![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
233 Cards in this Set
- Front
- Back
|
What are the functions of cartilage?
|
"MSG"-model for bones, supports soft tissues, provides a gliding surface at articulations
|
|
|
What are the three types of cartilage connective tissue
|
Hyaline, fibrocartilage and elastic cartilage
|
|
|
What are the two growth patterns for cartilage?
|
Interstitial and appositional
|
|
|
Define interstitial growth of cartilage.
|
Interstitial growth is from within. A chondrocyte within lacuna goes through mitosis. Each cell then produces a new matrix and forms a separate lacuna.
|
|
|
Define appositional growth of cartilage
|
Appositional growth is at the edge or the perichondrium. In the perichondrium are undifferentialed stem cells that are dividing. Under the perichondrium is a new cartilage matrix that has chondroblasts secreting this matrix. Under this level is an older cartilage layer of chondrocytes. Appositional growth grows peripherally.
|
|
|
List the functions of bone.
|
Support, movement, hemopoiesis and mineral storage.
|
|
|
What are the classifications of bones by shape?
|
Long bones like the femur, short bones like the tarsal, flat bones like the frontal and irregular like the vertebra.
|
|
|
List the different parts of long bones.
|
Diaphysis, epiphysis, metaphysis, articular cartilage, medullary cavity, endosteum, periosteum, spongy bone, and epiphyseal plate.
|
|
|
What is located in the medullary cavity?
|
Yellow bone marrow comprised of fat.
|
|
|
What are the layers of the periosteum?
|
From external to deep: fibrous layer and then a cellular layer containing osteoprogenitor cells.
|
|
|
What anchors the periosteum to the bone underneath?
|
perforating fibers
|
|
|
What are the four types of lamellae?
|
circumferential, concentric, interstitial and parallel.
|
|
|
Describe the endosteum and it's location.
|
The endosteum lines the medullary cavity and has a more oval pattern than the periosteum. The matrix is called osteoid.
|
|
|
List the four type of bone cells.
|
osteoprogenitor cells that become osteoblasts that lay down the matrix. These then become osteocytes in lacuna in canaliculi. The fourth type is osteoclasts that are involved in bone reabsortion via osteolysis.
|
|
|
Describe osteoclasts.
|
A huge cell that breaks down the matrix and reabsorbs bone. It is located in Howship's lacuna and has a ruffled border. Lysosomes are residing on it.
|
|
|
Name the two types of bone.
|
spongy and compact.
|
|
|
Describe spongy bone and where it is located.
|
Called diploe and is a typical flat bone within the skull The layers are periosteum, compact bone, spongy bone, compact bone and then periosteum. It contains parallel lamellae.
|
|
|
Describe compact bone.
|
Periosteum, perforating fibers, exernal circumferential lamellae, osteons, trabeculae of spongy bone.
|
|
|
Describe an osteon.
|
Is made of concentric lamellae and has osteocytes in lacuna withing canalicui so they can connect to other osteocytes.
|
|
|
Describe trabeculae
|
