![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
89 Cards in this Set
- Front
- Back
|
male urethra consist of which parts
|
1 prostatic 2 spongious 3 membranous 4 intramural
|
|
|
The seminal colliculus (''hill'') is located in
|
prostatic part of urethra
|
|
|
the kidneys are fixed in their position by
|
1 adipose renal capsule/perirenal fat 2 intraabdominal pressure 3 ant/prerenal & post/retrorenal fascia
|
|
|
topology of crossing of deferent duct and ureter
|
deferent duct goes above ureter
|
|
|
urinary bladder, physiological capacity
|
500 mL
|
|
|
the external spermatic fascia is a continuation of the following layer of the anterior abdominal wall
|
superficial abdominal fascia
|
|
|
the narrowest points on the ureter are
|
during its passing through the wall of the bladder
|
|
|
the ampulla of the deferent duct
|
is located medially to the point of crossing of the deferent duct w the ureter
|
|
|
topological projections onto renal pelvis
|
1 tail of pancreas/cauda pancreatis project to the left from it 2 descending part of duodenum project onto right one
|
|
|
mesosalpinx, structure, function, continuation of what
|
double fold of peritoneum (contain blood vessels), fixates uterien tube, continuation of broad lig./lig. latum uteri
|
|
|
Ureter, path through abdomen
|
retroperitoneal
|
|
|
the ureter crosses
|
1 deferent duct 2 uterine a 3 commonoiliac a 4 psoas major m
|
|
|
color of urinary bladder mucosa in a healthy individual
|
intensive red
|
|
|
Differences between left and right renal a
|
right renal a is longer than the left one
|
|
|
which arterial branches do we get from the right renal artery
|
testicular artery
|
|
|
which renal a is a direct branch of aorta?
|
left
|
|
|
fixation of ovaria
|
1 lig. suspensorium 2 lig mesovarium 3 lig propria ovaria
|
|
|
lig latum uteri, originate from, path, characteristic feature
|
peritoneum (its a peritoneal fold), descend over uterus and uterine tubes, most caudal extension of pelvic cavity
|
|
|
muscles underlying each kidney
|
quadratus lumborum, psoas major
|
|
|
navicular fossa
|
terminal dilated portion of urethra in glans penis
|
|
|
parts of epididymis
|
1 head (above superior pole of testis) 2 body 3 tail
|
|
|
penis, fixation
|
lig fundiforme (''sling-shaped''), lig suspensorium penis
|
|
|
prostatic part of urethra contain
|
colliculus seminalis (hill w opening of the two ejaculatory ducts and utriculus prostaticus) & utriculus prostaticus (analog of uterus & vagina)
|
|
|
relative location of left and right kidneys
|
right kidney is half a vertebra lower due to the liver
|
|
|
retroperitoneal space contains
|
1 organs of urinary system 2 adrenal glands 3 aorta+inferior vena cava 4 sympathetic trunk
|
|
|
testis, Layers (int -> ext)
|
1 tunica vaginalis (serous from peritoneum, epichorium (visc) and perichorium (parietal)) 2 internal spermatic fascia (<- transveralis fascia) 3 Cremasteric fascia (cremaster m (<- internal oblique m)) 4 External spermatic fascia (<- fascia of external oblique m) 5 scrotum (house dartos fascia = smooth m)
|
|
|
urogenital diaphragm, shape, consist of
|
triangular, 1 m transversus perineal profundus (sphincter urethra is derived from it) 2 m transversus perineal superficiale
|
|
|
uterus, a supply
|
a uterina (from a iliaca int)
|
|
|
uterus, ligaments
|
1 l latum uteri 2 l cardinal uteri/mackenrodts lig 3 l teres uteri 4 l pubovesicalia 5 l vesicouterina 6 l rectouterina 7 l sacrouterina
|
|
|
when can testes/ovaries be spotted?
|
12th week
|
|
|
when can we see the kidneys?
|
6th week
|
|
|
constrictions of ureter
|
1 exiting renal pelvis 2 entrance into lesser pelvis in front of sacroiliac j 3 intramural
|
|
|
ejaculatory duct, where, made from
|
prostate, vas deferens+excretory duct of seminal vesicles
|
|
|
inferior vena cava in the abdomen is located to the ... of the center
|
right
|
|
|
transverse section at L1, 1-7?
|
1 fascia renalis 2 lamina prerenalis 3 lamina retrorenalis 4 corpus adiposum perirenale 5 corpus adipsoum pararenale 6 peritoneum 7 fascia transversalis
|
|
|
The kidneys
a. Renal sinus b. Which kidney is usually larger c. Weight d. Size |
a. Renal sinus
The cavity of the kidneys, containing the calices and pelvis of the ureter and the segmental vessels embedded within a fatty matrix. b. The right kidney. c. An adult kidney weighs 120-300g. d. 10-12 cm long, 5-6 cm wide, 4 cm thick. (Thieme) |
|
|
The kidneys
a. Structures of the renal medulla b. Structures of the renal cortex |
a. Renal medulla
1. Renal pyramids (Base against cortex, apices called renal papillae against hilum into renal calices) (Outer reddish zone, inner lighter zone) (Striated and pale) 2. Renal papillae I. Cribriform area - numerous perforations produced by the openings of papillary ducts b. Renal cortex - 1 cm below capsule 1. Renal columns - extensions between the renal pyramids (The cortical part containing the renal columns\between the medullary rays are called the cortical labyrinth) 2. Medullary rays - striations from extensions of the base of the renal pyramids (The cortical part containing the medullary rays are known as the cortex corticis) (Thieme) |
|
|
The kidneys
a. Uriniferous tubules - components, basis for differentiation b. Describe the nephron c. Describe the parts of the collecting duct |
a. Nephron and collecting ducts, different embryological origins.
