![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
16 Cards in this Set
- Front
- Back
|
CN I: Olfactory
Noxious odors should not be used as these may cause pain, thereby stimulating sensory axons in which cranial nerve? |
Noxious odors may cause pain, thereby stimulating general afferent axons in the first and second divisions of the trigeminal nerve (V). |
|
|
CN II: Optic
Visual Acuity: How would you test the visual acuity of a young child, illiterate adult or an adult whose language does not use English letters?
|

Charts that do not require letter recognition are available for young children, illiterate adults or adults whose language does not use English letters. One version uses simple pictures or patterns. Others are printed with the block letter "E" turned in different orientations, the so-called Tumbling E. The patient simply indicates which direction each "E" is facing. Examples are below. |
|
|
Visual Fields: How will damage to the optic nerve differ from damage to the optic tract? |
Damage to the optic nerve will cause visual deficits in one eye, while damage to the optic tract will cause visual field deficits that are similar for both eyes. This is because half the axons in the optic nerve cross to the contralateral side in the optic chiasm. |
|
|
CNIII: Oculomotor
Pupillary Responses:
What type of axons in the oculomotor nerve are responsible for pupillary constriction?
What muscle do they innervate?
Where are the cell bodies of the axons innervating this muscle located?
What type of axons in the oculomotor nerve are responsible for accommodation?
What muscle do they innervate?
Where are the cell bodies of the axons innervating this muscle located?
What type of axons in the oculomotor nerve are responsible for keeping the eyelid elevated? What muscle do they innervate?
Where are the cell bodies of the axons innervating this muscle located?
Damage to what other innervation could result in ptosis?
What muscle do they innervate?
Where are the cell bodies of the axons innervating this muscle located?
|
General visceral efferent parasympathetic axons are responsible for pupillary constriction.
The postsynaptic parasympathetic axons innervate the sphincter pupillae muscle within the iris (smooth muscle).
The neuronal cell bodies of the axons innervating this muscle are in the ciliary ganglion.
General visceral efferent parasympathetic axons are responsible for accommodation.
The postsynaptic parasympathetic axons innervate the ciliary muscle (smooth muscle).
The neuronal cell bodies of the axons innervating this muscle are in the ciliary ganglion.
General somatic efferent axons are responsible for elevation of the eyelid.
The axons innervate the skeletal muscle of the levator palpebrae superioris.
The neuronal cell bodies of the axons innervating this muscle are in the nucleus of the oculomotor nerve.
General visceral efferent postsynaptic sympathetic axons innervate the smooth muscle within the levator palpebrae superioris that is also responsible for elevation of the eyelid.
The neuronal cell bodies of the axons innervating this muscle are in the superior cervical ganglion. |
|
|
Extraocular Movements:
Ask the patient to look to the right and observe the left eye, and then ask the patient to look to the left and examine the right eye.
What muscle is being tested?
Ask the patient to look straight up and then straight down. Observe if they can do so and whether gaze moves either laterally or medially.
What would you expect if the oculomotor nerve were damaged? |
The medial rectus is responsible for medial movement of the eyeball.
If the oculomotor nerve were damaged, the patient will not be able to look up at all since neither the inferior oblique nor the superior rectus are functional, and the eye will deviate laterally if the patient tries the look straight down since the inferior rectus is not functional but the superior oblique remains innervated. |
|
|
CN IV: Trochlear
Extraocular Movements:
Ask the patient to look straight up and then straight down. Observe if they can do so and whether gaze moves either laterally or medially.
What would you expect if the trochlear nerve were damaged? |
If the trochlear nerve were damaged, upward movement would be normal since both the inferior oblique and the superior rectus are functional; however, the eye will deviate medially if the patient tries the look straight down since the superior oblique is not functional but the inferior rectus remains innervated. |
|
|
CN VI: Abducent
Extraocular Movements:
Ask the patient to look to the right and observe the right eye, and then ask the patient to look to the left and examine the left eye.
What muscle is being tested? |
The lateral rectus is responsible for lateral movement of the eyeball. |
|
|
CN V: Trigeminal
Sensory: Ask the patient to close their eyes. Touch the patient’s forehead, cheek and jaw randomly with either a safety pin or paint brush on both the right and left sides. Ask the patient if they feel something sharp or dull.
Which divisions of the trigeminal nerve are being tested in each case?
Ask the patient to look to the right. Touch the lateral edge of the left eyeball with a Q-tip that you have spun between your fingers to a narrow point. There should be a blink reflex in both eyes.
What division of the trigeminal nerve is being tested?
What other cranial nerve is involved in the blink reflex and what is its function? |
Touching the forehead tests V1 (ophthalmic nerve), touching the cheek tests V2 (maxillary nerve) and touching the jaw tests V3 (mandibular nerve).
The blink reflex tests V1 (ophthalmic nerve).
The afferent limb of the blink reflex is the trigeminal nerve but the motor limb is the facial nerve (VII) that causes contraction of the orbicularis oculi. |
|
|
Motor:
Ask the patient to clench their teeth. Palpate and confirm contraction of the temporalis and masseter muscles.
What other muscle acts with the masseter in elevating the mandible?
Ask the patient to protract the mandible. What muscle is being tested?
|
The medial pterygoid acts with the masseter to elevate the mandible.
Bilateral contraction of the lateral pterygoid results in protraction while unilateral contraction results in movement to the contralateral side. |
|
|
CN VII: Facial
Motor:
Ask patient to smile, wrinkle their brow and show their teeth. What muscles are being tested in each case?
Ask the patient to clench their eyes tight. Attempt to open the eyes with your fingertips. What muscle is being tested?
