![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
110 Cards in this Set
- Front
- Back
- 3rd side (hint)
|
5 basic functions of respiratory system |
Extensive area for gas exchange. Regulation of blood pH. Producing speech sounds and providing olfactory sensations. Protection of respiratory system. |
|
|
|
How is speech produced by the respiratory system? |
Movement of air over the vocal cords. |
|
|
|
Why does the respiratory system need protection? |
It is the perfect environment for bacteria. The air in there is moist and has a constant supply of oxygen. |
|
|
|
What is the bypass of the respiratory system and why is it needed? |
A person can breathe through their mouth. It acts as compensation when illness makes nose breathing difficult. |
|
|
|
What makes up the upper airways? |
The nose, nasal passageway and the pharynx. |
|
|
|
What is the purpose of the nose and nasal passageways? |
It is the primary air passage way. Its shape allows control of our passage. It is the beginning of respiratory defence. |
|
|
|
What is the structure of the nose and the nasal passageway? |
It consists of bone and cartilage, covered by connective tissue and skin. This acts as a form of protection. The nose is filled with cilia and mucus. They filter warm/humidifies the air (in preparationfor the lower respiratory system) and filter/catch particles in the air. |
|
|
|
What is the pharynx and its purpose? |
This is the connection between the digestive and respiratory system. It is designed so air and food can pass through. |
|
|
|
What are the lower airways? |
The larynx, trachea, lungs and bronchi. |
|
|
|
What is the larynx and its structure? |
It is where the vocal cords are located. It contains no bones, only cartilage (for flexibility and protection). A decrease in cartilage and an increase in smooth muscle as you move down (this gives involuntary control for constriction and dilation for controlling air). It leads to the trachea. |
|
|
|
What is the trachea also caned and what is it attached to? |
The trachea is the windpipe. It extends from the larynx to the primary bronchi, where it splits into the left and right primary bronchi. |
|
|
|
What is the structure of the trachea? |
It is made of connective tissue and smooth muscle and is reinforced by C-shaped rings of cartilage. The cartilage rings act as protection and allows movement when the heart moves/food is swallowed ao also enables reduction/increase in air volume. |
|
|
|
Purpose of the vast amount of cilia and goblet cells in the trachea? |
The goblet cells produce mucus. the cilia in moves the mucus upwards to be swallowed. This creates a mucus-cilia elevator, if this breaks down there is no protection for the respiratory system. |
|
|
|
what is the structure of the bronchi? |
It is made of smooth muscle (for volume intake). The right bronchus is larger (most blockages occur here). There are 3 levels: primary,secondary and tertiary bronchi. The walls contain progressively less cartilage (decrease in cartilage = increase in smooth muscle). |
|
|
|
What is the bronchial tree? |
Where airways enter the lungs primary bronchi their branches form a bronchial tree. |
|
|
|
What is the anatomy of the thorax? |
It is bounded at the neck with the spinal column, ribs and sternum making up the wall (also contains lots of connective tissue with elastic properties). It is separated from the abdomen by the diaphragm. |
|
|
|
What is the pleural sac? |
It is a serous membrane that is double-folded. It contains the lungs (and associated membranes) and it is contained in the thorax. |
|
|
|
What is the pleura? |
The pair of serous membranes in the thorax that envelop the lungs. They are known as the pleural cavities. |
|
|
|
What separates the 2 pleural cavities? |
The mediastinum, a bundle of connective tissue. |
|
|
|
What is the anatomy of the pleura? |
Each lung occupies a single pleura. The consist of 2 layers : the parietal pleura and visceral pleura(both secrete pleural fluid). |
|
|
|
What is the parietal pleura? |
It covers the inner surface of the thoraic wall. |
|
|
|
What is the visceral pleura? |
It covers the outer surfaces of the lungs and extend into fissures between lobes. |
|
|
|
What is the purpose of the pleura? |
It encases and protects the lungs (from expansion) and also allows a reduction of pressure. |
|
|
|
What is the term for the disease state of the pleura? |
Pleurisy. |
|
|
|
How many lobes does the right lung have? |
3 |
|
|
|
How many lobes does the left lung have? |
2. |
|
|
|
What is the bronchial tree? |