b. Nephron Renal\Malpighian corpuscle 1. Glomerulus (Capillary cluster) 2. Glomerular\Bowman's capsule Renal tubule 1. Proximal tubule I. Proximal convoluted tubule II. Proximal straight tubule\thick descending limb of loop of Henle 2. Thin\Intermediate tubule I. Descending thin limb II. Ascending thin limb 3. Distal tubule I. Distal straight tubule\Thick ascending limb of loop of Henle II. Distal convoluted tubule 4. Junctional\Connecting tubule c. Collecting duct I. <- Connecting\Junctional tubule II. -> Papillary duct which opens on the tip of the papilla (Each collecting duct receives appx 10 nephrons) (Thieme) |
|
|
The kidneys
a. Describe the pathway of the renal vessels b. Straight arterioles and venules |
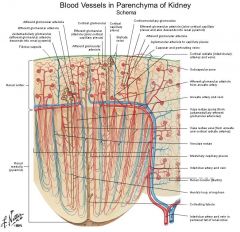
a. The pathway of the renal vessels
1. Renal artery -> 2. Interlobar arteries -> (Between renal pyramids toward the cortex) 3. Arcuate arteries -> (At the corticomedullary border) 4. Interlobular arteries -> (Radiate toward the fibrous capsule) 5. Afferent glomerular arterioles -> 6. Gomeruli -> 7. Efferent glomerular arterioles -> 8. Peritubular capillaries -> 9. Interlobular veins -> 10. Arcuate veins -> 11. Interlobar veins -> 12. Renal vein b. In juxtamedullary nephrons, follow the loop of Henle. Efferent arteriole -> straight arterioles -> straight venules -> arcuate veins. (Thieme) |
|
|
The nephron
a. Glomerular\Bowman's capsule b. Filtration membrane c. Give the epithelium for the proximal tubule, intermediate tubule, distal tubule, and collecting duct |
a. Glomerular\Bowman's capsule
The expanded beginning of a nephron composed of an inner and an outer layer. I. The inner visceral layer consist of podocytes that surround a tuft of capillaries. II. The outer parietal layer consist of simple squamous epithelium that become cuboidal at the urinary pole. (Thieme call only the parietal layer Bowman's capsule..) b. Filtration membrane 1. Capillary endothelium with fenestrations 2. Fused basement membrane 3. Podocytes with primary processes which give rise to secondary or foot processes which interdigitate, but leave narrow gaps, or filtration slits, between them. c. Renal epithelium - all are simple 1. The proximal tubule - cuboidal cells, long microvilli, infoldings and abundant mitochondria at the basolateral surface (Proximal convoluted tubule and thick descending limb of loop of Henle) 2. Intermediate tubule Squamous, short microvilli (Thin descending and ascending limb of loop of Henle) 3. The distal tubule Cuboidal cells, basal striations (basal mitochondria), short microvilli (Thick ascending limb of loop of Henle, distal convoluted tubule, junctional\connecting tubule) 4. The collecting ducts I. 2\3 pale-staining epithelial cells with distinct cell borders, progressively flatter II. 1\3 dark-staining intercalated cells (Microvilli = brush border) (Thieme) |
|
|
The kidneys
a. Which veins drain only into the left renal vein b. Location of hilum in relation to the vertebral column c. Fasial layers |
a. Left renal vein
I. Left suprarenal vein II. Left testicular\ovarian vein b. Hilum - L1 (Superior pole - T12, Inferior pole - L3, the right kidney usually lies about one half vertebra below the left) c. Fascial layers 1. Inner perirenal fat capsule (Surround the entire kidney and adrenal gland) 2. Outer fascial pouch I. Thin anterior layer II. Tough posterior layer (Connected at the superior and lateral border. Not present at the inferior border, closed only by adipose tissue here) (Thieme) |
|
|
The kidneys
a. Number of major calices b. Number of minor calices c. Number of renal papillae opening into one minor calices d. The two variations of the renal pelvis |
a. 2-3 major calices.
b. 8-10 minor calices. c. 1-3 renal papillae opens into each minor calyx. d. The renal pelvis I. The branching type - if the minor calices consistently opens into the major calices II. The ampullary type - if the minor calices also opens directly into the renal pelvis (The volume of the renal pelvis is 3-8 mL) (Thieme) |
|
|
The renal pelvis and ureter
a. Histology of the walls b. Arterial supply of the ureter c. The constrictions of the ureter d. Topography\Pathway of the ureter |
a. Histology
Renal pelvis and ureter 1. Mucosa - urothelium\transitional epithelium (5-7 layers, can adapt to the amount of distention by altering the height and number of cell layers. The thickened apical membrane in the top layer of the cells protects the epithelial cells from hypertonic urine.) 2. Muscular layer I. Inner longitudinal II. Outer circular Only distal ureter - III. Outer longitudinal 3. Adventitia (The lumen of the ureter is star-shaped) b. Arterial supply of the ureter 1. The renal arteries 2. The testicular\ovarian arteries 3. The internal pudendal arteries 4. The superior vesical arteries (Equivalent veins) c. Ureteric constrictions 1. The first point of constriction of the ureter - as it exits from the renal pelvis 2. The second point of constriction of the ureter - where it enters the lesser pelvis in front of the sacroiliac joint I. Right ureter - at the level of the bifurcation of the common iliac artery II. Left ureter - at the level of the external iliac artery 3. 3rd point of constriction of the ureter - the intramural part (2cm long) d. Topography\Pathway of the ureter 1. Medial side of psoas major - between its muscle fascia and the peritoneum in front of it I. Crossed over by the testicular\ovarian vessels II. Crosses the genitofemoral nerve 2. Enters the lesser pelvis in front of the sacroiliac joint I. The left at the level of the external iliac artery II. The right at the level of the bifurcation of the common iliac artery 3. Pass immediately beneath the peritoneum along the lateral wall of the pelvis. I. Male - reach the posterolaterla wall of the urinary bladder at a point above the seminal vesicle, crossing below the ductus deferens II. Female - run in the base of the broad ligament of uterus, crosses under the uterine artery, enter the urinary bladder posterolaterally. (Thieme) |
