![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
24 Cards in this Set
- Front
- Back
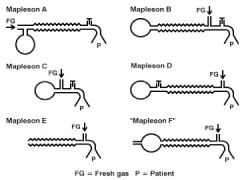
Describe approp use of the various delivery systems for Mapleson A, B, and C
|
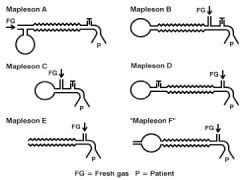
Mapleson A:
“Magill’s Circuit” FGF must = MV in order to prevent rebreathing of CO2 SV only!!! CV would require a FGF of >20LPM – inefficient Mapleson B: Use for SV or CV SV minimum FGF = MV x 2 CV minimum FGF = MV x 2-2.5 FGF moves closer to pt (vs A) Less rebreathing of CO2 Example – if norm MV is 5LPM, then x2 = 10LPM of FGF in order to prevent rebreathing Theoretically scavenging IS possible by connecting tubing to the pop-off valve Mapleson C: Water’s Circuit Can be used for SV or CV SV min FGF = MV x 2 CV min FGF = MV x 2-2.5 Short, large bore tubing allows mixing of gases Improved ability to get rid of alveolar gases b/c don’t have a long tubing acting as a reservoir, increases the likelihood that the pt will inhale fresh gases. Otherwise arrangement same as B |
|
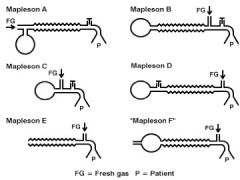
Describe approp use of the various delivery systems of Mapleson D, Baine, E, and F
|
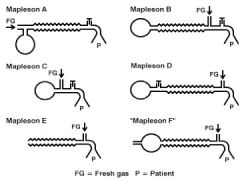
Mapleson D:
Reversal of A! Valve now in back and FGF in front closer to pt Amt of rebreath varies w/RR & TV (MV) b/c of arrangement of exp valve & FGF inlet CV or SV SV, FGF = 2-3 x MV CV, FGF = 1-2 x MV More efficient w/CV – use as low as 1 x MV (5LPM) bc now FG coming in close to pt, w/mix of gases in corrugated tubing Bain Circuit COAXIAL MODIFICATION of D! Initially developed for use on peds CV or SV FGF requirements same as D FGF is a tube w/in the large bore corruated tubing – allows exhaled gas to warm the inspired gas, preserves heat and humidity, eases scavenging Disadv – Potential for undetected inner tube leaks Must perform “Pethic Test” to determine if leaks are present Mapleson E: Modification of Ayre’s T-Piece Originally developed for craniofacial surgery Commonly used to admin O2 in ICU & PACU settings No Reservoir Bag! (exp limb tubing is reservoir) No Valve! CV or SV SV, FGF = MV x 2-3 CV, FGF = MV x 3 For use in CV – occlude non-pt end of tubing, FGF flows in, pt chest will rise, let go of occluded end, allow pt to exhale Mapleson F: “Jackson Rees Circuit” Modification of D, incorporates mechanism for release of exhaled gases Either have valve at end of bag or a fenestration in the bag itself When pressure gets too high, it opens up. Very pop in peds – little dead space and little resistance to breathing, and can control amt of inspiratory pressure Use to transport ICU pts CV or SV SV, FGF = MV x 2-3 CV, FGF = MV x 2 |
|
|
Identify and describe the advantages of the various delivery systems.
|

Follow the chart...
|
|
|
Compare and contrast the various types of anesth delivery systems (4 types) -> (open)
|
Open
No gas reservoir bag No rebreathing of exhaled gas 2 types (insufflation and open drop) Insufflation “Blow By” Advantages: Simple No rebreathing of CO2 Disadvantages: No ability to assist or control ventilation No control of anesthetic depth Open Drop “Schimmelbusch Mask” Advantages: Simple Inexpensive Portable Disadvantages: Cooling of anesth liquid decreases vapor production Accumulation of CO2 under mask Deep anesth predisposes to hypoxia risk SV only – No CV (SV=spont vent CV=controlled vent) OR pollution |
|
|
Identify components of the various delivery systems:
|
Components of Mapleson Circuits:
Breathing Tubes Fresh Gas Inlet (source) Pressure Relief Valve (Pop-off or APL) |
|
|
Compare and contrast the various types of anesth delivery systems (4 types) -> (semi-open)
|
Semi-Open
Gas reservoir bag Use of high FGF or unidirectional valve to prevent rebreathing Examples – Mapleson’s A-F 1950 Mapleson classified 6 prevalent systems (A-F) |
|
|
Rank Mapleson systems in order of efficiency for CV and SV:
|
Mapleson A is the most efficient for SV!