The branching system of bronchi and bronchioles, conducting air from the trachea to re alveoli. |
|
|
|
The lungs are protected by the pleural sac and are pressurised. |
Blank. |
|
|
|
What is the conducing zone? |
The low resistance pathway that transports and prepares air for gas exchange. It is also where respiratory defence occurs. NO GAS EXCHANGE OCCURS HERE. |
|
|
|
What does the conducting zone consist of? |
The nasal cavity, trachea, bronchi, bronchioles and terminal bronchioles. |
|
|
|
What leads to scar tissue formation in the lungs and why is this detrimental? |
Infection in the lung. Scar tissue does not function (other than for protection). |
|
|
|
What is the respiratory zone? |
The site of gas exchange. |
|
|
|
What does the respiratory zone contain? |
Respiratoy bronchiole ( connected to individual alveoli), alveolar ducts, alveolar sacs (which contain alveoli). |
|
|
|
What is the structure of alveoli? |
The alveolar walls contain capillaries and very small intestinal spaces, the blood is seperate from air within the alveolus by an extremely thin barrier (0.2 micrometres). There are approximately 300 million in the lungs and their total surface area is the size of a tennis court. This makes them specialised for rapid gas exchange. |
|
|
|
What do alveoli contain? |
Type 1 alveolar cells, type 2 alveolar cells and alveolar macrophages. |
|
|
|
What are type 1 alveolar cells? |
Flat squamous epithelial cells that make up 95% of the alveolar surface. They allow rapid gas diffusion. These cells are liable to damage but can repair to a point. |
|
|
|
What are type 2 alveolar cells? |
Cuboidal septal cells. They are scattered between type 2 cells and make up 5% of the alveolar surface. They Have a main functions: produce surfactant and repair alveolar epithelium (type I cells). |
|
|
|
What is the purpose of alveolar macrophages? |
Also known as dust cells. They are the last line of defence and engulf anything that shouldn't be there. |
|
|
|
What is surfactant? |
It is a phospholipid that coats the alveoli. It reduces surface tension and prevent alveoli collapse during exhalation (allowing lungs to expand). Without it surface tension would be 10X greater. |
|
|
|
What is Infant Respiratory Distress Syndrome (IRDS)? |
Premature (before 8 months) babies lungs lack sufficient surfactant, as it is not produced until 8 months in foetal life. This results in alveoli collapse. |
|
|
|
What are the main respiratory defences? |
The nasal cavity warms/fiIters air. Mucous escalator. The structure of the respiratory epithelium changes throughout respiratory tract. Alveolar macrophages. |
|
|
|
Why must the pharyngeal epithelium must protect itself? |
It must protect itself from abrasion and chemical attack as the pharyna must conduct air to the larynx and convey food to the oesophagus. |
|
|
|
What causes a breakdown of respiratory defence? |
The presence of irritants (cigarette smoke). Aggressive pathogens (tuberculosis). Inherited congenital defects that affect mucus production/transport ( cystic fibrosis). |
|
|
|
What is pulmonary ventilation? |
It is the physical movement of air into and out of the respiratory tract, that is to maintain alveolar ventilation to ensure a suppy continuous of oxygen. |
|
|
|
What are the 2 phases of ventilation and what causes them? |
Inhalation (Inspiration) and exhalation (expiration). Ventilation is driven by changes in volume, which result in a pressure change. |
|
|
|
What are the main rules regarding volume and pressure change? |
A change in volume causes a change in pressure. A larger volume results in a lower pressure, while a smaller volume results in a higher pressure. Air will flow from high to low pressure. |
|
|
|
How is volume and pressure changed during ventilation and why is it important? |
Muscles of respiration charge thoracic volume and thus pressure. Air flow from outside the body into the alveoli is due to pressure differences. |
|
|
|
What pressures are important in ventilation? |
Atmospheric pressure (Patm). Alveolar (interpumonay) pressure (Palv). Intra peral pressure (Pip). Transpulmonary pressure (Pip). |
|
|
|
What is atmospheric pressure (Patm)? |
Pressure exerted by weight of gas in atmosphere on Objects on earth surface (760mmHg, sometimes described as 0mmHg). |
|
|
|
What is alveolar (intrapulmonary) pressure (Palv)? |
Pressure inside respiratory tract (at alveoli), normal breathing difference is very small. |
|
|
|
What is intrapleural pressure (Pip)? |
