![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
113 Cards in this Set
- Front
- Back
|
What is the functional unit of the nervous system? |
Neuron (transmits electrical impulses to and from the brain. Interruption of signals cause signs based on the location of the lesions) |
|
|
Name 2 parts of the central nervous system |
Brain, spinal cord |
|
|
Name the 2 parts of the peripheral nervous system: |
Cranial nerves Peripheral nerves |
|
|
Name 1 disease related to the brain |
Trauma, Vestibular disease, neoplasia, seizure disorders |
|
|
Name 1 disease related to the peripheral nervous system. |
Deafness, metabolic neuropathy, megaesophagus, polyradiculoneuritis, facial nerve paralysis |
|
|
Name 1 disease related to the spinal cord. |
Intervertebral Disc Disease (IVDD), spinal cord trauma, atlantoaxial subluxation, cervical spondylomyelopathy, degenerative myelopathy, discospondylitis, ischemic myelopathy. |
|
|
Traumatic brain injury has acute clinical onset from a ______. |
traumatic event |
|
|
What are the 2 classes of traumatic brain injury? What is the difference? |
Primary event: direct injury to the tissues (may disrupt tracts that can't be repaired, or cause repairable cell damage which is reversible). Secondary event: Intensify the neurologic damage already there from a primary event. (ICP, edema, hypoxia, seizures). |
|
|
What are some of the clinical signs of Traumatic brain injury? |
Hx of head trauma, seizures, blood in ears, nose, oral cavity, ocular hemorrhage, anisicoria (unequal pupil size), loss of consciousness, decreased response to stimuli, shock, arrhythmias, altered resp. patterns. |
|
|
What can increased ICP (Intercranial pressure) cause? |
Cushing's reflex (results in bradycardia, hypertension, irregular resp., widening pulse pressures)
Usually seen in the terminal stages of acute head injury!! |
|
|
Hypertension, bradycardia, and widening pulse pressure are all examples of the ______. |
Cushing triad (this is a sign of ICP, where there is an increase in sympathetic outflow to the heart, where the body is trying to increase arterial BP and total peripheral resistance, this is accompanied by bradycardia). |
|
|
How would you diagnose traumatic brain injury? |
hx of trauma, clinical signs, chemistries to rule out other possible causes of neuro signs. |
|
|
True or False: Treatment for traumatic brain injury is very involved. You need to correct metabolic derangements, give oxygen, elevate their head and give drug therapies. |
True |
|
|
Match the drug therapy used in traumatic brain injury with its class:
1. Osmotic agents (decrease ICP/cerebral edema) 2. Antieleptics 3. Corticosteroids
A. Solu-Delta Cortef B. Mannitol, Diuretics, Hypertonic saline C. Valium, phenobarbital |
1. B 2. C 3. A |
|
|
There are 3 things that you want to check when doing an evaluation of brain trauma. These are: |
Gait/reflexes, Consciousness, PLR/OVR |
|
|
This disease is an acute disorder of dogs and cats, and is signified by inflammation around the 8th cranial nerve. |
Vestibular disease (idiopathic in older/middle aged animals, can reoccur) |
|
|
The neurological equipment that is responsible for perceiving one's body orientation relative to the earth is called the ______. |
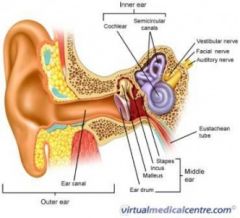
Vestibular apparatus |
|
|
What are 2 things that can cause vestibular disease? |
Idiopathic (unknown cause), middle ear infection, brain lesion, neoplasia, autoimmune inflammation. |
|
|
What are 2 clinical signs of vestibular disease? |
loss of balance, nystagmus (uncontrollable "shaking" of the eyeballs), disorientation, ataxia, vomiting/anorexia, circling, head tilt. |
|
|
Give two treatment options for vestibular disease. |
Antihistamines (centrally acting, reduce nausea/vertigo), steroids?, treat underlying ear infection (if present), supportive care, help them up/down/out, etc, it's not a stroke! |
|
|
True or False With neoplasia, tumors in the brain can cause compression on neurologic tissue and cause acute signs. |
False. Can cause progressive signs (symptoms are often VERY progressive, and treatment doesn't cure them). |
|
|
Primary tumors are usually ______. Metastatic tumors are usually ______. |
Primary=single Metastatic/secondary=multiples |
|
|
Clinical signs usually vary depending on the location of the tumor involved in neoplasia. Can you name 2 signs? |
Worsening seizures in old dogs, endocrine imbalances, vestibular signs, tremors, ataxia. |
|
|
How would you diagnose for neoplasia? |
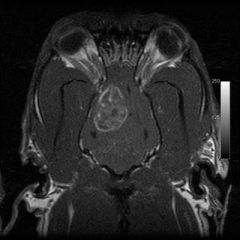
screening for tumors in other body regions, CBC/Chem/Lytes, Rads, CSF tap, ophthalmic exam, CT/MRI. |
|
|
Give 2 treatment options for neoplasia |
sx removal for single masses, radiation/chemo, antieleptics, corticosteroids. |
|
|
How are seizures categorized in cats and dogs? |
Extracranial vs. Intracranial Extracranial-outside the body. (Toxins, etc) Intracranial-inside the body (progressive (neoplasia) vs. non-progressive (epilepsy) |
|
|
What are 2 extracranial causes of seizures? |
Hypoglycemia, liver or kidney dz, hypocalcemia, hypothyroidism, hyperthermia, toxicoses (organophosphates/chocolate) |
|
|
What are 2 intracranial causes of seizures? |
Epilepsy, hydrocephalus, canind distemper encephalitis, thiamine deficiency, neoplasia, cranial trauma, cerebral infarction, degenerative conditions (lysosomal storage dz). |
|
|
Generalized seizures are also called ______ seizures. |
Tonic-clonic seizures |
|
|
What happens during the tonic phase of a seizure? |
animal falls, loses consciousness, limb rigidity |
|
|
What happens during the clonic phase of a seizure? |
paddling of the limbs, chewing, biting. May also defecate, urinate, mydriosis, hypersalivation. |
|
|
1. Partial seizure 2. Complex partial seizure
A. movements are restricted to one area of the body (usually associated w/ secondary epilepsy) B. psychomotor or behavioral (associated w/ bizarre/complex behaviors that are repeated during the seizures) |
1. A 2. B |
|
|
multiple seizures within a short period of time, and only brief consciousness between seizures is called ______.
One seizure lasting 30 minutes or longer, or multiple short seizures with no time in between are called ______.
A. Status epilepticus B. Cluster seizures |
1. B 2. A
Both should be treated as medical emergencies |
|
|
What are the 4 basic stages of a seizure? |
Prodrome behavior changes. can occur hours/days before seizure. Aura sensory/focal onset (percieved smell/deja vu/behavioral changes). Ictus The seizure event itself. Post-ictal Neurological status alterations hours/days after the seizure.
|
|
|
1.Prodrome 2.Aura 3.Ictus 4.Post-ictal
A. Time after the seizure B. Signals the start of the seizure C. Precedes the seizure (restlessness, mood/behavior change). D. The actual seizure |