Mapleson D is a reversal of the A’s pressure relief valve and FGF inlet Mapleson D is the mose efficient during CV! A, B, & C’s no longer seen today D, E, & F’s are used today for weaning and transport, and in pts where you need to control the amt of pressure you are using when performing CV |
|
|
Compare and contrast the various types of anesth delivery systems (4 types) -> (semi-closed and closed)
|
See Next Lecture
|
|
Identify the main subsystems of an anesthesia circuit
|
There are 7 components to the circle system;
1. FGF source (common gas outlet) 2. Inspiratory and expiratory unidirectional valves 3. Inspiratory and expiratory corrugated tubing 4. Y-Piece connector 5. Pop-off valve (over flow, or APL valve) 6. Reservoir bag 7. CO2 absorber canister |
|
Describe how CO2 is eliminated from the circle system:
|
CO2 is removed via the CO2 absorbent in the canister as gas flows from bellows/reservoir bag to the pt.
Flow of gas: Expiration, Expiratory unidirectional valve, Reservoir bag (inflates), Bellows rise, APL valve, CO2 absorber canister where mixing of gases occur, Common (fresh) Gas Inlet, Inspiratory unidirectional valve, Breathing tube, Patient inhales. |
|
|
The chemical reaction for absorption with Soda Lime
|
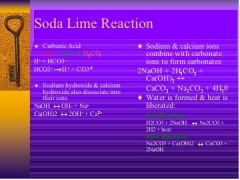
Soda Lime:
CO2+H2O =H2CO3(carbonic acid) Fast Reaction - H2O3+2NaOH=Na2CO3+2H2O+Heat Slow Reaction – Na2CO3+Ca(OH)2=CaCO3+2NaOH |
|
|
Draw the chemical reaction for absorption with Baralyme
|
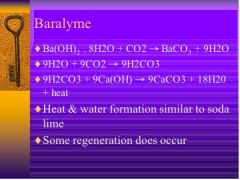
Baralyme:
Ba(OH)2 * 8H20+CO2 --- BaCO3+9H2O 9H2O+9CO2---9H2CO3 9H2CO3+9Ca(OH) --- 9CaCO3+18H20+heat Heat and water formation similar to soda lime. Some regeneration does occur. |
|
|
Compare and Contrasts the basics between Soda Lime and Baralyme
|
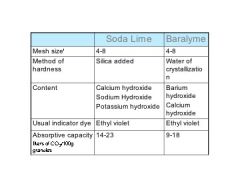
Soda Lime
4% Na+ hydroxide, 1% K+ hydroxide, 14-19% H20, 0.2% silica (to make harder), 80% Ca+ hydroxide Most common absorbent Capable of absorbing up to 23L of CO2 per 100g of absorbent. Silica added for hardness to prevent dust Water is present as thin film on granule surface Moisture is essential! Rxn takes place btw ions that only exist in presence of water (H20 makes rxns move forward) Baralyme (Barium Hydroxide lime) 20% barium hydroxide, 80% Ca+ hydroxide No silica No H20 Moisture incorporated as an octahydrate Ba(OH)2 * 8H20 |
|
|
Identify the main subsystems of an anesthesia circuit:
|
Open
Semi-Open Semi-Closed Closed |
|
|
The major difference btw these systems
|
***The major difference btw these systems is dependent upon the amt of FGF (fresh gas flow) coming into the system. (This was stressed about a gazillion times in lecture, so I’m sure we’ll be seeing it on the written or oral exam.)
