![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
8 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
Phase 1:
No CO2 Inspiration & 1st part of expiration Dead Space gas exhaled Phase 2: Sharp upstroke represents rising CO2 level in sample Slope determined by evenness of alveolar emptying Mixture of dead space and alveolar gas Phase 3: Alveolar Plateau Constant or slight upstroke Longest phase Alveolar gas sampled Peak at end of plateau is where the reading is taken – End Tidal Partial Pressure of CO2 (PEtCO2) Norm value = 30-40mmHg Reflection of PACO2 & PaCO2 Phase 4: Beginning of inspiration CO2 concentration Rapid decline to inspired value |
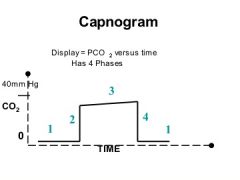
Interpret the shape of the normal capnogram
|
(Identify the phases)
|
|
|
Methods for measurement and detection of CO2: (2 main methods
|
Mainstream Capnography a.k.a. “Flow Thru”
Heated infrared measuring device placed IN circuit Sensor window must be clear of mucus Less time delay, quick reading Potential burns Weight of it can cause kinks in the ETT and leave marks on pt Sidestream Capnography Aspirates fixed amt gas/minute, range is 50-500ml, but usually 100-150ml Transports expired gas to sampling cell via tubing Near ETT is best location for sampling Big time delay Potential disconnect source Pediatric sampling (TV’s 100-200) Water vapor – condensation, traps & filters can clog up filter causing EtCO2 to stop working |
|
|
|
Methods of measuring CO2 in expired gases: (4)
|
Mass Spectrometry
Switching device directs gas from sampling line @ T-Piece to mass spec Sample is ionized & exposed to magnetic field in vacuum chamber Ionized gases then separated based on mass/charge ratio Allows for analysis of multiple gases w/increased accuracy Large and expensive Raman Analysis (RASCAL) Photons generated by increased intensity argon laser collide w/gas molecules Gas molecules momentarily excited to unstable vibrational & rotatory states Gases return to normal state, photons of characteristic frequency are emitted Scattered photons are measured as peaks in spectrum – determines concentration and composition of respiratory gases Colorimetric Rapid assessment of CO2 presence, not as accurate Metacresol purple impregnated paper CO2 + H2O = Carbonic Acid (changes color in presence of acid) Off-site anesthesia, a/w management, ICU/ER/code intubations Can be reliable indicator of proper ETT placement when used in combo w/auscultation of breath sounds Infrared Absorption Most common, rapid and reliable Infrared light transmission thru gas sample is measured and compared to gas that is free of CO2 |
|
|
|
. Compare & contrast capnometry, capnogram, and capnography
|
Capnometry – numeric representation e.g. EtCO2 30mmHG
Capnogram – time/concentration e.g. the actual curve itself Capnography – con’t monitor of capnogram e.g. multiple capnogram tracings |
|
|
|
Interpret the shape of the normal capnogram:
|
Phase 1:
No CO2 Inspiration & 1st part of expiration Dead Space gas exhaled Phase 2: Sharp upstroke represents rising CO2 level in sample Slope determined by evenness of alveolar emptying Mixture of dead space and alveolar gas Phase 3: Alveolar Plateau Constant or slight upstroke Longest phase Alveolar gas sampled Peak at end of plateau is where the reading is taken – End Tidal Partial Pressure of CO2 (PEtCO2) Norm value = 30-40mmHg Reflection of PACO2 & PaCO2 Phase 4: Beginning of inspiration CO2 concentration Rapid decline to inspired value |
|
|
|
Identify pt problems that can be detected by use of capnography:
|
Detects changes in ventilation, PaCO2, metabolic activity, & pulm bld flow; will produce characteristic waveform changes
May be used as estimate of PaCO2; average gradient is 2-5mmHg under GA Can determine incr. in metabolism such as malignant hyperthermia. MH produces incr. in CO2 before other s/s arise such as incr. temp Blocked pulm bld flow – CO2 on arterial side never makes it to alveoli – dramatic decrease of EtCO2. In order for EtCO2 to pick up anything, it needs to get to alveoli, detecting expired CO2. Obstructive Lung Dz’s (COPD, asthma, bronchoconstriction, acute obstx) will show slow rise in Phase 2 and little-no Phase 3. Smooth alveolar emptying not occurring. Gas trapping then happens. |
|
|
|
Increased CO2 (w/unchanged ventilation)
|
MH
Szr Shivering TQT release Release aortic vessel clamp IV bicarb Insufflation of CO2 into peritoneal cav Equipment defects (exp valve stuck, exhausted CO2 absorbers) |
|
|
|
Decreased CO2
|
Hyperventilation
Gradual decr relects increased minute vol (MV) Rapid decr reflects possible PE (thrombus, fat, amniotic fluid, air), V/Q mismatch, incr in PaCO2 & PEtCO2 gradient Cardiac Arrest – no C.O., no EtCO2 during MI Sampling error – disconnect, high sampling rate w/elevated FGF, esp on peds Decr BP – if pt becomes hypotensive, they won’t get enough bld flow to pulm circulation, causing a decr in ETCO2. |
|

