![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
66 Cards in this Set
- Front
- Back
|
Antibiotic |
substance produced by microorganism that kills/inhibits growth of another organism at high dilution |
|
|
Antimicrobial Agent |
chemical that kills/inhibits growth of microorganism |
|
|
Antibiotic Characteristics |
-Specific Spectrum (narrow spectrum: effective against few related bacteria) -Specific Mechanism of Action -Selective toxicity - bc of specific mechanism of action, are tolerated by host, lethal to microbes -Therapeutic Index |
|
|
Therapeutic Index |
-lowest dose toxic to pt/dose used to treat pt (larger is better) |
|
|
General Adverse Effects |
1. Allergic Rxns - ppl develop hypersensitivity to antimicrobials 2. Toxic Effects 3. Suppression of Normal Flora - GI problems & other pathogens can grow at hi numbers |
|
|
Disinfectant |
-Nonspecific mechanism of action & broadly active, not tolerated by host, need hi concentrations due to lack of specificity
|
|
|
5 major mechanisms of how ABx work |
1. Inhibit CW synthesis (most common) 2. Inhibit protein synthesis 3. Inhibit Nucleic Acid function/production 4. Disrupting Metabolic Pathways 5. Disrupting PM |
|
|
3 Mechanisms for ABx Selective Toxicity |
1. Absence of target from host (e.g. CW) 2. Permeability differences (e.g. ABx taken up by bacteria but not by our cells, so we take those ABx thru IV) 3. Structural differences in target (e.g. ribosomes are sufficiently different) |
|
|
Bacteriostatic Agents |
-Reversibly inhibit bacterial growth -Often resemble metabolite analogs & act as competitive inhibitors of normal metabolites -often target metabolic processes |
|
|
Bacteriocidal Agents |
-Kill bacteria -Generally effective only against actively growing cells, mycobacteria (cause TB) are a problem bc they grow slowly -often target cell wall/PM- may or may not cause lysis |
|
|
Susceptibility Testing |
-Goal: to determine sensitivity of infecting agent in a culture to various ABx -Minimum Inhibitory Concentration: lowest conc of AB that effectively inhibits growth of microorganism -2 techniques: 1. Tube dilution method: bacteria grown in small cultures in presence of diff AB concentrations -tells you sensitivity to diff drug conc 2. Disc Diffusion method: bacterial isolate is spread over a plate, grows cloudy 'lawn' on plate, and AB discs are placed on agar to diffuse drug into agar. -Not sensitive to AB: more cloudy area around disc -Sensitive: clear area around disc- width of clear area related to MIC |
|
|
Situations Warranting Combined Therapy |
(After Susceptibility Testing- how many drugs do you need?) 1. Chronic infections- prevent strain resistance 2. Emergency situations - not enough time for lab studies 3. Mixed Infections 4. Synergistic Effects |
|
|
Practical Examples of Synergism |
1. Bactrim: used to treat ear infections, UTI, etc -Sulfamethoxazole: inhibits NEW synthesis of THF acid, not existing pools -Trimethroprim: inhibits exsint pools of THF acid, not NEW synthesis 2. Augmentim: -Amoxicillin: beta-lactam AB -Clavulanic acid: beta-lactamase inhibitor |
|
|
Practical Examples of Antagonism |
Penicillin: disrupts growth of CW on actively growing bacteria producing CW Erythromyocin: bacteriostatic AB that inhibits protein synthesis -erythromyocin render Penicillin much less effective by slowing bacterial growth |
|
|
Drug-Drug Interactions |
Indifferent, Additive, Synergsitic, Antagonistic |
|
|
Factors Limiting Successful Antimicrobial Therapy |