|
|
The urinary bladder
a. Parts b. The capacity of the urinary bladder c. How high can it extend when its distended d. The trigone of the bladder - what, special characteristic |
a. The urinary bladder
1. The body - the largest part 2. The apex - anterosuperior, give rise to the obliterated urachus (Which pass in the median umbilical ligament) 3. The fundus - Lateral-posterior, opening of ureters 4. The neck - Inferior - continuous with the urethra. b. 500 mL (The urge to void starts at 300 mL) c. Up to the superior border of the pubic symphysis. d. The trigone of the bladder I. The triangle formed by the ureteric orifices and the internal urethral orifice II. No mucosal folds due to its firm attachment to the underlying muscular layer and its absence of lamina propria. (Uvula of the bladder projects into the internal urethral orifice from the prostate in males) (Thieme) |
|
|
the urinary bladder
a. Histology b. Arterial supply c. Venous drainage d. Lymphatic drainage |
a. Histology of the urinary bladder
1. Mucosa I. Transitional epithelium\Urothelium II. Lamina propria mucosae (Loose CT, absent at trigone of the bladder) 2. Muscular layer I. 3 layers in detrusor muscle (all except trigone of bladder\neck) II. 2 layers at the trigone of the bladder, sphincteric arrangement at the internal urethral orifice 3. Serosa I. Subserosa b. Arterial supply Internal iliac artery -> 1. Superior vesical artery 2. Inferior vesical artery c. Venous drainage Vesical venous plexus -> internal iliac veins. d. Lymphatic drainage 1. Upper and lateral portions -> external iliac nodes 2. Fundus, the trigone of the bladder, and the anterior wall -> internal iliac nodes (Extrinsic and intrinsic nervous systems like in the intestine) (Thieme) |
|
|
Urethra
a. Length of the female urethra b. Length of the male urethra c. Histology of the urethral wall |
a. 3-5 cm
b. 20 cm c. Histology of the urethral wall 1. Mucosa - longitudinal folds I. Transitional epithelium II. Lamina propria mucosae (Abundant veins and urethral glands) 2. Muscular layer I. Inner longitudinal II. Outer circular (Thieme) |
|
|
The male reproductive organs
a. The internal organs b. The external organs b. Embryological origins of a and b |
a. The internal organs
1. Testis 2. Epididymis 3. Ductus deferens 4. Accessory sex glands I. Prostate II. Seminal vesicle\seminal glands III. Bulbo-urethral glands\Cowper's glands b. The external male genitalia 1. Penis 2. Scrotum 3. Tunics of the testees b. Embryological origins a. <- arise above the pelvic floor from the urogenital ridge b. <- derived from the urogenital sinus below the pelvic floor (Pelvic floor\diaphragm - the paired levator ani and coccygeus, together with the fascia above and below them.) (Thieme) |
|
|
Testis and epididymis
a. Size of testis b. What is the name of the connective tissue capsule investing each testis c. Appendix of testis - where, what d. Epididymis - parts |
a. 4-5 cm x 3 cm
b. Tunica albuginea. c. Appendix of testis I. Superior pole II. Remnant of the embryonic Mullerian duct d. Epididymis 1. Head (Above superior pole, appendix of epididymis is a remnant of the mesonephros) 2. Body 3. Tail (One duct, has its own CT capsule, (Lie posterior on the testis) (Thieme) |
|
|
The testis and epididymis
a. Processues vaginalis testis b. Layers of testis - from internal to external c. Lobule of testis - produced by, #, each lobe contains |
a. Processus vaginalis testis
Transitory peritoneal diverticulum that traverse the inguinal canal preceding the testis in males. In the male it degenerates except the caudal part which forms the tunica vaginalis testis. In females it disappears. (Can persist as canal of Nuck) b. Layers of testis from internal to external 1. Tunica albuginea (CT capsule) 2. Tunica vaginalis of testis I. Visceral layer - eporchium II. Parietal layer - periorchium (Serous sheath of testis and epididymis) 3. Internal spermatic fascia (<- Transversalis fascia) 4. Cremasteric fascia (<- Internal oblique, cremaster muscle) 5. External spermatic fascia (<- External oblique) 6. Skin of scrotum (Continuous with abdominal skin, heavily pigmented, hairy, sebaceous glands, subcutis w\o fat) I. Dartos fascia - subcutaneous tissue - smooth muscle cells, no fat (The scrotum is divided in two by septum of scrotum) c. Lobule of testis I. From invaginations of tunica albuginea (Converge to form mediastinum testis) II. 200-300 III. Several (convoluted) seminiferous tubules (Thieme) |
|
|
Testis and epididymis
a. Name the pathway from the site where spermatogonia are produced to duct of epididymis b. Cells in the seminiferous tubules and surroundings |
a. Pathway
1. Seminiferous tubules -> (200-300, in lobules of testis) 2. Straight tubules -> 3. Rete testis -> (In mediastinum testis) 4. Efferent ductules -> (Form lobule of epididymis) 5. Duct of epididymis in its head b. Cells in the seminiferous tubules and surroundings 1. Leydig cells - in interstitial tissue 2. Myofibroblasts and fibroblasts - surroudn the seminiferour tubules 3. Germinal epithelium - line the seminiferous tubules I. Spermatogenic cells (Lie along the basement membrane. Type A spermatogonia - stem cells, mitotic. Type B are precursors to spermatozoa - meiotic. (Thieme) II. Supporting Sertoli cells |
|
|
Testis and epididymis
a. Outline the changes and path from spermatogonia to spermatozoa b. Parts of a spermatozoa c. Sertoli cells - location, function |
a.