Located withing spongy bone and has osteoblasts aligned along the edges. The lamellae is parallel and elongated. Contains osteocytes and osteoclasts also.
|
|
|
What are the two types of ossification?
|
Intramembranous ossification and enchondral ossification.
|
|
|
Describe intramembranous ossification.
|
Applys to flat bones only. Mesenchye tissue becomes thickened and condensed. A tissue ossification center starts to develop. Osteoblasts lay down a matrix called osteoid. Osteoid becomes hard when added to minerals. Trabeculae of woven bone is created then lamellar bone that becomes compact bone with spongy bone in the middle.
|
|
|
Describe endochondral ossification
|
The most common type and begins with a hyaline cartilage model. The cartilage calcifies and a bone collar forms around what will be the diaphysis. The perichondrium is replaced by the periosteum that lays down the bone matrix. The first site is called the primary ossification center in the diaphysis that grows distally and proximally to lengthen the shaft. Secondary ossification centers are formed at the epiphyses. The metaphysis gets smaller and then called epiphyseal plate then epiphyseal ine when we stop growing.
|
|
|
Name the zones in the epiphyseal plate.
|
Zone of resting cartilage, zone of proliferation cartilage, zone of hypertrophic cartilage, zone of calcified cartilage and zone of ossification.
|
|
|
Name the two types of bone growth.
|
Interstitial and oppositional
|
|
|
Where does interstitial bone growth occur?
|
In the epiphyseal plate as chondrocytes undergo mitosis - from within
|
|
|
Where does appositional bone growth occur?
|
Within the periosteum or on the edge.
|
|
|
What is bone remodeling?
|
Bone growth is reached, but bone continues to reshape itself in a constant process of reabsortion and deposition. Osteoblasts vs. osteoclasts. Helps maintain calcium and phosphate levels in body fluids. Occurs at periostel and endosteal surfaces of bones.
|
|
|
Name the arteries that feed bones,
|
Nutrient artery in the diaphysis, metaphyseal artery, epiphyseal artery and periosteal artery.
|
|
|
List the four types of fractures.
|
stress, pathologic, simple and compound
|
|
|
List some kinds of fractures
|
colles on the forearm, comminuted or shattered, greenstick on the collar bone, open compound that penetrates the skin and pott that is in the ankle.
|
|
|
Explain how a fracture heals.
|
A hematoma forms because a fracture bleeds. This blood is then replaced by fibrocartilage and a had bony callus forms. The bone is then remodeled.
|
|
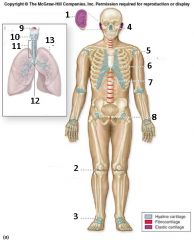
1, 2, 3
|
1. Cartilage in the external ear
2. meniscus (pad like knee joint) 3. Articular cartilage |
|
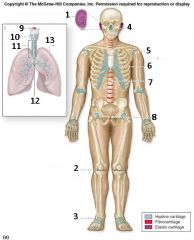
4, 5, 6
|
4. cartilages in the nose
5. articular cartilage of a joint 6. costal cartilage |
|
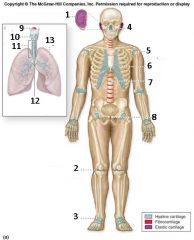
7, 8
|
7. cartilage of invertable disk
8. pubic symphisis |
|
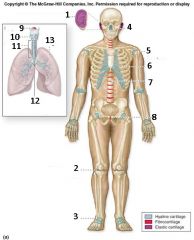
9, 10, 11
|
9. epiglottis
10. layrnx 11. trachea |
|
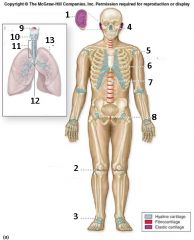
12, 13
|
12. respiratory tract cartilages on the neck, throax, lungs, trachea, and larynx
13. lung. |
|

