Ototoxicity 3- Thrombophlebitis 4- Diffuse flushing (redman syndrome) 5- DRESS syndrome |
|
|
|
Mechanism of resistance for vancomycin |
Occurs in bacteria eg enterococcus via amino acid modification of D-ALA D-ALA to D-ALA D-Lac |
|
|
|
Protein synthesis inhibitors |
1- Target smaller bacterial ribosomes (70s, 30s and 50s subunits) 2- Leave 80s human ribosome unaffected 3- Bacteriatatic except 1- Aminoglycosides (bactericidal) 2- Linezolid (variable) 4- 30s subunit 1- Aminoglycoside 2- Tetracycline 5- 50s subunit 1- Chloramphenicol 2- Clindamycin 3- Erythromycin (macrolide) 4- Linezolid
|
|
|
|
Aminoglycosides |
1- Gentamicin, Neomycine, Amikacin, Tobramycin and streptomycin 2- Mechanism 1- Bactericidal 2- Irreversible inhibit the initiation complex by binding to 30s subunit 3- Can cause misreading of mRNA and block translocation 4- Required O2 fro uptake 2- Use 1- Gram negative bacteria 2- Synergistic with beta lactam antibiotic 3- Neomycin use for bowel surgery |
|
|
|
Adverse effect of aminoglycoside |
1- Nephrotoxicity (especially with loop diuretic) 2- Ototoxicity 3- Teratogenic 4- Neuromuscular blockage (contraindicated in myasthenia gravis) |
|
|
|
Adverse effect of aminoglycoside |
1- Nephrotoxicity (especially with loop diuretic) 2- Ototoxicity 3- Teratogenic 4- Neuromuscular blockage (contraindicated in myasthenia gravis) |
|
|
|
Mechanism of resistance of aminoglycoside |
Bacterial transferase enzymes inactive drugs by acetylation phosphorylation or adenylation |
|
|
|
Can aminoglycoside kill anaerobic bacteria |
No they require oxygen for uptake |
|
|
|
Tetracycline |
1- Tetracycline, doxycycline and minocycline 2- Mechanism 1- Bacteristatic 2- Bind to 30s subunit and prevent attachment of amino acetyl-tRNA 3- Do not take with milk (Ca) antacid (Ca and Mg) or iron containing preparation because divalent cations inhibit drug absorption in the gut 4- Limited CNS penetration 2- Uses 1- Borrelia burdorferi 2- Mycoplasma pneumonia 3- Rickettsia (accumulate Intracellularly) 4- Chlamydia 5- Doxycycline use to treat acne and community acquired MRSA, Excreted Fecal and used in patients with renal failure |
|
|
|
Adverse effect of tetracycline |
1- GI distress 2- Teeth discoloration 3- Inhibits growth in children 4- Photosensitivity 5- Contraindicated in pregnancy |
|
|
|
Adverse effect of tetracycline |
1- GI distress 2- Teeth discoloration 3- Inhibits growth in children 4- Photosensitivity 5- Contraindicated in pregnancy |
|
|
|
Mechanism of resistance of tetracycline |
Decrease uptake or increase efflux out of bacterial cell by plasmid encoded transport pump |
|
|
|
Tigecycline |
1- Tetracycline derivative 2- Use 1- Broad spectrum (anaerobes, gram positive and gram negative) 2- MRSA 3- Infection requiring deep tissue penetration 3- Adverse effect 1- nausea and vomiting |
|
|
|
Chloramphenicol |
1- Block peptidyltransferase at 50s ribosomal subunit bactericidal 2- Use 1- Meningitis 2- Rickettsia 3- Adverse effect 1- Microcytic anemia 2- Aplastic anemia 3- Grey baby syndrome ( premature infants due to lack of liver UDP glucoronosyltransferase) 4- Mechanism of resistance - Plasmid encoded acetyltransferase inactivates the drug |