1. C 2. B 3. D 4. A |
|
|
Paroxysmal transient disturbances of brain function are also called ______. |
seizures |
|
|
What are the two different types of epilepsy (determined by the cause)? |
Idiopathic (#1 cause in dogs and cats, unknown cause although a hereditary basis has been established) Secondary (when a cause can be determined) |
|
|
What breeds are predisposed to idiopathic epilepsy? |
German shepherd, golden retriever, labrador retriever, mini and toy poodles, saint bernard, cocker spaniel, beagle, irish setter. |
|
|
True or False In order to diagnose idiopathic epilepsy, you want to run a CBC and chemistries to rule out other possible causes, also a CT/MRI to rule out lesions in the brain. |
True |
|
|
Why would you want to wait to treat idiopathic seizures? |
because you want to establish a pattern of frequency(so you aren't treating them if it is only going to occur every 6 months), then start treatment when seizures occur every 4-8 weeks. |
|
|
What is one drug therapy that is used in idiopathic seizures? |
Potassium bromide, phenobarbital |
|
|
True or False Status epilepticus is not an emergency situation. |
False It is an emergency situation (can lead to irreversible brain damage and death, and high temps) |
|
|
Status epilepticus can cause high temps, and irreversible brain damage and death. What are some treatment options? |
Diazepam, Phenobarbital, Mannitol/Prednisone (if cerebral edema is suspected), Cool bath (for temps). |
|
|
Is epilepsy a curable disease? |
No. Medications will need to be given for the rest of their lives, and monitored/adjusted often. The can live a normal life once the seizures are controlled though. |
|
|
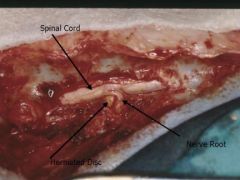
What is the outer fibrous layer of the intervertebral discs called?
|
Annulus fibrosus |
|
|
What is the inner gel-like nucleus of the intervertebral discs called? |
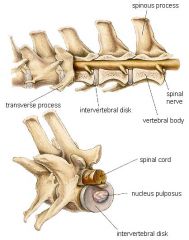
Nucleus pulposus |
|
|
One of the most common disk disorders are called ______. |
intervertebral disk disease (IVDD) Disks become dislodged, protruded, herniated, and ruptured |
|
|
What are the 3 most common areas for disc protrusion in IVDD? |
Cervical Caudal Thoracic Lumbar |
|
|
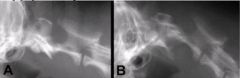
What are the 2 types of disc herniations in IVDD? |
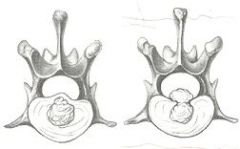
Hansen type I(right) (acute rupture, more common in small breed, younger dogs). Hansen type II (left) (less acute, more common in large breed dogs >5 years). |
|
|
What are 2 clinical signs of IVDD? |
Apparent pain, presence/absence of motor and sensory deficits, acute onset (type I), paresis or paralysis (can be unilateral), decreased panniculus reflex (quick twitch in sq muscle along back due to a pinprick), altered deep pain response. |
|
|
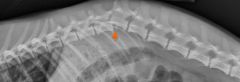
When diagnosing for IVDD, what is one thing that you may see on a radiograph. |
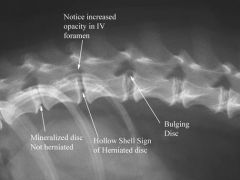
Narrowed intervertebral space at location of the lesion (C7-T1, T9-10, L7-S1), Opacity of the "horse's head" of intervertebral foramen.
Myelogram is required for definitive location of the lesion. |
|
|
Give a way to treat IVDD. |
With pain, can be managed medically. Confinement, corticosteroids, muscle relaxers, pain meds, intensive care nursing, PT.
If you have multiple episodes of ataxia, paralysis, and an absence of deep pain, that may require surgical intervention ASAP. |
|
|
Give one way to prevent IVDD. |