Ask the patient to puff out their cheeks. Attempt to push in the cheeks with your fingertips. What muscle is being tested?
Would these muscles be affected equally if the facial nerve were damaged at the internal acoustic meatus and/or the stylomastoid foramen? |
Smiling – zygomaticus major (primarily)
Clenching the eyes closed – orbicularis oculi
|
|
|
Sensory: Prepare three solutions of sugar, salt and lemon juice. Place a Q-tip into each solution. taste. Is the patient able to do so? facial nerve were damaged at the internal acoustic meatus and/or the stylomastoid foramen? |
Damage to the facial nerve would result in a loss of taste only on the anterior two-thirds of the tongue. Damage to the facial nerve at the internal acoustic meatus would affect taste since these axons go through this foramen as part of the intermediate nerve of VII (nervus intermedius), but damage at the stylomastoid foramen would have no effect on taste since taste axons exit through the petrotympanic fissure or with the greater petrosal nerve through an unnamed foramen. |
|
|
What functions of the facial nerve have not been tested and what other deficits might the patient exhibit if there is facial nerve damage? |
The following functions of the facial nerve have not been tested:
-Innervation of the stylohyoid and posterior belly of the digastric (there would be weakness in the suprahyoids which may or may not be perceived)
-Innervation of the stapedius (the inability to dampen loud noises results in hyperacusis in which patients are sensitive to loud noises)
-Innervation of a portion of the skin of the external ear and external auditory meatus (some numbness may be perceived) |
|
|
CN VIII: Vestibulocochlear
Hearing:
Ask the patient to close their eyes and say “left” or “right” when the hear a sound. Place your fingers near the patient’s ears and rub them together testing each side randomly a couple of times. Ask the patient if the sound was the same in both ears or louder in one. A tuning fork will be used for the next two tests. Hold the tuning fork by its stem and hit it against your hand to start it vibrating. Place the stem of a vibrating tuning fork on top of the patient’s head in the midline and ask where they hear the sound. This is the Weber test. Patients with normal hearing will report hearing it in the midline. Place the stem of a vibrating tuning fork on the right mastoid process. This is testing bone conduction. Ask the patient to let you know as soon as they can no longer hear the sound. Then move the vibrating portion of the tuning fork just lateral to the external ear and ask if the patient can hear the tuning fork. This is called the Rinne test and is testing air conduction. Repeat on the left side. Normal individuals will hear a tone better by air conduction. Conductive hearing loss occurs if there is anything in the external or middle ear interfering with the conduction of sound such as excess ear wax, a perforated eardrum, a middle ear infection, or pathological conditions (i.e. excess bone growth, tumors). Sensorineural hearing loss results from neural defects occurring anywhere from the cochlea to the brain.
What would you anticipate in patients with a conductive hearing loss; would air or bone conduction be greater?
What about in patients with sensorineural hearing loss? |
In patients with a conductive hearing loss bone conduction is greater than air conduction, because bone conduction bypasses problems in the external or middle ear.
In patients with sensorineural hearing loss, air conduction is greater than bone conduction (as in normal hearing), however, hearing is decreased in the affected ear. |
|
|
CN IX, X: Glossopharyngeal, Vagus
Damage to the glossopharyngeal and vagus nerves would affect what phase of swallowing?
What cranial nerves would be involved if a patient had trouble with the first phase of swallowing?
in hoarseness?
Ask the patient to open their mouth. Using the flashlight and tongue depressor, ask the patient to say “Ah.”
Does the soft palate elevate symmetrically?
Paralysis of what muscle would result in asymmetrical elevation of the soft palate?
What nerve innervates this muscle?
Would the ipsilateral or contralateral nerve be affected? |
Damage to the glossopharyngeal and vagus nerves would affect the second and third phases of swallowing since these involuntary phases involve the muscles of the soft palate and pharynx.
The first phase of swallowing involves compression of the bolus of food against the soft palate and primarily involves the muscles of the tongue and soft palate.
Therefore the hypoglossal and vagus nerves would be involved if a patient had trouble with the first phase of swallowing.
The buccinator muscle (innervated by the facial nerve) plays a role in chewing by keeping the food on the occlusal surface.
Damage to the recurrent laryngeal branch of the vagus nerve results in hoarseness.
Paralysis of the levator veli palatini, innervated by the vagus nerve, would result in asymmetrical elevation of the soft palate.
If the uvula deviates to the right upon elevation of the soft palate, the left levator veli palatini is paralyzed and the left branch of the vagus nerve is affected.
Therefore, the uvula will deviate away from the affected side so the contralateral nerve is affected. |
|
|
CN XI: Spinal Accessory
What muscle is being tested when the patient turns their head to the right? |
The patient is contracting the left sternocleidomastoid when turning their head to the right. |
|
|
CN XII: Hypoglossal
Ask the patient to stick out their tongue. What muscle is being tested?
If the tongue curves to one side, is the ipsilateral or contralateral genioglossus muscle paralyzed?
|
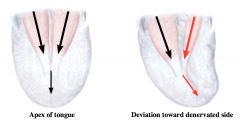
Bilateral contraction of the genioglossus muscles results in sticking out the tongue.
The line of pull of the individual genioglossus muscles is not in the midline; however, the summation of the two muscles results in the ability to stick out the tongue in the midline.
If one of the genioglossus muscles is paralyzed, the tongue will deviate toward the affected side.
Therefore the ipsilateral muscle is paralyzed.
Unilateral contraction of the ipsilateral hyoglossus and styloglossus results in moving the tongue from side to side.
The palatoglossus is innervated by the vagus nerve. |