(b), 1, 2
|
(b) hyline cartilage
1. extracellular matrix 2. lacuna (with chondrocyte) |
|

(c), 3, 4, 5
|
(c). Fibrocartilage
3. lacunae 4. extracelluar matrix 5. collagen fibers |
|

9d), 6, 7, 8
|

(d). Elastic cartilage
6. extracelluar matrix 7. elastic fibers 8. lacunae (w/ chondrocytes) |
|

1, 2, 3
|
1. Proximal epiphysis
2. metaphysis 3. diaphysis |
|

4, 5 and what bone is this?
|
4. metaphysis
5. distal epiphysis - femur |
|
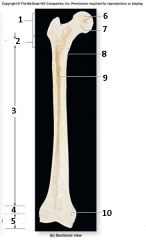
6, 7, 8
|
6. spongy bone (contains red marrow)
7. epiphyseal line 8. compact bone |
|
9, 10
|
9. Medullary cavity
10. Epiphyseal line |
|

1, 2, 3
|
1. Articualr Cartilage
2. Spongy bone 3. epiphyseal line |
|

4, 5, 6
|
4. Compact bone
5. Medullary cavity 6. Endosteum |
|

7, 8, 9
|
7. periosteum
8. perforating fibers 9. nutrient artery (through nutrient foramen) |
|
|
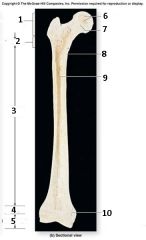
7, 8, 9
|
7. periosteum
8. perforating fibers 9. nutrient artery (through nutrient foramen) |
|

7, 8, 9
|
7. periosteum
8. perforating fibers 9. nutrient artery (through nutrient foramen) |
|

10
|
articular cartilage
|
|

11, 12
|
11. proximal epiphysis
12. Metaphysis |
|

13, 14, 15
|
13. Diaphysis
14. Metaphysis 15. Distal epiphysis |
|
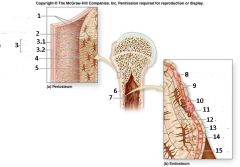
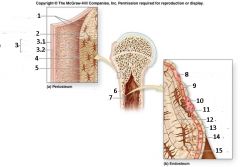
1, 2
|
1. Perforating Fibers
2. Circumferential lameliae |
|
3, 3.1, 3.2
|
3. Periosteum
3.1 Fibrous layer 3.2 Cellular layer |
|
4, 5
|
4. Canaliculi
5. Osteocyte in Lacuna |
|
6, 7
|
6. Compact bone
7. Endosteum |
|
8, 9, 10
|
8. Osteoprogenitor
9. Osteoblasts 10. Osteoclast |
|
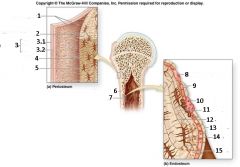
11, 12, 13
|
11. Bone Mix
12. Canaliculi 13. Endosteum |
|
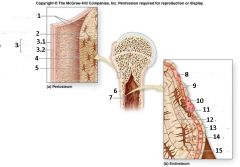
14, 15
|
14. Osteoctye in Lacuna
15. Osteoid |
|
14, 15
|
14. Osteoctye in Lacuna
15. Osteoid |
|