1. Type A spermatogonia -> Type B spermatogonia (Stem cell, mitotic) 2. Type B spermatogonia -> Primary spermatocyte (Mitotic, precursor to spermatozoa) (1-2 on basement membrane) (Primary spermatocyte - 4n DNA) 3. Primary spermatocyte -> Secondary spermatocyte (1st meiotic division - 24 days for prophase, during which recombination of genetic material occur) (Secondary spermatocyte - 2n DNA) 4. Secondary spermatocyte -> spermatids (2nd meiotic division, 1n DNA) (Gradually ascend into the lumen during the proliferation and differentiation) 5. Spermatid maturation -> Spermatozoa (Spermatozoa capable of fertilization, nuclear condensation, acrosome formation, flagella formation) b. Spermatozoa 1. Head - dense nucleus, acrosomal cap 2. Tail I. Neck II. Middle piece (Rich in mitochondria) III. Principal piece IV. End piece (60 um long) c. Sertoli cells I. On basement membrane II. Numerous cell junctions = blood-testis barrier -> basal compartment and adluminal compartment of the germinal epithelium (Germ cells can pass through) II. Nourish and facilitate transport of germ cells (Thieme) |
|
|
Eponyms
a. Stellate veins\Venulae Stellatae b. Renal columns c. Rectoprostatic fascia d. Retropubic\Prevesical space |
a. Verheyen stars
(The star-shaped group of venules in the renal cortex.) b. Bertin columns (The prolongations of cortical substance separating the pyramids of the kidneys.) c. Denonvilliers (rectoprostatic) fascia (A fascial layer that extends superiorly from the central tendon of the perineum to the peritoneum between the prostate and rectum.) d. Retzius space (The area of loose connective tissue between the bladder with its related fascia (umbilicovesical fascia) and the pubis and anterior abdominal wall.) (Netter\Stedman) |
|
|
The kidneys
a. Vascular segments of the kidneys b. Which area of the kidneys are most susceptible to ischemia c. Vasa recta vera & spuria |
a. Vascular segments of the left kidney - renal artery ->
Posterior branch 1. Posterior segment Anterior branch 2. Anterior superior segment 3. Anterior inferior segment 4. Superior segment 5. Inferior segment (Embryonic lobes, segments of the renal artery: renal artery -> segmental arteries -> interlobar arteries) b. The inner zone of the renal pyramids. c. Arteries penetrating and supplying the renal medulla (pyramids). I. Vasa recta vera - from arcuate and interlobular\cortical radiate arteries II. Vasa recta spuria - from juxtamedullary efferent glomerular arterioles (Netter, Stedman) |
|
|
Variation in the renal vein
|
Variation in renal vein
1. Double left renal vein may form ring around abdominal aorta. 2. Multiple renal veins. 3. Persistent left inferior vena cava may join left renal vein. (Netter) |
|
|
Pelvis
a. Uterosacral\Sacrogenital folds |
a. Uterosacral\Sacrogenital folds
Peritoneal folds that extend backward from the sides of the bladder of the male or uterus of the female on either side of the rectum to the sacrum, forming the lateral boundaries of the rectovesical pouch or rectouterine pouch. |
|
|
The testis
a. Rete testis - location, histology b. Efferent ductues - #, histology c. The duct of epididymis - histology d. Temperature in the testis |
a. Rete testis
I. In mediatsinum testis II. Simple squamous\cuboidal epithelium b. Efferent ductules I. 12-20 II. Pseudostratified epithelium - squamous for absorption, columnar with kinocilia for transport (Kinocilia - A cilium, usually motile, having nine peripheral double microtubules and two single central ones.) c. The duct of epididymis I. Pseudostratified tall columnar epithelial cells with stereocilia (Produce secretion which assist in sperm maturation) (Stereocilia - a nonmotile, long microvillus) II. A few smooth muscle cells in the wall d. At least 2 degrees below the core temperature. (The higher temperature in inguinal testes nondescented testes prevent sperm production) (Thieme) |
|
|
Testis and associated structures
a. Arterial supply b. Venous drainage c. Innervation d. Lymphatic drainage |
a. Arterial supply
1. Aorta -> testicular artery -> testes, branch to epididymis 2. Patent part of umbilical artery -> artery to ductus deferens -> ductus deferens, testes, seminal vesicle 3. Inferior epigastric artery -> cremasteric artery -> tunics of testes 4. Internal pudendal branches -> scrotum (1-3 anastomose) b. Venous drainage 1- Testes and epididymis -> pampiniform ('tendril-shape') venous plexus -> right testicular vein (-> IVC), left testicular vein (-> left renal vein) 2. Tunics and scrotum -> I. Great saphenous vein II. Inferior epigastric vein III. Internal pudendal vein (The pampiniform plexus are valveless -> varicocele) c. Innervation 1. Sympathetic fibers from the celiac plexus follow the arteries 2. Ilioinguinal and pudendal nerves -> scrotal nerves -> scrotum 3. Genital branch of genitofemoral nerve -> cremaster muscle d. Lymphatic drainage 1. Testes and epididymides -> lumbar nodes 2. Tunics of the testes, scrotum -> inguinal nodes (Thieme) |
|
|
Ductus\Vas deferens
a. What, opens into b. Ejaculatory duct c. Histology d. Parts |
a. The continuation of the duct of the epididymis. Opens into the ejaculatory duct in the prostatic urethra.
(35-40 cm, form the ampulla of ductus deferens right before opening into the ejaculatory duct) b. Ejaculatory duct I. The duct formed by the union of the deferent duct and the excretory duct of the seminal vesicle. II. Opens into the prostatic urethra. c. Histology I. Star-shaped II. Layers 1. Pseudostratified, stereociliated, columnar epithelium (Thin underlying CT) 2. Muscular layers - outer & inner longitudinal, middle circular 3. Adventitia d. Parts 1. The scrotal part (Along the inner aspect of the epididymis) 2. The funicular part (Funiculus spermaticus, surrounded by veins in the spermatic cord) 3. The inguinal part (Inguinal canal, deep to peritoneum, cross inferior epigastric and external iliac vessels) 4. the pelvic part (Cross linea terminalis into the lesser pelvis) (Thieme) |
|
|
Ductus\Vas deferens
a. Arterial supply b. Venous drainage c. Innervation d. Lymphatic drainage |
a. Arterial supply
Patent part of umbilical artery -> artery to ductus deferens b. Venous drainage 1. Pampiniform venous plexus (-> right testicular vein goes to IVC, left testicular vein goes to left renal vein) 2. Vesical and prostatic venous plexus c. Innervation Inferior hypogastric nerve plexus d. Lymphatic drainage Lumbar nodes (Thieme) |
|
|
The male genital system
a. The spermatic cord\funiculus - from-to, components b. The spermatic cord\funiculus - coverings |
a. The spermatic cord - deep inguinal ring->scrotum
1. Ductus deferens 2. Testicular artery 3. Artery to ductus deferens 4. Pampiniform venous plexus 5. Testicular vein 6. Autonomic nerves 7. Genital branch of genitofemoral nerve b. Internal spermatic fascia, cremasteric fascia, external spermatic fascia. (Gradually as it progress through the inguinal canal) (Thieme) |
|
|
The seminal vesicles
a. Location b. Connection to the ejaculatory duct in the prostatic urethra - which structure does it join here c. Histology d. Secretion e. Arterial supply |
a. Against the posterior surface of the urinary bladder, lateral to the ampulla of ductus deferens.