1. Location -intracellular location of bacteria -blood-brain barrier/other anatomic barriers -biofilm 2. Abscess formation & necrosis -decrease circulation limits access of drug, Antibodies, & phagocytes -Limited O2 & nutrients slow bacterial growth -e.g. Necrotizing pneumonia 3. Presence of foreign bodies & obstructions -bacteria adheres to surface and forms biofilm -e.g. catheter, sutures 4. Drug Resistance |
|
|
Mechanisms of AB resistance |
1. Enzymatic inactivation/alteration of AB -beta-lactamase cleaves beta-lactam ring of penicillin 2. Inadequate/Decreased Uptake of AB -Absence of adequate transporter, mutated porin 3. Active/Increased Efflux of AB out of microbe -bacteria have multidrug efflux systems that form membrane pores |
|
|
3 Ways ABx are Used |
Empiric Therapy- given for proven/suspected infection, but organism not identified - broad spectrum ABx Definitive Therapy- for proven infection & based on causative organism Prophylaxis - given to prevent infection |
|
|
Questions to Always Ask before prescribing ABx |
1. Necessary? 2. Allergies to ABx? (e.g. penicillin) 3. Community or hospital acquired? (Later has greater resistance) 4. Is pt immunocompromised? (if so, think unusual pathogens) 5. Positive cultures? (if so, narrow-spectrum) 6. Dose, frequency, route? (depends on how sick is pt) 7. Combination? 8. How serious is infection? life-threatening? 9. Cost? meh.... |
|
|
Drugs by Mechanism of Action |
1. Penicillin, Cephalosporin, Carbapenem - beta-lactams, CW 2. Glycopeptides/Polypeptides - PM 3. Macrolides, Aminoglycosides, Tetracyclines Chloramphenicol - Protein Synthesis 4. Quinolones, Rifampin, Metronidazole - NA Synthesis 5. Suflonamide - Antimetabolites
|
|
|
Drugs that need ID approval before use at Penn |
Why need approval? Due to Side effect issues, but more so "heavy-hitters"- drugs that commonly work against drug-resistant organisms- so we don't resistance development. Ceftazidime, Meropenem, Colistin, Daptomycin Cholamphenicol Levofloxacin
|
|
|
Mechanism of Beta-Lactam ABx |
-ABx bind to transpeptidase & inhibit its function as competitive inhibitors -do not destroy exising cross-links but prevent formation of new ones -More effective against gram+
|
|
|
Penicillin |
Very effective & well tolerated -share beta-lactam ring: 4-sided ring w/ Nitrogen
|
|
|
Penicillin- 3 Classes |
1. Natural Penicillins 2. Penicillinase-resistant penicllins 3. Extended-spectrum penicillins |
|
|
Natural Pencillin |
-Primarily active against most Gram+ (poor against Staph (resistant)) -drug choice for Streptococcus, Meningococcus, susceptible Pneumococci, Syphillis -Penicillin G: inactivated by low pH so given IV -Penicillin V - acid stable, so taken PO
|
|
|
Penicillinase-resistant (aka Beta-Lactamse resistant) Penicillins |
-Resistant to beta-lactamases, so are narrow-spectrum ABx used against Staph -narrow spectrum-- used for community-acquired infections -No coverage of Gram--- Methicillin, nafcilin, oxacillin, cloxacillin, dicloxacillin
|
|
|
Extended Spectrum Penicillins |
-Coverage of many Gram-- -sensitive to beta-lactamase so used w/ beta-lactamase inhibitors -used to treat UTI, otitis media, uncomplicated community-acquired pneumonia, H. influenzae, Listeria meningitis, Lyme disease Ampicillin, Amoxicillin, Carbenicllin, Piperacillin -Amoxicillin used more than ampicillin bc can be absorbed better |
|
|
Side Effects of Penicillin |
-Overall relatively Safe, but must ask if there is a history of taking pencillin before -Hypersensitivity: ~1-10%; main side effect -Anaphylaxis: severe, rare, but what you worry about
*Nausea & vomiting: NOT allergic rxns to drug |
|
|
Beta-Lactam 3 Mechanisms of Resistance |
1. Beta-lactamase production 2. Transpeptidase mutation (prevents drug binding) 3. Gram-negatives have membrane pumps to remove drug out of periplasm