Prevent excess weight gain, avoid standing on hind legs, prognosis=poor if animals lack deep pain for 24 hrs.
40% have recurrence with more severe signs. |
|
|
There are two types of effects due to spinal cord trauma, what are they? |
Direct effects-due to primary disruption of pathways Indirect effects-result from edema, hemorrhage, inflammation, ischemia, neuronophagia causing autodissolution of the cord. |
|
Give a way to diagnose spinal cord trauma. |
History of trauma, Schiff-Sherrington (rigid hypertonicity of fron legs), lack of panniculus reflex, paresis or paralysis. |
|
|
How can you treat spinal cord trauma? |
Corticosteroids (Dexamethasone, Solu-Delta Cortef), Mannitol, treat other injuries, strict confinement for 8 weeks (if mild dislocation or fractures), surgical treatment, daily PT, bladder expression/catheter, nursing care. |
|
|
What type of dogs usually have atlantoaxial subluxation? |
Young toy/mini breeds.
(cranial portion of axis is displaced into spinal column) |
|
|
What are the two possible causes of atlantoaxial subluxation? |
congenital (birth defects) trauma or it can be both. |
|
What are some clinical signs of atlantoaxial subluxation? |
Young toy/mini breeds, reluctant to be patted on the head, tetraplegia(total paralysis of all limbs) or tetraparesis(weakness of all limbs), sudden death due to respiratory paralysis. |
|
|
What is the medical treatment for atlantoaxial subluxation? What is the surgical treatment? |
medical-Splint neck in extension (strict cage confinement for 6 weeks, steroids, pain meds) Surgical-stabilization/decrompression, stainless steel wire, bone grafts/cross pinning, hemilaminectomy to relieve compression. |
|
|
What is cervical spondylomyelopathy also known as? |
wobbler syndrome
(common in large breed dogs) Great dane (onset before 1 year of age), doberman (onset before 2 years old), borzoi, basset hound |
|
|
What are some clinical signs of cervical spondylomyelopathy? |
pelvic limb ataxia, dragging toes, crossing limbs, abnormal proprioception, swinging/wobbly gait in hind end, worse on rising, atrophy of scapular muscles, rigid neck flexion without pain. |
|
|
How can you diagnose cervical spondylomyelopathy? |
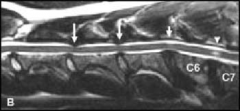
Rule out metabolic defects (esp. hypothyroidism), radiographs (may indicate malalignment or sliiping of vertebrae, narrowing of spinal canal, myelography, CT/MRI |
|
|
What is the medical treatment for cervical spondylomyelopathy? Surgical? |
Medical-cortisone, neck brace, cage confinement (3-4 weeks) Surgical-decompression and stabilization
prognosis is guarded (inherited defect) |
|
|
With IVDD, once deep pain is lost there is a....
____% chance of recovery with sx w/in 24 hrs
After ____ hours, prognosis is poor.
____to____% chance of progressive myelomalacia leading to respiratory paralysis. |
50% if sx w/in 24 hours after 48 hours, prognosis=poor 5-10% chance of progressive myelomalacia |
|
|
There are several different techniques/approaches for IVDD surgery, and they depend on the site of IVD rupture, what are 2 techniques? |
cervical spine-dorsal laminectomy or ventral spondylectomy (aka slot) thoracolumbar spine-dorsal laminectomy or hemilaminectomy |
|
|
Diffuse degeneration of white matter in all segments of the spinal cord is called ______. |
Degenerative Myelopathy (may be autoimmune) |
|
|
What type of dogs can get degenerative myelopathy? |
german shepherds, belgian shepherds, OES, Weimaraner
all are generally older that 5-6 years |
|
|
What is a clinical sign of degenerative myelopathy? |