(Their lateral, superior portions are covered by peritoneum, 5 cm long) b. Excretory duct of seminal vesicles -> ejaculatory duct along with ductus deferens c. Simple layer of various height cells. d. Alkaline fluid rich in fructose. (Make up the majority of the secretion) e. Arterial supply 1. Inferior vesical artery 2. Artery to ductus deferens 3. Middle rectal artery (Inferior hypogastric nerve plexus, internal iliac nodes) (Thieme) |
|
|
The prostate
a. Location - anterior, posterior, inferolateral, base of prostate, apex of prostate b. Pierced by c. Anatomical parts d. The prostate is an exocrine organ - # glands, type, connection to male urethra |
a. Below the urinary bladder on the pelvic floor.
I. Anterior surface - pubic symphysis II. Posterior surface - rectum III. Inferolateral surface - lateral pelvic wall (Adjacent to the inferior hypogastric nerve plexus) IV. The base of prostate - fused to the fundus of the urinary bladder V. The apex of prostate - face the urogenital diaphragm (Urogenital diaphragm - between ischiopubic ramus, 3-layered: superior fascia of diaphragm, deep transverse perineal muscle & sphincter urethrae, perineal membrane) b. The male urethra and the ejaculatory ducts. c. Anatomical parts 1. Right and left lobes 2. The isthmus of prostate 3. The middle lobe d. 40 tubuloalveolar glands. Prostatic ductules -> openings around the seminal colliculus. (Thieme) |
|
|
The prostate
a. Composition b. Secretion c. Clinical divison d. Arterial supply e. Venous drainage f. Innervation g. Lymphatic drainage |
a. Composition
I. Parenchyma - 40 tubuloalveolar glands with prostatic ductules (Pseudostratified columnar) II. Fibromuscular stroma - CT, smooth muscle III. Tough CT capsule b. Secretion Numerous enzymes - acid phosphatase (15-30% of the seminal fluid) c. Clinical division 1. The transitional zone - enclose the urethra to the level of the opening of the ejaculatory ducts 2. Central zone - glandular tissue surrounding the transitional zone and the ejaculatory duct 3. The peripheral zone - outer, lower zone (Benign prostatic hyperplasia - central zone, tumor - peripheral zone. Enlargement of the central zone has a more obstructive effect) d. Arterial supply 1. Internal pudendal artery branches 2. Inferior vesical artery branches 3. Middle rectal artery branches e. Venous drainage Prostate, seminal vesicle -> prostatic venous plexus (Connected with the vesical venous plexus) f. Innervation Inferior hypogastric nerve plexus g. Lymphatic drainage Internal iliac and sacral nodes (in the concavity of the sacrum - drain the rectum and posterior pelvic wall). (Thieme) |
|

|

Netter
|
|
|
Penis
a. Cavernous bodies b. Parts c. Name of superior side, inferior side |

b. 2 corpus cavernosum penis, 1 corpus spongiosum penis surrounding the urethra.
b. Parts of penis 1. Root of penis - the part attached to the pubis and the perineum 2. Body of penis c. Superior - dorsum of penis, Inferior - urethra. surface (Thieme) |
|
|
Penis
a. Root of penis - parts b. Root of penis - attachments c. Body of penis - parts and characteristics d. Glans penis |

a. Root of penis
1. Crura of penis - proximal part of corpus cavernosum penis, connected to inferior pubic rami 2. Ischiocavernosus muscle - striated, surround crura of penis 3. Bulb of penis - thickened proximal part of corpus spongiosum, between crura of penis, connected to urogenital diaphragm 4. Bulbospongiosus - cover bulb of penis b. Attachments 1. Bulb of penis - urogenital diaphragm 2. Crura of penis and ischiocavernosus - inferior pubic rami 3. Fundiform ('looped') ligament of penis (A band of elastic fibers of the superficial fascial layer that extends from the linea alba above the pubic symphysis splitting to surround the penis before attaching to the Dartos fascia of the penis.) 4. Suspensory ligament of penis (A fibrous band at the deep fascial layer that extends from the pubic symphysis to the deep fascia of the penis\Buck's fascia anchoring the roof of the penis.) c. Body of penis 1. Corpus cavernosum penis I. Dual-chambered II. <- Crura of penis III. Covered by tunica albuginea of corpora cavernosa - also form a median partition of the corpora cavernosa - septum penis 2. Corpus spongiosum I. Tunica albuginea of corpus spongiosum (Thinner than for #1) II. <- Bulb of penis 3. Tough fascia\Buck fascia I. Surround the three erectile bodies 4. Superficial fascia d. Glans penis I. Termination of corpus spongiosum II. External urethral orifice III. Corona of glans (Thieme) |
|
|
Penis
a. Subcutaneous tissue of penis - characteristics b. Corpus cavernosum - histology c. Corpus cavernosum - arteries and veins d. Corpus spongiosum - histology |

a. Subcutaneous tissue of penis
I. No fat II. Forms prepuce of penis b. Corpus cavernosum Lined by endothelium in a framework of collagenous and elastic fibers and a network of smooth muscle cells called trabeculae of corpora cavernosa. (Slits -> several mm cavities) c. Corpus cavernosum I. Internal pudendal artery -> Deep artery of penis -> helicine ('coiled') arteries II. Subfascial and epifascial veins d. Corpus spongiosum I. Wide vascular spaces lined by endothelium but less prominent fibromuscular framework -> soft filling -> permit sperm movement within it (Thieme) |
|
|
Penis
a. Arterial supply b. Venous drainage c. Innervation d. Lymphatic drainage |

a. Arterial supply - 3 paired from internal pudendal arteries