1, 2, 3
|
1. Nuclei
2. Lysosomes 3. Ruffled border |
|

4, 5, 6
|
4. Endosteum
5. Osteoclast 6. Howship's lacuna |
|

7, 8, 9
|
7. Osteocytes
8. Osteoblasts 9. Osteoclast |
|
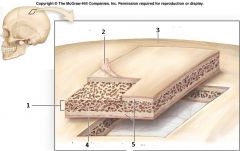
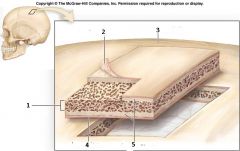
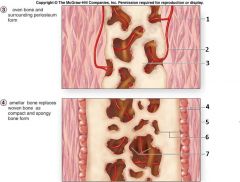
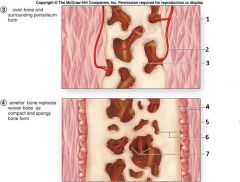
1, 2, 3
|
1. Spongy bone
2. Periosteum 3. Flat bone of skull |
|
4, 5
|
4. Periosteum
5. Compact Bone |
|
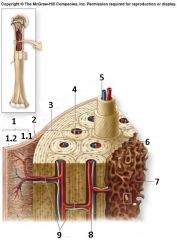
1, 1.1, 1.2
|
1. periosteum
1.1 Cellular layer 1.2 Fibrous Layer |
|
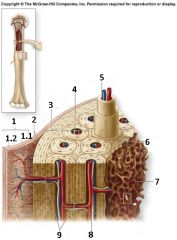
2, 3, 4, 5
|
2. Perforating Fibers
3. External circumferential 4. Osteon 5. Central Canal |
|
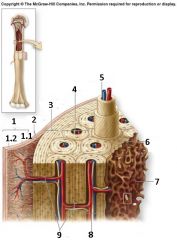
6, 7
|
6. Interstitial lamellae
7. Trabeculae of Spongy bone |
|
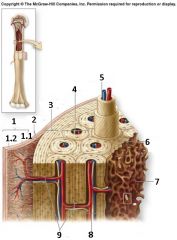
8, 9
|
8. Central canal
9. Perforating canals |
|
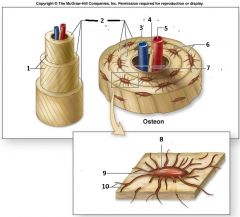
1, 2
|
1. Collagen fiber orientation
2. Concentric lamellae |
|
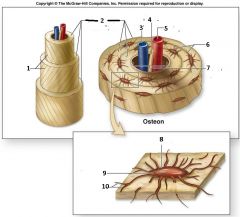
3, 4, 5
|
3. Vein
4. nerve 5. Artery |
|
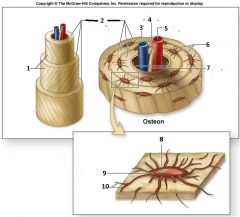
6, 7
|
6. Canaliculi
7. Central canal |
|
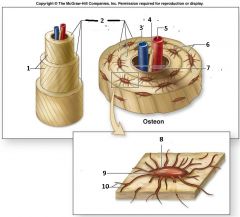
8, 9, 10
|
8. Lacuna
9. Osteocyte 10. Canaliculi |
|
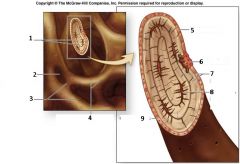
1, 2, 3, 4
|
1. Interstitial lamellae
2. Space for red bone marrow 3. trabeculae 4. Canaliculi opening |
|
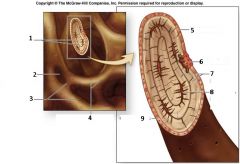
5, 6, 7, 8, 9
|
5. endosteum
6. Osteoclast 7. Parallel lamellae 8. Osteocyte in lacuna |
|
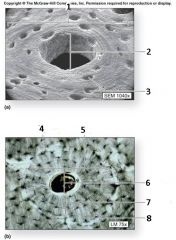
2, 3
|
2. Central canal
3. Lacunae |
|
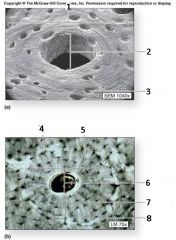
4, 5, 6, 7, 8
|
4. lacuna (w/osteocyte)
5. Osteon 6. Central Canal 7. Concentric canal 8. canaliculi |
|

1, 2
|
1. Osteoblasts
2. Spongy bone |
|

1, 2, 3, 4, 5
|
1. Collagen fiber
2. mesenchymal cell 3. ossification 4. osteoid 5. Osteoblast |
|

6, 7, 8, 9
|
6. Osteoid
7. Osteoblast 8. Osteocyte 9. Newly calcified bone matrix |
|
1, 2, 3
|
1. Mesenchyme condensing to form the periosteum
2. Blood vessel 3. Trabecula of woven bone. |
|
4, 5, 6, 7
|
4. Periosteum
5. Osteoprogenitor cell 6. Compact bone 7. Spongy bone |
|
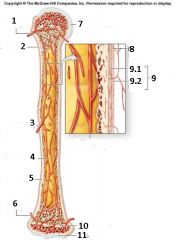
1, 2, 3
|
1. metaphyseal artery
2. periosteum 3. nutrient artery |
|
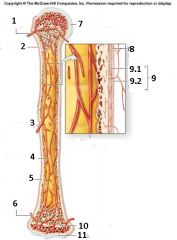
4, 5, 6
|
4. Medullary bone cavity (contains yellow bone marrow)
5. Compact bone 6. Metaphyseal artery |
|
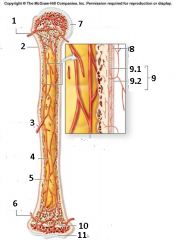
7, 10, 11
|
7. Articular cartilage
10. Epiphyseal line 11. Articular cartilage |
|
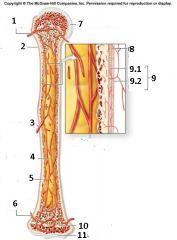
8, 9, 9.1, 9.2
|
8. periosteal arteries
9. Periosteum 9.1 cellular layer 9.2 Fibrous layer - please note unlabeled = Branch of nutrient artery |
|