slowly hind limb ataxia and paresis, loss of proproiception, muscle wasting, unable to support weight with rear limbs. |
|
|
What would a neurologic exam show with degenerative myelopathy? |
Decreased or absent proprioception and placing, increased to normal patellar reflexes, lack of pain, normal sphincter tone, normal panniculus reflex. |
|
|
What would radiographs show with degenerative myopathy? |
ossification and narrowed disc spaces |
|
|
Is there any treatment that is helpful when dealing with degenerative myelopathy? |
No treatment is helpful, irreversible damage to the spinal cord, and it is time to consider quality of life when they cannot support their weight. |
|
|
Inflammation of IV disk and/or vertebral bodies (vertebral osteomyelitis) is also called ______. |
Discospondylitis |
|
|
True or False Discospondylitis is usually caused by the hematogenous spread of bacterial or fungal infections from penetrating wounds, abscesses or infection, surgery, and grass lawns. |
True |
|
|
Discospondylitis can be caused by common infections such as what? |
UTI, bacterial endocarditis, dental extraction (immunosuppresion may play a role) |
|
|
What are some clinical signs of discospondylitis? |
Often vague and non-specific, wt. loss, fever, depression, reluctance to exercise, spinal pain, hyperesthesia. |
|

How would you diagnose discospondylitis? |
radiographs (may show lysis of bony end plates, osteophytes, decreased disk space), myelography (spinal compression), CBC (high WBC count), CSF (may show high WBC's and elevated protein), Culture and Sensitivity of blood, CSF, and urine, sx biopsy/tissue culture are definitive. |
|
|
How can you treat discospondylosis? |

long term antibiotic therapy (6 weeks to 6 months), analgesia, guarded prognosis
also, brucellosis can cause it (caution! zoonotic) |
|
|
Ischemic Myelopathy is caused by ______. |
Fibrocartilagenous Emboli (Necrosis of the spinal cord due to obstruction of veins and arteries, and have an acute onset, and severe neurologic deficit) |
|
|
What type of dogs get ischemic myelopathy? |
Giant/large breed dogs between 1 and 9 years old (less common in cats and small dogs). |
|
|
What is a clinical sign of ischemic myelopathy? |
acute onset of neurologic signs, lack of spinal pain, paresis or spastic paralysis, reluctance to move. |
|
|
How would you diagnose ischemic myelopathy? |
rule out all other causes, rads and labs are usually unremarkable, myelogram (spinal cord edema). |
|
|
What is a treatment option for ischemic myelopathy? |
administer corticosteroids (shock dose), good nursing care, most recover in a few months, prognosis is guarded but good, keep them comfortable and prevent further injury. |
|
|
______ is often associated with trauma to peripheral nerves. |
Neuropathic syndrome (reduced or absent muscle tone, wekness, or paralysis of affected limb or muscle). |
|
|
True or False Neuropathic syndrome may involve a single nerve or multiple nerves, and the cause is easily diagnosed. |
False, the cause is often unknown, so it is not easily diagnosed. |
|
|
Deafness resulting from central/peripheral (pick one) origin results from damage to CNS and auditory pathways. |
central origin |
|
|
Deafness resulting from central/peripheral (pick one) origin results from cochlear abnormalities. |
Peripheral origin |
|
|
Conductive/neural (pick one) deafness is usually associated with chronic otitis, rupture of the membrane, or damage to the middle ear. |
Conductive deafness |
|
|
Conductive/neural (pick one) deafness can be hereditary or congenital, drug therapy, or aging changes. |
Neural deafness |
|
|
True or False Congenital defects are partial or total agenesis (failure of organ to develop) of the hearing organ, organ of Corti, siral ganglion, or cochlear nuclei. |
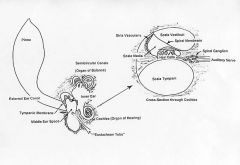
True |
|
|
Name 2 ototoxic drugs. |
Aminoglycosides (e.g. gentocin), polymyxin B, chloramphenicol |
|
|
What are 2 breeds that are predisposed to deafness? |