|
|
|
Clindamycin |
1- Block peptide transfer translocation at 50s ribosomal subunit Bacteriastatic 2- Use 1- Anaerobic bacteria in aspiration pneumonia, lung abscess and oral infection (anaerobes above diaphragm) 2- Invasive group A streptococcus infection 3- Adverse effect 1- Fever 2- Diarrhea 3- Pseudomembranous colitis (overgrowth of C. Difficile) |
|
|
|
Macrolides |
1- Azithromycin, Clarithromycin and Erythromycin 2- Block translocation at 50s ribosomal subunit. Bind to 23S rRNA of 50s ribosomal subunit. Bacteriostatic 3- Use 1- Atypical pneumonia (mycoplasma, chlamydia and legionella) 2- STI (chlamydia) 3- Gram positive cocci (streptococcus infection in patients allergic to penicillin) 4- B. Pertussis 4- Mechanism of resistance- Methylation of 23SrRNA binding site preventing binding of drug |
|
|
|
Adverse effect of macrolides |
1- GI motility issues 2- Arrhythmia caused by prolonged QT interval 3- Cholestatic hepatitis 4- Rash 5- Eosinophilia 6- Increase serum concentration of thiophyllin and oral anticoagulants 7- Clarithromycin and erythromycin inhibits Cytochrome p450 |
|
|
|
Linezolid |
1- Prevent formation of initiation complex by binding to 50s ribosomal subunit 2- Use 1- gram positive bacteria 2- MRSA 3- VRE 3- Adverse effect 1- Bone marrow suppression (especially thrombocytopenia) 2- Peripheral neuropathy 3- Serotonin syndrome (due to partial MAO inhibition) 4- Mechanism of resistance- Point mutation of ribosomal RNA |
|
|
|
Polymyxins |
1- Colistin (polymyxin E), polymyxin B 2- Mechanism 1- Cation polypeptide that binds to phospholipid on cell membrane of gram negative bacteria 2- Disrupt cell membrane integrity — Leakage of cellular component— cell death 3- Use- 1- Salvage therapy for multi drug resistant gram negative bacteria (E. Coli, K. Pneumonia and pseudomonas) 2- Polymyxin B is a component in a triple antibiotic use to treat superficial skin infections 4- Adverse reaction- 1- Nephrotoxicity 2- Neurotoxicity (slurred speech, weakness and paresthesia) 3- Respiratory failure 4- Contact dermatitis |
|
|
|
Sulfonamide |
1- Sulfamethoxazole (SMX), sulfisoxazole, sulfadiazine 2- Mechanism 1- Inhibit dihydropterate synthase this inhibiting folate synthesis (Bacteristatic (Bactericidal when combined with trimethaprim) 3- Use 1- Gram positive 2- Gram negative 3- Nocordia 4- Simple UTI 4- Mechanism of resistance - Altered enzyme (dihydroorotate synthase) decrease uptake and.increase PABA synthesis |
|
|
|
Adverse effect of Sulfonamide |
1- Hypersensitivity reaction 2- Hemolytic anemia in G6PD deficiency 3- Nephrotoxicity ( tubulointerstitial nephritis) 4- Photosensitivity 5- Steven Johnson syndrome 6- Kernicterus in children 7- Displace drugs from albumin eg warfarin |
|
|
|
Dapsone |
1- Mechanism 1- Imhibit dihydroorotate synthase thus inhibiting folate synthesis 2- Use- 1- Leprosy 2- Pneumocystis jirovecii prophylaxis and treatment with combination of TMP 3- Adverse effect 1- Agranulocytosis 2- Methhemoglobinemia 3- Hemolytic anemia in G6PD deficiency |