|
|
|
Describe the use of a circle circuit as a semi-open, semi-closed, or closed system:
|
Semi-open
APL open, High FGF, scavenging possible Semi-closed APL is somewhat open or open all the way (depending on whether or not your are assisting the pt…), low flow rates 1-3 lpm, requires CO2 absorption Closed APL Closed, very low flows, 250-300 ml/min, requires CO2 absorption |
|
|
Compare and contrast semi-open, semi-closed, and closed systems:
|
Semi-Open System
Not used often No rebreathing occurs Requires a very high FGF FGF is 4-6 x pt’s MV; washes out CO2 Wastes gases and heat No conservation at all APL valve is open all the way Circle system can be converted to semi-open system by “de-nitrogenating” the pt, which means you don’t allow them to rebreathe O2, and you pre oxygenate them. Semi-Closed System Used most often in anesthesia practice in US today Low-moderate flow rates (1-3 lpm) Conserves heat and gases Some rebreathing of agents and exhaled gases (minus CO2) APL valve is somewhat open or open completely, depending on whether you are assisting the pt or not (vent mode = no APL; spont breathing = APL open) Closed System 3rd world countries Inflow of gas exactly matches that being taken up by the pt VERY low flows (Average 70kg pt would use 250-300ml/min) 2nd Thorpe tube is off No scavenging of any cases Total rebreathing of all gases except CO2 Total conservation of all exhaled gases APL valve is CLOSED Disadvantages: Metabolic need for O2 varies (incr in HR & BP require incr need for O2) Requires constant readjusting of flows, tedious for practitioner Must use math calc (very bad) Anesthetic depth is difficult to gauge |
|
|
Compare and contrast the 2 most common absorbent materials:
|
Soda Lime
4% Na+ hydroxide, 1% K+ hydroxide, 14-19% H20, 0.2% silica (to make harder), 80% Ca+ hydroxide Most common absorbent Capable of absorbing up to 23L of CO2 per 100g of absorbent. Silica added for hardness to prevent dust Water is present as thin film on granule surface Moisture is essential! Rxn takes place btw ions that only exist in presence of water (H20 makes rxns move forward) Baralyme (Barium Hydroxide lime) 20% barium hydroxide, 80% Ca+ hydroxide No silica No H20 Moisture incorporated as an octahydrate Ba(OH)2 * 8H20 |
|
|
CO2 Absorbent Overview (M&M, Ch 3)
|
Rebreathing alveolar gas conserves heat and humidity. However, the CO2 in exhaled gas must be eliminated to prevent hypercapnia. CO2 chemically combines w/H2O to form carbonic acid. CO2 absorbents (soda lime or barium hydroxide aka “Baralyme”) contain hydroxide salts that are capable of neutralizing carbonic acid.
|
|
|
Draw the chemical rxn for absorption w/each absorbent:
|
SODA LIME:
CO2 + H2O <---> H2CO3(carbonic acid) Fast Reaction H2O3 + 2NaOH <---> Na2CO3 + 2H2O + Heat Slow Reaction Na2CO3 + Ca(OH)2 <---> CaCO3 + 2NaOH BARALYME Ba(OH)2 * 8H20+CO2 <---> BaCO3 + 9H2O 9H2O + 9CO2 <---> 9H2CO3 9H2CO3 + 9Ca(OH) <---> 9CaCO3 + 18H20 + heat Heat and water formation similar to soda lime. Some regeneration does occur. |
|
|
Identify the end products of CO2 absorption
|
Reaction end products include heat, water, and calcium carbonate
|
|
|
Describe channeling and its consequences
|
Granule size is a compromise btw the higher absorptive surface area of small granules and the lower resistance to gas flow of larger granules.
|
|
|
Describe the cause of regeneration
|
Absorbent should be replaced when 50-70% has changed color. Altho exhausted granules may revert to their original color if rested, no signif recovery of absorptive capacity occurs.
|
|
|
How does regeneration manifest in day-to-day practice
|
Sarah intubates her patient, Brad Pitt, w/o any difficulty after unsuccessful attempts by both the anesthesia resident and anesthesiologist. 30 minutes into Brad’s elective “enlarging” surgery, Sarah notices that the CO2 absorbers are well over 75% purplish in color. She definitely recalls when performing the FDA checklist that the absorbers were present and NOT purple. Sarah knows that absorbers can revert to their normal color when left open overnight. She remembers that her friend, Ralph, had this very same room yesterday, and had probably bushwhacked her by not changing the exhausted absorbers. So Sarah jacks up the flowrate to wash CO2 out of the system, while this is a waste of gases it is necessary in this scenario.
|