|
|
|
Beta-Lactamase Inhibitors |
-alone- weak antimicrobial activity -combined w/ penicillin to treat beta-lactamase producing bacteria
|
|
|
Methicillin |
-Beta-lactamase resistant penicillin used against Staph -If resistant to methicillin, it is resistant to all Beta-lactamase penicillins -Not commonly used at Penn -MRSA - resistant to methicillin |
|
|
Cephalosporin |
-same mechanism of action as penicillin w/ 1) Wider spectrum 2) Resistance to beta-lactamase 3) Improved pharmacokinetics -Bactericidal -beta-lactam ring -6-membered ring instead of 5-membered ring attached to beta-lactam -resistant to beta-lactamase produced by Staph & common Gram-- -do not cover enterocci -described as generations (1-4): each successive generation has better Gram+ coverage, worse Gram-- coverage |
|
|
Cephalosporin - 1st generation |
-very active against Gram+, including Staph but not MRSA, but moderate against Gram--, e.g. E coli -used for community-acquired UTI & respiratory infections -Cefazolin- famous for being used against surgical prophylaxis |
|
|
Cephalosporin- 2nd generation |
-used for Otitis media in children -increased activity against Gram--, esp H. influenzae, Resp infections, & UTIs
|
|
|
Cephalosporin- 3rd generation |
-management of hospital-acquired Gram-- bacteremia, inpatient pneumonia & UTI -unlike 1st & 2nd generation, can penetrate CNS -single-dose ceftriaxone is used for gonococcal infections (*see STD lecture) -Ceftazidime: pseudonomaz |
|
|
Side Effects of Cephalosporins |
-overall pretty safe -Hypersensitivity rxns (just like penicillin)
-GI problems bc more Gram--- coverage
-Resistance (just like PCN) |
|
|
Carbapenems |
-Same mech of PCN w/ 1) wider spectrum 2) resistance to beta-lactamases 3) improved pharmacokinetics -Bactericidal (usually given IV) -Cover virtually everything except enterococci -BROAD spectrum, powerful drugs that are rarely used (bc we wanna avoid resistance) -often used as empirical therapy for very ill pts -last resort for E. Coli & Kliebsalla infections |
|
|
ABx that disrupt PM |
-Glycopeptides - Vancomyocin -Polypeptides- Bactitracin & Polymixin |
|
|
Vancomyocin- Properties |
-glycopeptide -Interacts w/ D-alanine-D-alanine termini of pentapeptide side chains interfering w/ formation of bridges bw PG chains -inhibits CW synthesis, similar to beta-lactams, but no cross-resistance w/ these drugs -given IV bc of poor absorption from intestinal tract except for when treating GI infection |
|
|
Vancomyocin- Uses |
-Excellent Gram+ coverage -No Gram-- coverage (bc too big to pass thru porins) -Used for MRSA & other beta-lactam resistant Gram + organisms -Used for C. difficile colitis |
|
|
Vancomyoicin- Side Effects |
must be infused slowly or will cause hypersensitivity rxn -thromboephlebitis -'Red Man syndrome' - rare, more severe, w/ red rash over neck face, & trunk
|
|
|
Bactitracin |
-Polypeptides -Interferes w/ transport of PG precursors across PM -can't be taken PO bc of toxicity issues -only used topically & most effective against Gram+ |
|
|
Drugs that inhibit protein Synthesis |
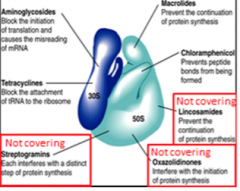
-mostly attack bacterial ribosomes *catcher makes a CLEan TAG Chloramphenical/Clindamycin, Linezolid, & Erythromyocin - (all macrolides; must remember that Erythromyocin is macrolide) bind to 50S Tetracycline & AminoGlycosides- bind to 30S
|
|
|
Macrolides- Properties |
-reversibly bind to 50S ribosome & prevents protein elongation -bacteriostatic -well-tolerated -Erythromyocin- largely replaced by Azithromycin
|
|
|
Macrolides- Uses |
-marketed as Z-pak -broad spectrum against Gram+, some Gram-