|
|
|
Trimethoprim |
1- Inhibit dihydrofolate reductase, Bacteriostatic 2- Use 1- UTI 2- Shigella 3- Salmonella 4- Pneumocystis jirovecii treatment and prophylaxis 5- Toxoplasmosis prophylaxis 6- Use in combination with Sulfonamide 3- Adverse effects 1- Hyperkalemia 2- Megaloblastic anemia 3- Leukopenia 4- Granulocytopenia (avoid with combination of leucivorin (folinic acid) |
|
|
|
Fluroquinolones |
1- Ciprofloxacin, enoxacin, norfloxacin ofloxacin respiration fluroquinolones - levofloxacin, genifloxacin, moxifloxavin 2- Mechanism 1- Inhibit prokaryotes topoisomerase 2 (DNA gyrase) and topoisomerase 4 2- Bactericidal 3- Not to be taken with antacid 3- Use 1- Gram negative Urinary, respiratory and GI tract infection (pseudomonas) 2- Gram positive neisseria 3- Otitis externa 4- mechanism of resistance 1- Chromosome encoded mutation in DNA gyrase 2- Plasmid mediated resistance 3- Efflux pump |
|
|
|
Adverse effect of fluroquinolones |
1- GI upset 2- Superinfection 3- Skin rash 4- Headache 5- Dizziness 6- Contraindicated in pregnancy, nursing mothers and children <18 due to possibility of damage to cartilage 7- Prolonged QT interval 8- Tendonitis or Tendon rupture in patients >60 years old or patients taking prednisone 9- Ciprofloxacin inhibit cytochrome P450 |
|
|
|
Daptomycin |
1- Lipopeptide that disrupt cell membranes of gram positive cocci by creating transmembrane channels 2- Use 1- S. Aureus (especially MRSA) 2- VRE 3- Bacteremia 4- Endocarditis 3- Adverse effects 1- Myopathy 2- Rhabdomylitis 3- Not used for pneumonia ( avidly bind to and is inactivated by surfactant) |
|
|
|
Metronidazole |
1- Form toxic free radical metabolites in bacterial cell that damage DNA, Bacteriacidal and anyiprotozoal 2- Use 1- Giardia 2- Entamoeba 3- Trichamonas 4- Gardenella vaginalis 5- Anaerobes 6- H. Pylori replaces amoxicillin in triple therapy 3- Adverse reaction 1- Disulfiram like reaction ( severe flushing, tachycardia, hypotension) with alcohol use 2- Headache 3- Metallic taste |
|
|
|
Antimicrobial therapy for M. Tuberculosis, M. avium and M. Leprosy |
1- M. Tuberculosis 1- Prophylaxis- Isoniazid 2- Treatment 1- Rifampin 2- Isoniazid 3- Pyrazinamide 4- Ethambutal (RIPE) 2- M. avium-Intracellular 1-Prophylaxis- Azithromycin and rifabutin 2- Treatment 1- Azithromycin or Clarithromycin and ethambutal 3- M. Leprosy Treatment 1- Dapson and Rifampin - tuberculoid form Add clofazime for lepromatous
|
|
|
|
Rifamycin |
1- Rifampin, Rifabutin 2- Mechanism - Inhibit DNA dependent RNA polymerase 3 Use- 1- Mycobacteria tuberculosis 2- Leprosy 3- Meningococcal prophylaxis and chemoprophylaxis in contacts of children with H. Influenza 4- Adverse effect 1- Heptatotoxic ( increase cytochrome p450) 2- Red/orange urine 3- Rifabutin use in HIV due to less cytochrome P450 5- Mechanism of resistance 1- Mutation reduce binding to RNA polymerase 2- Monotherapy rapidly leads to resistance |
|
|
|
What is the benefit of utilizing Rifampin in the treatment of mycobacterium leprae |
It delays resistance to dapsone |
|
|
|