name the following types of fractures in the picture
1, 2, 3, 4, 5, 6 |

|
|

1, 2
|
1. Spiral
2. Transverse |
|

identify this image
|
bone with osteoporosis
|
|
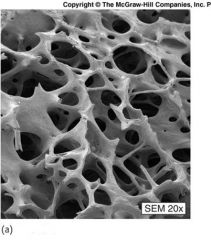
Identify this image
|
Normal bone
|
|
|
1 a. Describe the three types of cartilage. Which is most abundant? Strongest?
|
"Hyaline cartilage, Fibrocartilage, Elastic cartilage. Hyaline is the most abundant found in the joints and intercostals. Fiber cartilage is the strongest.
|
|
|
b. Why do we need more than one type?
|
each type offers a different level of flexibility or stiffness based on its function.
|
|
|
|
|
|
|
2 a. Describe the anatomy of the epiphyseal plate.
|
Epiphyseal plates are found in growing bones. They are located in the metaphysis at each end of a long bone.
|
|
|
b. Which zone is last to be replaced by bone? Why?
|
The epiphyseal plate is the last zone to be replaced by bone. It eventually gets thinner and thinner as we progreess through puberty and becomes the epiphyseal line
|
|
|
|
|
|
|
3 a. Describe the structure and location of the periosteum.
|
The membrane that lines the outer surface of old bones except for the joints long bone
|
|
|
b. With long bones, specifically, where is the growth most obvious?
|
Growth is most obvious Towards the ends .
|
|
|
|
|
|
|
4 a. Describe/Draw a long bone.
|
The bones that are longer than they are wide, Such as the femur , fibula, tibula, humerus
|
|
|
b. What advantage is there for a medullary cavity?
|
the bones are lighter. If they were solid we would weight 300lbs.
|
|
|
5 a. Describe/Draw the microscopic anatomy of compact bone.
|
osteocytes are arranged in a cocentric layer which contains blood that supplys the osteon.
|
|
|
b. How do osteocytes get nutrients? Is diffusion possible?
|
osteoctye receive nutrients through blood vessels that travel near them. Diffusion is possible
|
|
|
6 a. Where is spongy bone in a typical long bone?
|
in the epiphysis
|
|
|
b. Is spongy bone strong? How can spongy bone withstand stress?
|
Spongy bone is strong. It forms a strong mesh of cells that can withstand lots of
|
|
|
7 a. Describe the steps of endochondral ossification.
|
two essential processes during fetal development of the mammalian skeletal system resulting in the creation of bone tissue
|
|
|
b. Why is endochondral ossification not appropriate for the skull?
|
Because it is the process used to make long bones.
|
|
|
|
|
|
|
8 a. How is intramembranous ossification different from endochondral ossification?
|
endochondrial ossification is the production of hyline cartridge. Intramembrnaous ossification being with mesenchymal cells
|
|
|
b. Which do you think is faster? Why?
|
intramembranous is faster.
|
|
|
9 a. Describe the different arteries and their locations in bone.
|
metaphyseal vessels, epiphyseal, periosteal
|
|
|
b. Why do arteries need to penetrate bone, why not just stay on the surface?
|
because the bone is living tissue and require blood and nutrients too.
|
|
|
10 a. Describe some markings on bones.
|
trochanter, head, neck, facet, tubercle and chondyle.
|
|
|
b. Why do we have so many different names?
|
there are many different types
|
|
|
3 major functions of Cartilage CT
|
1. supporting soft tissues 2. provide a gliding surface for joints 3. model for forming bones
|
|
|
Chondroblasts
|