|
|
|
Aminoglycosides - Mechanism |
-Irreversibly bind 30S & causes distortion/malfunction of ribosome, blocks initiation translation, and misreading of DNA -Bactericidal bc bind irreversibly -Penetration thru PM is aerobic, energy-dependent process, so not effective against anaerobes -Not effective against enterococci & streptococci unless B-lactam drug is coadministered |
|
|
Aminoglycosides- Uses |
-Primarily against aerobic, Gram-- rods, e.g. E. Coli, and Klebsiella -not absorbed from gut, so given IV -Toxic, so reserved for serious Gram-- infections
Gentamicin & Tobramycin- most commonly used -gentamicin is co-administere dw/ beta-lactam which damages CW to help it penetrate
|
|
|
Aminoglycosides- Resistance |
-Resistance is increasing w/ Pseudonomas & Enterococci -3 Resistance Mechanisms 1) enzymatic modification of drug 2) reduced uptake/permeability 3) altered ribosome binding site |
|
|
Aminoglycosides- Side Effects |
Nephrotoxicity- associated w/ hi trough levels, reversible Ototoxicity- associated w/ hi peak levels, irreversibly can cause tinnitus & permanent deafness bc of hair cell loss |
|
|
Tetracyclins - Mechanism |
-reversibly bind 30S ribosomal subunit --> blocks attachment of tRNA to ribosome & prevents continuation of protein synthesis -bacteriostatic
|
|
|
Tetracyclin- Use |
-an 'old drug class' used for unusual agents: chlamydia, mycoplasma, & Lyme Disease -also commonly used for acne |
|
|
Tetracyclin- Side Effects |
-discolored teeth in children- DO NOT GIVE TO PREGNANT WOMEN or CHILDREN -GI upset -Phototoxic dermatitis |
|
|
Chloramphenicol- Mechanism |
-Binds to 50S ribosomal subunit - & prevents peptide bonds from forming & blocking protein synthesis |
|
|
Chloramphenicol- Uses |
Very wide variety of organisms -bc of rare/deadly side effects, it is used as last resort for life-threatening infection
-Widely used in developed countries bc of broad spectrum & very low cost
|
|
|
Chloramphenicol- Side Effects |
Aplastic anemia |
|
|
Drugs that inhibit Nucleic Acid Synthesis |
DNA Replication: Quinolones/fluorquinolones, Metronidazole RNA replication: Rifampin |
|
|
Quinolones- Mechanism |
Target DNA gyrase (which nicks and reanneals DNA to relieve supercoiling) - inhibits DNA replication
|
|
|
Fluoroquinolones - Examples |
-Commonly used at Penn: Levofloxacin, norfloxacin -Ciprofloxacin
|
|
|
Fluoroquinolones- Uses |
-Not good for Gram+, good for Gram---
-Levofloxacin: active against many PNC-resistant pneumococci |
|
|
Fluoroquinolones-Properties |
-Safe -Good PO -Good tissue adsorption
|
|
|
Fluoroquinolones- Side Effects |
-Resistance: due to mutations in drug binding site @gyrase -C. difficile: by disrupting normal gut flora, can increase chance of getting C. difficile |
|
|
Metronidazole- Properties & Uses |
Properties -Bactericidal - disrupts DNA structure -administered as prodrug Uses: -Anti-parasitic -very good against anaerobes -C. difficile (also can use vancomycin) |
|
|
Sulfa drugs- Antimetabolites |
-group of related compounds collectively called sulfa drugs -target folic acid synthesis (humans don't have specific enzyme in folic acid pathway, allowing for selective toxicity) -inhibit growth of gram+ & gram- organisms -Resistance due to plasmid encoded alternative enzyme
|
|
|
Trimethroprim |
-Sulfa drug- inhibits folic acid synthesis -used synergistically w/ sulfonamide, e.g. Sulfamethaxazole |
|
|
Bactrim - Uses |
Bactrim = trimetroprim + sulfamethaxazole
|
|
|
Bactrim - Side Effects |
-hypersensitivity -dont give to pts taking warfarin (blood thinner), since it increases warfarin levels & can lead to bleeding |