4 Rs of Rifampin |
RNA polymerase Ramps up cytochrome P450 Red/orange body fluid Rapid resistance when used alone |
|
|
|
Isoniazid |
1- Decrease synthesis of mycolic acid. Bacterial catalase-peroxidase (encoded by KatG) is needed to convert INH to its active metabolite 2- Use - Mycobacterium tuberculosis 3-Adverse effect 1- Hepatotoxicity 2- Anion gap metabolic acidosis 3- Vitamin B6 deficiency (peripheral neuropathy, sideriblastic anemia) administered with pyridoxine B6 4- Cytochrome P450 inhibition 5- Drug induced lupus 6- Seizure (high dose, refractory to benzodiazepines 4- Mechanism of resistance- Mutation leads to under-expression of katG |
|
|
|
Why do patients require different dosages of isoniazid |
People are either fast or slow acetylators and half life of isoniazid differed dependen on rate of acetylation |
|
|
|
Pyrazinamide |
1- Mechanism unknown. Prodrug that is converted to its active compound pyrizonic acid. Works best at acidic pH 2- Use- Mycobacterium tuberculosis 3- Adverse effect 1- Hepatotoxicity 2- Hyperurecemia |
|
|
|
Ethambutol |
1- Decrease carbohydrate polymerization by blocking arabinosyltransferase 2- Use - mycobacterium tuberculosis 3- Adverse effect 1-Optic neuropathy (red- green color blindness, reversible) 2- Peripheral neuropathy 3- Arthralgia |
|
|
|
Streptomycin |
1- Inhibit protein synthesis by binding to 30s ribosomal subunit 2- Use - 2nd Lind for mycobacterium tuberculosis 3- Adverse effects 1- ataxia 2- Tinnitus 3- Vertigo 4- Nephrotoxicity |
|
|
|
Antibiotic against exposure to meningococcal infection |
Ceftriaxone Ciprofloxacin Rifampin |
|
|
|
Antibiotics against endocarditis, dental procedure |
Amoxicillin |
|
|
|
Antibiotics against recurrent UTI |
TMP-SMX |
|
|
|
Malaria prophylaxis for travelers |
1- Atovaquone- proguanil, 2- mefloquine 3- doxycycline 4- Primaquine 5- Chloroquine |
|
|
|
Antibiotic for pregnant woman carrying group B strep |
1- Penicillin G 2- Ampicillin |
|
|
|
Prevention of gonococcal conjuctivitis in newborn |
1- Erythromycin ointment in eye |
|
|
|
Prevention of post surgical infection due to S. Aureus |
Cefazolin |
|
|
|
Prophylaxis of strep pharyngitis in child with prior rheumatic fever |
1- Benzathine penicillin G 2- Oral penicillin V |
|
|
|
Prophylaxis given to HIV patients with CD4 count <200 |
1- TMX-SMX 2- Pneumocystis jirovecii |
|
|
|
Prophylaxis given to HIV patients with CD4 count <200 |
1- TMX-SMX 2- Pneumocystis jirovecii |
|
|
|
Prophylaxis in HIV patients with CD 4 count <100 |
1- TMP-SMX 2- Pneumocystis jirovecii and toxoplasmosis |
|
|
|
Prophylaxis for HIV patients with CD 4 count <50 |
1- Azithromycin or Clarithromycin 2- Mycobacterium avium complex |
|
|
|
Antibiotics for MRSA |
1- Daptomycin 2- Doxycycline 3- Ceftaroline 4- Vancomycin 5- Tigecyclin 6- Linezolid |
|
|
|
Antibiotics for VRE |
1- Streptogramins (quinupristin, dalfopritin) 2- Tigecyclin 3- Linezolid |
|
|
|
Antibiotics for multi drug resistant pseudomonas and acinabacter baumani |
Polymyxin E (colistin) and Polymyxin B |
|
|
|
Amphotericin B |