Pressure within the pleural sac (in the space between parietal and visceral pleura). Usually less than atmospheric pressure (normally -6mmHg but can reach -18mmHg during powerful inhalation) |
|
|
|
What is transpulmonary pressure (Ptp)? |
The differences in pressure. Ptp = Palv - Pip. |
|
|
|
What is Boyles Law? |
Pressure of a gas is inversely proportional to its volume. |
|
|
|
How does Boyles law relate to the respiratory system? |
Pressure changes result from charges in dimension of chest wall and lungs. In smaller spaces the particles suffer more collisions with the container's walls. |
|
|
|
What pressure changes cause inhalation? |
Alveolar pressure (Palv) < Atmospheric pressure (Patm). The driving force fo air flow is negative. Air flows inwards. |
|
|
|
What pressure changes occur in exhalation? |
Alveolar pressure (Palv) > Atmospheric pressure (Patm). Driving force for air flow is positive. Air flows outward. |
|
|
|
What is lung compliance? |
A measure on how easily the lungs expands and contracts. Low compliance means a greater force is required to fill/empty the lungs. High compliance means it is easier to expand the lungs ax given change in transpulmonary pressure. |
|
|
|
What factors affect lung compliance? |
Connective tissue structure of the lungs. Level of surfactant production. Mobility of thoracic cage. |
|
|
|
How does connective tissue structure affect lung compliance andwhaatisdislase state associated with it? |
Loss or supporting tissue resulting from alveolar damage increases compliance. Emphysema. |
|
|
|
How does level of surfactant production affect long compliance and what disease state can be associated with it? |
Collapse of alveoli on exhalation is prevented by surfactant. Inadequate surfactant reduces compliance. IRDS. |
|
|
|
How does mobility of the thoracic cage affect lung compliance and what disease state can be associated? |
Reduction of compliance can result from any disorder affecting articulations of ribs/spinal column. Arthritis. |
|
|
|
What is the respiration cycle? |
An inhalation followed by an exhalation. There are 10-15 respiratory cycles per minute. |
|
|
|
How much air enters the lungs per min and how much blood flows through the pulmonary capillaries at rest and during exercise in normal adults? |
At rest, ~4L fresh air enters the lungs per min and 5L of blood flows through the pulmonary capillaries. During heavy exercise airflow increases by ×20 and blood flow increases by ×5. |
|
|
|
What triggers breathing ? |
The most important trigger is proton concentration in cerebral fluid. The second most important one is PCO2 (partial pressure of carbon dioxide) in the body. Oxygen needs is the third most important trigger. |
|
|
|
During a normal inhalation, how much air is breathed in at rest? |
500ml. |
|
|
|
What are the mechanisms of inhalation? |
The chest expands. The ribs more out (inspiratoy intercoastal muscles contract) and the diaphragm contracts. The thorax expands. Pip becomes more sub atmospheric (transpulmonary pressure increases). Lungs expand. Palv becomes sub atmospheric. Air flows into the alveoli. |
|
|
|
What is the mechanism of exhalation? |
The diaphragm and me inspiratory intercoastal muscles relax. The chest wail recoils inward. Trans pulmonary pressure moves back towards pre-inspiration valve. Lungs recoil to pre-inspiration size. Air in alveoli becomes compressed. Palv becomes greater than Patm. Air flows out of the lungs. |
|
|
|
What are in muscles of inhalation and when are they used? |
They are the intercoastal muscles. There are 2 types: inspiratory (internal) and expiratory (external). They are the accessory muscles. Inspiratory one used during normal breathing and expiratory are used during forced breathing. on |
|
|
|
What are the pressure changes in normal breathing (inhalation)? |
(Indicated as mmHg below / above -760mmHg) Alveolar = -3 , Intrapleural = -6. Transpulmonary = +3. |
|
|
|
what are the pressure changes in normal breathing (exhalation)? |
(Indicated as below or above -760mmHg. Alveolar = +3. lnlrapieural = -3. Transpulmonary = +6. |
|
|
|
What are the aeessory muscles of inspiration and there purpose? |
Sternocleidomastoid, elevates the sternum. Scalenes group, elevate the upper ribs. Pectoralis minor. |
|
|
|
What are the principle muscles of inspiration and their purpose? |
External intercoasts and interchondral part of internal intercoasts elevate the ribs. Diaphragm done descends to increase the vertical dimension of the thoracic cavity and elevates the lower ribs. |
|
|
|
What are the muscles of expiration in normal (quiet) breathing? |