Dalmations, Bull terriers, dobermans, rottweilers, pointers, australian shepherds, english setters, cattle dogs, blue-eyed white cats. |
|
|
What are 2 clinical signs of deafness? |

lack of response to auditory stimuli, excessive sleeping, typical breed. |
|

How would you diagnose deafness? |
inability to arouse a sleeping patient with loud noises, evaluate responses to multiple auditory stimuli, specialty diagnostics (typanometry, acoustic reflex testing, auditory evoked responses) |
|
|
True or False Hearing loss in deaf animals is not permanent, and hearing aids are easy fixes. |
False (it is permanent, and most animals don't tolerate hearing aids). |
|
|
When dealing with Metabolic Neuropathy, polyneuropathy is caused by underlying diseases. Can you name one underlying disease? |
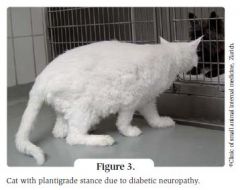
diabetes, hypothyroidism, hyperadrenocorticism |
|
|
This disease results in dilation of esphagus and regurgitation of food, and is a lack of effective peristalsis. |
Megaesophagus (risk of aspiration pneumonia with this disease) |
|
|
There are many causes of the acquired form of aspiration pneumonia, can you name 2? |
distemper, tick paralysis, lead poisoning, polymyositis, myasthenia gravis. |
|
|
When is the congenital form of megaesophagus usually noticed? |
Around the time of weaning |
|
|
What are 2 breeds that are predisposed to megaesophagus? |

Great Dane, German shepherd, irish setter, newfoundland, shar-per, greyhound. |
|
|
What are the management goals of megaesophagus? |

prevent aspiration pneumonia and nutritional deficiencies. (elevated feedings, small frequent meals, soft diet with high caloric density). |
|
|
What is tick paralysis associated with? |
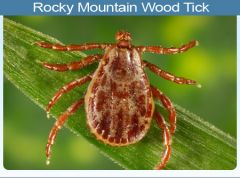
neurotoxin in saliva (common with dog tick, and rocky mountain wood tick) cats are resistant to this. |
|
|
How long after removal of a tick, will a dog recover from tick paralysis? |
1-3 days once the tick is removed |
|
|
How would you diagnose/treat tick paralysis? |
rule out the other causes of neuromuscular disease, remove all ticks, supportive care. |
|
|
What is acute Idiopathic Polyradiculoneuritis also called? |

Coonhound paralysis (it is passed on from a raccoon bite 7-14 days prior to onset) only sensitive dogs develop this disease. |
|
|
What does polyradiculoneuritis cause? |

Demyelination and degeneration of myelin and axons in nerve roots |
|
|
What are two signs of polyradiculoneuritis? |
Weakness in hind limbs, progresses to flaccid, systemic tetraplegia, absence of spinal reflexes, loss of voice, labored breathing, inability to lift head, conscious |
|
|
How would you diagnose polyradiculoneuritis? |
rule out all other infectious and metabolic causes, CSF analysis (increased TP, normal cell count), electromyography (denervation, slowed nerve conduction). |
|
|
What is one way to treat polyradiculoneuritis? |
Supportive nursing care, corticosteroids are not beneficial, respiratory support, may or may not regain total function, recovery can take 2-6 months. |
|
|
Facial nerve paralysis affects what breeds of dogs/cats? |

Cocker spaniels, corgis, boxers, english setters, longhaired cats. |
|
|
What are 2 clinical signs of facial nerve paralysis? |

Ear droop, lip paralysis, sialosis (excessive flow of saliva), deviation of the nose, absence of menace and palpebral reflexes. |
|
|
Give two ways to treat facial nerve paralysis. |
Corticosteroids, artificial tears, cause is unknown and complete recovery does not occur. |
|
|
What is something that may develop with facial nerve paralysis? |
May develop dry eye, and require lifelong supportive care. |