1- Bind to ergosterol. Form membrane pores that allows leakage of electrolytes 2- Use 1- Systemic fungus 2- Cryptocococcus 3- Candida 4- Mucor 3- Adverse effect 1- Anemia 2- Arrhythmia 3- Hypotension 4- Fever/ chills 5- IV phlebitis 6- Nephrotoxicity (hydration decrease toxic) 7- Supplementation with K and Mg due to altered renal tubular Permeability 4- Decrease toxicity- liposomal amphotericin |
|
|
|
What second agent can be administered with amphotericin B to treat cryptococcal meningitis |
Flucytosine |
|
|
|
Nystatin |
1- Bind to ergosterol. Form membrane pores that allow leakage of electrolytes (same as amphotericin B) 2- Use topical only as it is too toxic for systemic use 2- Use 1- Oral Candida 2- Diaper rash 3- Vaginal candidiasis |
|
|
|
Flucytosine |
1- Inhibit DNA and RNA biosynthesis by conversion to 5- Flouorouracil by cytidine deaminas 2- Use- systemic fungi (especially meningitis) 3- Adverse effect- Bone marrow suppression |
|
|
|
Azole |
1- Fluconazole, cotrimazole, isovuonazole, itraconazole ketaconazole, miconazole, variconazole 2- Inhibit ergosterol by inhibiting cytochrome P450 enzyme (14 alpha demthylase) that converts lansosterol to ergosterol 3- Use 1- systemic fungi 2- Fluconazole ( cryptococcus and Candida) 4- Adverse effect 1- Testosterone synthesis inhibitor (gynocomastia ketoconazole) 2- Liver dysfunction (inhibit cytochrome P450h |
|
|
|
Isavuconazole is indicated for which 2 fungal infection |
Mucar Aspergillus |
|
|
|
Terbinafine |
1- Inhibit fungal enzyme squalene epoxidase 2- Use- Dermatiphytes (especially onychomycosis) 3- Adverse effect 1- GI upset 2- Headache 3- Hepatotoxicity 4- Taste disturbance |
|
|
|
Echinocandins |
1- Antidulafungin, caspofungin, micafungin 2- Inhibit cell wall synthesis by inhibiting the synthesis of beta glucan 3- Use- 1- Invasive Aspergillus 2- Candida 4- Adverse effect 1- GI upset 2- Flushing (by histamine release) |
|
|
|
Griseofulvin |
1- Interferes with microtubles function, disrupts mitosis. Did posits in karatin containing tissues (eg nail) 2- Use 1- Oral antifungal for superficial infection 2- Inhibit the growth of dermatophytes 3- Adverse effect 1- Carcinogenic 2- Confusion 3- Increase cytochrome P450 4- Disulfiram like reaction 5- Teratogenic 6- Headache 7- Increase warfarin metabolism |
|
|
|
Antiprotozoal therapy |
1- Pyrimethamin - Toxoplasmosis 2- Suramin and melarssoprol - Trypanosoma brucei 3- Nifurimox - Trypanosoma cruzi 4- Sodeium stibogluconate - pediculus and Pthisus |
|
|
|
Anti- mite/louse therapy |
1- Permethrin- Inhibit Na channel deactivation— neuronal membrane depolarization 2- Malathion- ACH esterase inhibitor 3- Topical or oral ivermectin- Cl influx 4- Lindane - Blocks GABA channels 5- Treat scales and lice |
|
|
|
Cholroquine |
1- Blocks detoxification of Heme into hemozoin Heme accumulate and is toxic to plasmodia 2- Use- Plasmodia species except P. Falciparum 3- Adverse effect 1- Retinopathy 2- Pruritus |
|
|
|
P. Falciparum mechanism of resistance |
Due to membrane pump decrease Intracellular concentration of drug |
|
|
|
Anti helmets therapy |