1. The posterior\dorsal artery of penis (Deep to the fascia on the dorsum, -> glands, foreskin, skin) 2. The deep artery of penis (Within corpora cavernosa, -> helicine arteries) 3. The artery of bulb of penis (-> corpus spongiosum, male urethra) b. Venous drainage 1. Superficial dorsal vein of penis 2. Deep dorsal vein of penis 1-2 -> Prostatic and vesical venous plexuses (1-2 unpaired) c. Innervation 1. Sensory innervation - pudendal nerve 2. Autonomic - inferior hypogastric nerve plexus I. Sympathetic - from lumbar part of the sympathetic part (The center for the ejaculation reflex is located at L2-3. Orgasm include emission (internal) and ejaculation (external)). II. Parasympathetic part - from sacral part of the parasympathetic part (pelvic splanchnic nerves) d. Lymphatic drainage Inguinal nodes (Thieme) |
|
|
The penis
a. Epithelium of the urethra b. Glands of urethra - name, secretion c. Bulbo-urethral glands - location, location of excretory duct, secretion |
a. Epithelium
1. -> Middle of prostatic urethra - transitional epithelium 2. Middle of prostatic urethra->Navicular fossa - stratified, columnar epithelium 3. From navicular fossa - stratified, suqamous epithelium b. Urethral\Littre's glands - mucus c. Bulbuorethral glands I. In urogenital diaphragm II. Into proximal part of spongy urethra III. Stringy, mucus, slightly alkaine (Two, pea-sized) (Thieme) |
|
|
Female reproductive organs
a. Internal female genital organs b. External female genital organs c. Vulva c. Adnexa - synonym, components |
a. Internal female genital organs
1. Ovary 2. Uterine tube 3. Uterus 4. Vagina b. External female genital organs 1. Labium majus 2. Labium minus 3. Vestibule of vagina 4. Vestibular glands 5. Clitoris c. Vulva External genitalia plus urethral orifices and mons pubis. c. Adnexa\Accessory genital organs 1. Uterine tubes 2. Ovaries (Thieme) |
|
|
The female reproductive organs
a. The rectouterine fold - where, contain b. The ovary - size c. The ovary - location |
a. The rectouterine fold
I. Sacrouterine ligament and inferior hypogastric nerve plexus II. Form lateral borders of rectouterine puch of Douglas (Lowest part of peritoneum in females) b. 4 cm long x 1.5-2 cm wide c. The ovarian fossa I. A depression in parietal peritoneum of pelvis II. Bounded in front by occluded part of umbilical artery, bounded posteriorly by the ureter and the uterine vessels (Claudius fossa) |
|
|
Eponyms
a. Rectovesical pouch b. (Deep) perineal fascia c. Urethral glands of female d. Preputial glands |
a. Proust space
b. Gallaudet's fascia (Fascia that intimately invests the superficial perineal muscles (ischiocavernosus, bulbospongiosus, and superficial transverse perineal muscles); anteriorly it is fused to the suspensory ligament of the penis/clitoris, and is continuous with the deep fascia covering the external oblique muscle of the abdomen and the rectus sheath.) c. Skene glands with paraurethral Skene's ducts (Numerous mucous glands in the wall of the female urethra. Paraurethral ducts: inconstant ducts along the side of the female urethra that convey the mucoid secretion of Skene glands to the vestibule.) d. Tyson glands (Sebaceous glands of the corona and neck of the glans penis, produce an odoriferous substance called smegma.) (Netter, Stedman) |
|
|
The ovary
a. Relation to peritoneum b. Name of the superior and inferior pole c. Attachments d. Histology |
a. Intraperitoneally by the mesovarium.
(The mesovarium is connected posteriorly to the broad ligament of uterus, connected to the hilum of the ovary with the entry of the vessels and nerves). b. Superior pole = tubal extremity, inferior pole = uterine extremity. c. Attachments 1. Mesovarium - fold of peritoneum from posterior surface of broad ligament. 2. The suspensory ligament of ovary I. Band of peritoneum that pass upward from the tubal extremity II. Contain the ovarian vessels and ovarian plexus of nerves (Clado band) 3. The ligament of ovary I. Uterine extremity of ovary -> tubal angle of uterus II. d. Histology 1. Surrounding tunica albuginea I. Internal epithelial layer of cuboidal cells, erroneously referred to as the germinal epithelium (Role: replenish the surface after ovulation) 2. Ovarian stroma I. Ovarian cortex - ovarian follicles, corpus luteum and its remnants (500 000-1 000 000 primordial follicles at birth) II. Ovarian medulla - blood vessels, nerve fibers, Hilar cells (endocrine cells, similarities to Leydig cells) (Thieme) |
|
|
Ovarian follicles
a. Size of the oocyte b. Primordial follicle c. Primary follicle d. Secondary follicle |
a. Can reach up to 150 um during follicular maturation.
b. Primordial follicle The primordial oocyte is surrounded by a single layer of squamous follicular cells. c. Primary follicle I. The primary oocyte is surrounded by a ring consisting of a single layer of cuboidal follicular epithelium II. Zona pellucida (Extracellular coat, rich in glycoprotein, contain microvilli of oocyte) d. Secondary follicle\Vesicular ovarian follicle\Graafian follicle I. Oocyte surrounded by a ring of stratified follicular\granulosa epithelial cells II. Follicular fluid between adjacent follicular cells. III. Theca ('capsule') interna - steroid-producing cells IV. Theca externa - contractile cells e. Tertiary\Graafian follicle I. Follicular antrum II. Oocyte to one side in cumulus ('collection') oophorus with a 'collection' of follicular cells III. Corona radiata - the granulosa cells touching the oocyte. IV. Granular layer - the stratified epithelium lining the antrum (Granulosa cells = Follicular epithelial cells, become a luteal cell of corpus luteum after ovulation) (Thieme, Stedman) |
|
|
The ovary
a. What is released on ovulation b. What happens with the Graafian\Tertiary follicle |
a. The oocyte with its corona radiata and zona pellucida.