Expiration resvts from passive, elastic recoil of the lungs, rib cage and diaphragm. |
|
|
|
What are the muscles of expiration in active breathing? |
Internal intercoastals (except intvchondrai part) pull the ribs down. Abdominal, pull the ribs down and compress abdominal contents (thus pushing diaphragm upwards).Quadratus lumborum, pulls the ribs down. |
|
|
|
What are lung volumes? |
Tidal volume (TV), Inspiratoy reserve volume (IRV), Expiratory reserve volume (ERV) and Residual volume (RV). |
|
|
|
What are lung capacities? |
Functional residual capacity (FRC), vital capacity (VC) and Total lung capacity (TLC). |
|
|
|
What is tidal volume? |
The volume of air inspired) expired with each breath. ~500ml. |
|
|
|
What is inspiratory reserve volume? |
The volume of air forcefully inspired. ~ 3000mI. |
|
|
|
What is residual volume? |
The volume of air remaining in the lungs after maximal expiration. ~ 1200ml. |
|
|
|
What is functional residual capacity? |
ERV + RV . It is the volume of air remaining in lungs after normal expiration. ~2400ml |
|
|
|
What is vital capacity? |
IRV + TV + ERV. It is the maximum volume of air that a person can expel after maximum inspiration. ~4700ml. |
|
|
|
What factors make gas exchange efficient? |
A small distance between capillaries and lungs. Requires a concentration gradient for rapid transfer. A difference in partial pressures, as it is difficult for gas to pass into solution. |
|
|
|
Why does infection in the lungs make gas exchange inefficient? |
Inflammation makes the distance too large for gases to transfer over. |
|
|
|
Where does gas exchange occur in the body? |
Pulmonary ventilation ensures cells supplied with oxygen and removes carbon dioxide arriving from the bloodstream. Gas exchange occurs between the blood and alveolar air across respiratory membrane. |
|
|
|
What gases do we breathe in? |
Nitrogen, oxygen, water vapour and carbon dioxide. |
|
|
|
What is atmospheric pressure? |
It represents the combined effects of collisions of all gas molecules in the air. |
|
|
|
What is the partial pressure of a gas (P)? |
It is the pressure of a gas' contribution to pressure in a mixture of gases. It is directly proportional to the gas' concentration. All partial pressures added together equal the total pressure exerted by a gas mixture. |
|
|
|
What causes diffusion in partial pressure of gases? |
Net diffusion occurs from high to low partial pressures and is affected by temperature. |
|
|
|
Describe Daltons law |
Each gas contributes to total pressure in proportion to its relative abundance. |
|
|
|
What causes diffusion between liquids and gases? |
When under pressure, gas molecules to move into a solution. At equilibrium, gas molecules into/out of a liquid at the same rate (gases like to be at equilibrium but a difference is required for gas exchange). |
|
|
|
Describe Henrys Law. |
At a given temperature the amount of a particular gas in solution is directly proportional to its partial pressure (higher temperature means gas moves out of the solution more easily. |
|
|
|
What determines actual amount of gas in solution? |
Solubility of a gas in a particular liquid at a given temperature and pressure. Dissolved gas content is reported as mI gas per 100ml (1dl). |
|
|
|
What are the solubility of oxygen, nitrogen and carbon dioxide in the body fluids? |
Carbon dioxide is very soluble, oxygen is less soluble and nitrogen has limited solubility. |
|
|
|
What is decompression sickness (the bends)? |
High sea pressures forces nitrogen to move into solution into the body fluids. When the body depressurises (when moving quickly to lower pressures) it causes the dissolved gas to come out of solution to create bubbles in the body. |
|
|
|
Describe factors of normal diffusion at respiratory membranes. |
There is a substantial difference in partial pressure across the respiratory membrane. Gases are lipid soluble, there is a large surface area, coordinated blood flow and airflow (these directed to certain areas of the lungs). Gas exchange occurs over small distance (averagely 0.5 micrometres). Surfactant is present. |
|
|
|
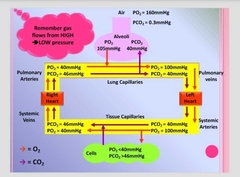
Draw a diagram of partial pressure of oxygen and carbon dioxide changes in the body. |
|
Normally blood in the lungs has a lower partial pressure of oxygen than the atmosphere and lungs, so air moves into the blood. The blood has a higher partial pressure of carbon dioxide than in the lungs so it moves out of the blood. |
|
|
What factors affect gas exchange? |
Damage to tissue or scar tissue. Cold temperatures increases membrane distance. Tumour growth reduces surface area. |