1- Pyrantel 2- Ivermectin 3- Mebendazole (Microtubles inhibitor) 4- Praziqunatal (Incrase Ca permeability, Increase vaculization) 5- Duethylcarbamazin |
|
|
|
Oseltamivir Zanamivir |
1- Inhibit influenza neuroaminidase, decrease release of progeny virus 2- Use 1- Treat and prevent influenza type A and B 2- Begin therapy within 48hrs of symptoms |
|
|
|
Acyclovir, Famciclovir, Valocyclovir |
1- 1- Guanosine analogue 2- Monophosphorylaed by HSV/VZV thymidine kinase 3- Triphosphate form by cellular enzymes 4- Inhibit viral DNA polymerase by chain termination 2- Use 1- HSV 2- VZV 3- Weak activity against EBV 4- Valciclovir have better oral bioavailability 5- Famciclovir for herpes zoster 3- Adverse effect 1- Obstructive crystalline nephrophaty 2- Acute kidney injury if not properly hydrated 4- Mechanism of resistance 1- Mutated viral thymidine kinase |
|
|
|
Acyclovir and valacyclovir are not useful against which 2 viruses |
Weak activity against EBV CMV |
|
|
|
Ganciclovir |
1- 1- Guanosine analog 2- 5’ Monophosphate formed by a CMV viral kinase 3- Triphosphate formed by cellular kinase 4- Inhibit viral DNA polymerase 2- Use 1- CMV 2- Valganciclovir better oral bioavailability 3- Adverse effect- 1- Bone marrow suppression 2- Renal toxicity 4- Mechanism of resistance 1- Mutated viral kinase |
|
|
|
Foscarnet |
1- 1- Inhibit viral DNA/RNA polymerase 2- Inhibit HIV reverse transcriptase 3- Bind to the phosphate binding site of enzymes 4- Does not required kinase activity 2- Use- 1- CMV retinitis in immunosuppressed individual when Ganciclovir fails 2- Acyclovir resistant HSV 3- Adverse effect 1- Nephroptoxicity 2- Electrolyte imbalance (hypo or hypercalcemia, hypo or hyperphosphatemia, hypokalemia and hypo magnesium) 3- Lead to seizures 4- Mechanism of resistance 1- Mutated DNA polymerase |
|
|
|
Cidofovir |
1- 1- Inhibit Viral DNA polymerase 2- Does not require kinase activity 2- Use 1- CMV retinitis in immunosuppressed patients when Ganciclovir fails 2- Acyclovir resistant HSV 3- Long half life 3- Adverse effect 1- Nephrotoxicity ( coadministered with probenecid and IV saline to decrease toxicity) |
|
|
|
HIV therapy |
1- Start therapy at diagnosis 2- Use when have AIDS defining symptoms , CD4 count <500 and high viral load 3- Recommended therapy 2 NRTI and Intergrase inhibitor 4- All antiretroviral can be used for HIV 1 and 2 except NNRTI and Enfuvirtide |
|
|
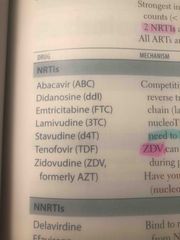
NRTI |
1- Competitive inhibitor of nucleotide by binding to reverse transcriptase- terminate DNA chain (lack 3’ OH group) 2- All or nucleosides except tenofovir which is a nucleotide. All nucleoside need to be phosphorylated to be active 3- ZDV given in pregnancy to decrease fetal transmission 4- Adverse effect 1- Bone marrow suppression 2- Peripheral neuropathy 3- Lactic acidosis 4- Anemia (ZDV) 5- Pancreatitis (didanosine) 6- Tenofovir - renal failure (fanconi syndrome) 5- Abacavir contraindicated in patients with HLA-B 507 mutation due to increase risk of hypersensitivity |
|
|
|
NNRT Delavirdine Efavirenz Nevirapine |