b. Graafian follicle -> Corpus rubrum -> Corpus luteum I. Cells of granular layer -> granulosa lutein cells II. Cells of theca interna -> theca lutein cells (-> Corpus albicans (Scar tissue)\-> Corpus luteum of pregnancy) (Thieme) |
|
|
Uterine tubes
a. Synonym b. Parts c. Relation to peritoneum d. Histology |
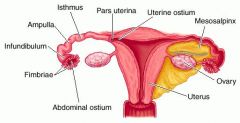
a. Uterine tubes\Salpinx\Fallopian tube
b. Parts 1. abdominal ostium 2. Infundibulum ('funnel') I. Fibriae (Ovarian fimbria is especially long, and attached to the ovary) 3. Ampulla (Lateral 2\3 of the uterine tube) 4. Isthmus (The narrow part closer to the uterus) 5. Intramural part c. Relation to peritoneum - intraperitoneal by mesosalpinx (Part of broad ligament) d. Histology 1. Mucosa I. Simple ciliated columnar epithelium, with glandular cells 2. Muscular layer I. Subperitoneal layer II. Perivascular layer III. Autochthonus muscles of the tube itself 3. Serosa (Thieme) |
|
|
Ovary and uterine tube
a. Arterial supply b. Venous drainage c. Innervation d. Lymphatic drainage |
a. Arterial supply
Ovary 1. Abdominal aorta -> ovarian artery 2. Uterine artery -> ovarian branch Uterine tube - anastomosing branches of ovarian and uterine arteries b. Venous drainage Ovarian plexus -> ovarian vein (Left ovarian vein in left renal vein, right ovarian vein in IVC) Uterine venous plexus -> ovarian, uterine veins c. Innervation Sympathetic - superior meseneric nerve plexus and renal nerve plexus Parasympathetic - inferior hypogastric plexus -> uterovaginal nerve plexus d. Lymphatic drainage Ovary -> lumbar nodes Uterine tube -> Lumbar nodes, Internal iliac nodes (Part of venous drainage via uterine veins) (Thieme) |
|
|
The uterus
a. Parts b. The cervical canal - mucosal characteristics c. Position of the uterus |
a. Parts
1. Body I. Fundus II. Left and right uterine horns III. Isthmus (The narrow portion at the junction of the uterus and the cervix) 2. Cervix - lower 1\3 I. Vaginal part - external os (anterior and posterior lips) II. Supravaginal part - internal os b. The cervical canal I. Palmate folds (Anterior and posterior, longitudinal, numerous rugae\secondary folds branch off) II. Cervical glands - mucus b. Position I. Anteversion (When the urinary bladder is empty, = the whole body of uterus is tilted forward) II. Anteflexion (Can go up to epigastrium during pregnancy) (Thieme) |
|
|
Uterus - layers of the uterine wall
|
a. Layers of the uterine wall
1. Endometrium - mucosa I. Simple ciliated columnar II. Tubular uterine glands III. Can be divided into functional layer with spongy layer (part with tubular glands) and compact layer (next to lumen, large epithelioid stromal cells appear) which undergo cyclic changes and basal layer which don't. 2. Myometrium - 3 layers, the middle are the best developed 3. Outer layer I. Serosa\Perimetrium at part of body and fundus II. Parametrium and paracervix- CT along lateral borders |
|
|
Uterus
a. Microanatomy of the cervical wall b. Epithelium of the vaginal part of the cervix c. Arterial supply d. Venous drainage e. Lymphatic drainage |
a. Cervix of uterus
I. Columnar epithelium overlies a layer of fibrocellular connective tissue. -> Don't undergo cyclic degeneration. II. cervical glands - branching tubular, alkaline mucus b. Vaginal part of cervix Stratified, nonkeratinized squamous epithelium. (Transformation zone from vaginal to uterine epithelium, visible by colposcopy, most common site of cervical carcinoma) c. Arterial supply 1. Internal iliac artery -> Uterine artery -> ascending main branch (-> ovarian branch, tubular branch), descending vaginal artery (Reach uterus via subperitoneal CT and base of broad ligament, cross over the ureter) d. Venous drainage Uterine plexus -> uterine veins -> internal iliac veins e. Lymphatic drainage Body and fundus -> 1. Lymph nodes along the aorta via the suspensory ligament of ovary 2. Superficial inguinal nodes via the round ligament of uterus 3. Lymph nodes along the division of the common iliac artery via the broad ligament of uterus Cervix -> 1. Lymph nodes along the division of the common iliac artery 2. Parietal lymph nodes along the internal iliac artery 3. Sacral nodes (All via broad ligament) (Thieme) (Thieme) |
|
|
Uterus
a. Innervation b. Support |
a. Innervation
Hypogastric nerve (sympathetic), Pelvic splanchnic nerves (parasympathetic) -> inferior hypogastric plexus -> uterovaginal plexus (Large Frankenhauser's ganglion) b. Support 1. The round ligament of uterus I. <- Area around uterine horns -> inguinal canal -> labia majora II. Has smooth muscle III. Derived from the gonadal fold IV. Continuation of the suspensory ligament of ovary 2. The broad ligament of uterus I. Peritoneal fold II. Lateral pelvic wall -> lateral margin of uterus 3. The rectouterine fold\ligament \ Sacrouterine ligament I. Peritoneal fold II. Bounding the rectouterine pouch of Douglas III. Contain inferior hypogastric nerve plexus (Some sources says it contains the smooth rectouterinus muscle) 4. Cardinal\Mackenrodt's ligament I. Condensation of CT that fix the cervix to the lateral wall. (However, its mainly supported by the pelvic floor muscles) (Thieme) |
|
|
Vagina
a. Vaginal fornix b. Mucosal landmarks c. Histology d. Source of vaginal fluid |
a. Vaginal fornix
I. The recess at the vault of the vagina II. Posterior (deepest, extend to rectouterine pouch), anterior, and lateral b. Mucosal landmarks I. Vaginal rugae - transverse II. Caginal columns - longitudinally (<- Underlying venous plexuses. The anterior vagal column is continuous with the urethral carina of vagina) c. Histology 1. Mucosa I. Stratified, nonkeratinized epithelium (Glycogen-rich) II. Lamina propria mucosae 2. Muscular layer I. Meshwork of smooth muscle and elastic fibrers 3. Adventitia - paracolpium d. Vaginal fluid 1. Transudate from venous plexuses 2. Cervical secretions 3. Exfoliated epithelial cells (Low pH of 4-4.5 from lactic acid production by lactic acid bacteria from glycogen in exfoliated epithelial cells) (Thieme) |