|
|
|
How are the states of oxygen and carbon dioxide changed for gas exchange? |
when inhaling, carbon dioxide mixes with gas in lungs (partial pressure of carbon dioxide increases). For gas exchange to occur, oxygen must be a gas and carbon dioxide must be liquid. Blood moves constantly so gas can't equilibrate. The blood has low oxygen so it moves from alveoli into the blood and is diluted. It also has high carbon dioxide which acts as the driving force for it to move out of solution ( the difference doesn't have to be large). |
|
|
|
Oxygen is insoluble, so how is it transported? |
Erythrocytes help carry it through haemoglobin. Haemoglobin consists of 4 haem groups (each haemoglobin unit can bind to 4 oxygen molecules . Oxyhaemoglobin). Each Erythrocyte has ~280million haemoglobin (can compensate for oxygen loss). |
|
|
|
Describe an oxygen dissociation curve . |

It is difficult to bind the first oxygen so a high pressure is required and as more oxygen birds the higher the affinity for it is. If partial pressure increases (lungs) the reaction shifts to the right and more oxygen gets bound to haem. If partial pressure of oxygen decreases (tissues) the reaction shifts to the left and more oxygen is released. |
|
|
|
What is the Bohr effect? |
A drop in pH causes a shift in the oxygen dissociation curve. As it causes the shape of Haemoglobin to change in a way that makes them well use oxygen reserves more readily. This effect is caused by primarily carbon dioxide. |
|
|
|
How does temperature effect haemoglobin saturation? |
When temperature rises haemoglobin releases more oxygen. The presence of carbon dioxide and large amounts of heat indicates metabolism occuring. |
|
|
|
What is carbon monoxide (CO) poisoning? |
CO competes with oxygen for the binding sites on haem units. It has a stronger affinity than oxygen, the bond it forms with haem is extremely durable (essentially makes the haem unit inactive for respiratory purposes). If CO molecules are 0.1% of inhaled air, human survival is impossible without medical intervention. A high partial pressure of oxygen is needed to push the CO off the haem. |
|
|
|
What methods of carbon dioxide transport are there? |
Carbon dioxide is generated by aerobic metabolism in peripheral tissues and it has an impact on blood pH. Upon entering the blood stream it is: converted to bicarbonate (70%), bound to protein portion of haemoglobin within erythrocytes (23%) or dissolved in plasma (7%). |
|
|
|
How is carbon dioxide converted into bicarbonate in the blood? |
Carbons dioxide combines with water to form carbonic acid (accelerated by carbonic annydrase). Carbonic acid is unstable so its intermediates dissociate into bicarbonate and proton. The bicarbonate is transported out of the erythrocyte into the blood's plasma in exchange for a chloride ion. In the lungs this reverses (chloride ion for bicarbonate) and the proton dissociates from the haemoglobin and binds to it forming carbonic acid. The carbonic acid quickly dissociates into carbon dioxide by carbonic anhydrase and is expelled from the lungs through exhalation. |
|
|
|
How is respiration controlled normally? |
Cellular absorption and generation rates are matched by the capillary rates of delivery/removal. |
|
|
|
How is respiration controlled when there is an imbalance? |
Homeostatic mechanisms intervene such as changes in blood flow and oxygen delivery regulation at a local level, as well as changes in rate of respiration under control of the respiratory centre. |
|
|
|
How is gas transport and alveolar function regulated locally? |
The rate of oxygen delivery and efficiency of oxygen pickup at lungs is regulated largely at a local level. Local factors (like differences in partial pressures) coordinate lung perfusion and alveolar ventilation. |
|
|
|
Describe local regulation of gas transport/alveolar function in peripheral tissues. |
If peripheral tissues become more active. In the interstitial fluid the partial pressure of oxygen reduces, while the partial pressure of carbon dioxide increases. This creates a differences between partial pressures in tissues and arriving blood, so more oxygen is delivered and more carbon dioxide is removed. |
|
|
|
Why is partial pressure of carbon dioxide need to be maintained? |
Blood pH must be 7.35 -7.45 (outside this range enzymes and proteins denature). A rise or fall in partial pressure of carbon dioxide indicates pH changes. Breathing rate changes to help control partial pressure of carbon dioxide. |
|