1- Bind to reverse transcriptase at a different site from NRTI 2- Does not require phosphorylation to be active 3- Adverse effect 1- Rash 2- Hepatotoxicity 4- Vivid dreams and CNS symptoms with efavirenz |
|
|
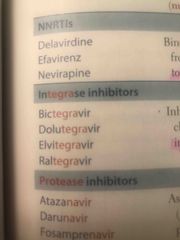
Integrase inhibitor |
1- Inhibit HIV genome integration into host cell by reversible inhibiting HIV integrase 2- Adverse effect - Increase creatine kinase |
|
|
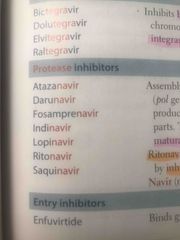
Protease inhibitor |
1- Prevent maturation of new virus 2- Ritinavir boost other drugs concentration by inhibiting cytochrome p450 3- Adverse effect 1- Hyperglycemia 2- GI intolerant 3- Lipodystrophy (Cushing like syndrome) 4- Nephropathy, hematuria, thrombocytopenia (indinavir) 5- Rifampin decrease protease inhibitor concentration use Rifabutin instead |
|
|
|
Enfuvirtide |
1- Bind to gp41 2- inhibit Viral entry |
|
|
|
Maraviroc |
1- Bind to CCR5 on T cells inhibiting interaction with go120 |
|
|
|
Pancytopenia develops in a patient being treated for HIV. Which drugs should be considered to counteract this adverse effect |
Granulocytes colony- stimulating factor (G- CSF) Erythropoietin |
|
|
|
Hepatitis C therapy |
1- NS5A inhibitor 2- NS5B inhibitor 3- NS3/4A inhibitor 4- Ribavirin |
|
|
|
NS5A inhibitor |
1- Ledipasivir, Ombitasivir and avalpatasvir 2- Inhibits NS5A, a viral phosphoproetin that plus a key role in viral RNA replication 3- Adverse effect 1- Headache 2- Diarrhea |
|
|
|
NS5B inhibitor |
1- Sofosbuvir, Dasabuvir 2- Inhibit NS5B, RNA dependent RNA polymerase that acts as a chain termination 2- Prevent viral RNA replication 3- Adverse effect 1- Headache 2- Fatigue |
|
|
|
NS3/4A inhibitor |
1- Grazoprevir, simeprevir 2- Inhibit NS3/4A , a viral protease 2- Inhibit viral replication 3- Adverse effect 1- Headache, fatigue - G 2- Photosensitivity, rash - S |
|
|
|
Ribavirin |
1- Inhibit synthesis of guanine nucleotide by competitively inhibiting IMP dehydrogenase 2- Adverse effect- 1- Hemolytic anemia 2- Teratogenic |
|
|
|
Disinfection and sterilization |
1- Autoclave 2- Alcohol 3- Chloehexidine 4- Chlorine 5- Ethylene oxide 6- Hydrogen peridoxide 7- Iodine and iodophors 8- Quaternary amines |
|
|
|
Use of Autoclave |
1- Sporicidal 2- Pressurized steam at >120’ 3- Not use for prions |
|
|
|
Alcohol and chlorhexidine use |
1- Not sporicidal 2- Denature proteins and Disrupts cell membrane |
|
|
|
Chlorine use |
1- Sporicidal 2- Oxidized and denature protein |
|
|
|
Ethylene oxide use |
1- Sporicidal 2- Alkaltating agent |
|
|
|
Hydrogen peroxide use |
1- Sporicidal 2- Free radical oxidation |
|
|
|
Iodine and iodophors use |
1- Sporicidal 2- Halogenation of DNA, RNA and protein |
|
|
|
Quaternary amines use |
1- Not Sporicidal 2- Impaired permeability of cell membrane |
|
|
|
Antimicrobial to avoid in pregnancy |
1- Sulfonamide- Kernicterus 2- Aminoglycoside- Ototoxicity 3- Fluroquinolones- Cartilage damage 4- Clarithromycin- Embryotixic 5- Tetracycline- Discolored teeth and impaired bone growth 6- Ribavirin - Teratogenic 7- Giseofulvin- Teratogenic 8- Chloramphenicol- Gray baby syndrome |
SAFe Children Take Really Goof Care |