|
|
Vagina
a. Arterial supply b. Venous drainage c. Innervation d. Lymphatic drainage |
a. Arterial supply - vaginal branches of
1. Uterine artery 2. Inferior vesical artery 3. Internal pudendal artery b. Venous drainage Vaginal venous plexus -> internal iliac veins c. Innervation Hypogastric nerve (sympathetic), pelvic splanchnic nerves (parasympathetic) -> Uterovaginal nerve plexus The inferior parts of the vagina are innervated by the pudendal nerve. d. Lymphatic drainage 1. External and internal iliac nodes 2. Superficial inguinal nodes (Thieme) |
|
|
External female genitalia
a. Labia majora b. Bulb of vestibule c. Labia minora - connections anteriorly and posteriorly d. Labia minora - covering\skin |
a. Labia majora
I. Fat pads and venous plexuses covered by skin II. Exterior skin - pigmented skin, hair, sebaceous, sweat glands III. Inner skin - poorly keratinized, sebaceous glands b. Bulb of vestibule I. Mass of erectile tissue on either side of the vagina, united anteriorly by the commissure of bulbs II. Covered by bulbospongiosus (Corresponds to male corpus spongiosum) c. Labia minora I. Posteriorly -> frenulum of labia minora II. Anteriorly -> two folds: frenulum of clitoris, prepuce of clitoris d. Labia minora I. Thin epidermis II. Sebaceous glands |
|
|
External female genitalia
a. Glands b. Clitoris - parts c. Arterial supply d. Venous drainage e. Innervation f. Lymphatid drainage |
a. Glands
1. Greater vestibular glands\Bartholin's glands I. On either side of the vaginal orifice at the termination of the vestibular bulbs. II. Open into vestibule of the vagina 2. Lesser vestibular glands I. In vestibule II. Mucoid discharge b. Clitoris 1. Crus of clitoris - left and right corpora cavernosa of clitoris (Arise from inferior pubic rami) (Covered by ischiocavernosus) 2. Body of clitoris (Suspensory ligament) 3. Glans of clitoris c. Arterial supply 1. Terminal branch of internal pudendal artery d. Venous drainage 1. Internal pudendal vein 2. External pudendal veins 3. Vesical venous plexus -> deep posterior vein of clitoris e. Innervation - branches of 1. Pudendal nerve 2. Ilioinguinal nerve 3. Genitofemoral nerve f. Lymphatic drainage - inguinal nodes (Thieme) |
|
|
Pelvis
a. Pelvic floor\diaphragm b. Ischioanal fossa - borders c. Ischioanal fossa - content d. Urogenital diaphragm |
a. Pelvic diaphragm\floor
Fascia above and below (Superior and inferior fascia of pelvic diaphragm) I. Pubococcygeus II. Iliococcygeus III. Puborectalis (Sling around rectum at anorectal flexure) 2. Ischiococcygeus (Ischial spine -> coccyx\sacrum) b. Ischioanal fossa 1. Medially I. External anal sphincter I. Levator ani (The inferior fascia of the pelvic diaphragm) 2. Laterally I. Ischial tuberosity II. Obturator fascia 3. Posterior I. Gluteus maximus II. Sacrotuberous ligament 4. Anterior - posterior border of urogenital diaphragm (Pyramid with apex near the union of letavor ani and obturator internus, base at perineal skin) c. Ischioanal fossa I. Fat body of ischioanal fossa II. Internal pudendal vessels and pdeudenal nerve in Alcock's canal in the the obturator internus fascia (Lateral wall of ischioanal fossa) d. Urogenital diaphragm 1. Superior fascia 2. Deep transverse perineal muscle and sphincter urethrae 3. Perineal membrane (The muscle-containing space between the fascia were previously referred to as the deep perineal space. These terms are not recognized by terminologica anatomica) (Thieme) |
|
|
Uterus - variations
|
1. Retroversion
I. 1-3 degree - altered rectal contour in 3rd degree 2. Retroflexion 3. Retrocession (Denoting a position of the uterus or other organ farther back than is normal.) 4. Severe anteflexion (Netter) |
|
|
Fascial layers of pelvis\perineum
a. Dartos fascia - what, what does it cover, which layers are it continuous with b. Colles fascia - what, what does it cover, which layers are it continuous with c. Buck's fascia - what, what does it cover, which layers are it continuous with d. Gallaudet's fascia - what, what does it cover, which layers are it continuous with |
a. Dartos fascia\Superficial fascia of scrotum
I. Superficial fascia in scrotum, have smooth muscle II. Colles fascia in perineum, Scarpa's fascia in abdomen b. Colles fascia\Subcutaneous tissue of perineum I. Dartos fascia above at scrotum, Scarpa's fascia above at abdomen, fascia lata of thigh c. Buck's fascia\(Deep) fascia of penis I. Surrounds the erectile bodies of the penis II. Continuous with aponeurosis of external oblique\anterior rectal sheath d. Gallaudet's fascia\(Deep) perineal fascia I. Fascia that intimately invests the superficial perineal muscles - ischiocavernosus, bulbospongiosus, superficial transverse perineal II. Continuous with suspensory ligament of penis, Buck's fascia, deep fascia covering external oblique and the anterior rectus sheath. (Stedman) |
|
|
Innervation of pelvic viscera in relation to parturition - list the three pathways pain can travel via with parturition
|
1. Pain from intraperitoneal pelvic viscera - fundus, body of uteurs
(Ie uterine contraction) I. Uterovaginal and pelvic plexuses -> II. Hypogastric nerves -> III. Superior hypogastric plexus -> IV. Lower aortic plexus -> V. Lower lumbar splanchnic nerves -> VI. Sympathetic trunk L4-L5 -> VII. Spinal nerves T11-12 2. Pain from subperitoneal pelvic viscera - cervix, upper vagina (Ie cervical dilation) I. Pelvic splanchnic nerves to S2-S4 3. Pain from lower vagina and perineum I. Pudendal nerve -> S2-S4 (Netter) |