cells that produce matrix of protien that form the gel like ground substance
|
|
|
Chondrocytes
|
mature cartilage cell.
|
|
|
Lacunae
|
space that trap the chondrocyte in the gel like matrix
|
|
|
name the 3 types of cartilage
|
fibrocartilage, hyaline cartilage, elastic cartilage
|
|
|
Hyaline Cartilage
|
found in joints to minimize friction
|
|
|
Perichondrium
|
a layer of dense irregular connective tissue which surrounds the cartilage of developing bone. It consists of two separate layers: an outer fibrous layer and inner chondrogenic layer. The fibrous layer contains fibroblasts, which produce collagenous fibers.
|
|
|
Fibrocartilage
|
contains a lot of collagen fiber. Collagen fibers imply that it requires strength. Found in found in the vertibral column and pubic symphysis
|
|
|
Elastic Cartilage
|
found in the epiglottis and ear
|
|
|
Interstitial Growth
|
cartilage that grows from within
|
|
|
Appositional Growth
|
cartilage that grow from the end
|
|
|
Bone CT
|
osseous CT. Has a sturdy martix because of calcification and mineralization
|
|
|
Calcification
|
Hardening of of bone by apsorption of calicium and phosphates
|
|
|
Functions of bone
|
1. support & protection 2. Movement 3. hemopooiesis 4. mineral storage and energy reserves.
|
|
|
Support & Protection
|
bone provide the support and framework for the entire body and protect delicate tissue. E.g. the skull protects the brain
|
|
|
Movement
|
Muscles attached to the bones of the skeleton contract and exert a pull on the skeleton, which then functions as a series of levers.
|
|
|
Hemopoiesis
|
the production of red blood cells
|
|
|
Red bone marrow
|
a mixture of mature and immature red and white blood cells. Is the base of blood production inside the marrow of some bones.
|
|
|
Yellow bone marrow
|
a loose connective tissue that may be dominated by adipose tissue.
|
|
|
Storage of Mineral & Energy
|
90% of the body's reserve of calicum and phostpate is stored in the bones.
|
|
|
Bone Classification
|
1. long 2. short 3. flat 4. irregular
|
|
|
Long Bones
|
Found in limbs, carpals
|
|
|
Short Bones
|
SEE PICTURE
|
|
|
Flat Bones
|
Found in skull
|
|
|
Irregular Bones
|
SEE PICTURE
|
|
|
Long Bone Structure
|
SEE PICTURE
|
|
|
Diaphysis
|
shaft of a bone
|
|
|
Epiphysis
|
ends of a bone
|
|
|
Proximal vs. Distal
|
|
|
|
Metaphysis
|
narrow zone that connects the epiphysis and diaphysis.
|
|
|
Epiphyseal Line
|
replaces the epiphyseal plate in mature bones
|
|
|
Articular Cartilage
|
type of Hyline cartilgae that Joints a bone with another bone
|
|
|
Medullary Cavity
|
cavity inside a bone that contains bone marrow.
|
|
|
Endosteum
|
lines the medullary cavity. Covers the trabeculae of spongy bone and lines the inner surface central and perforating canals.
|
|
|
Periosteum
|
a connective tissue that covers the outer layer of compact bone connected to the deep fascia.
|
|
|
4 functions of the periosteum
|
1. isolates the bones from the surrounding tissues 2. attachment for circulatory and nervous supply. 3. participates in bone growth and repair. 4. attaches bone to ct network of deep fascia.
|
|
|
Perforating Fibers
|
collagen fibers incorporated into bone tissue from the tendons to the superfiscial periosteum. Aka shipley fibers
|
|
|
Osteoprogenitor Cells
|
from stem cells. differentiate from mesenchyme and are found in the inner most layer of the periosteum and in the endosteum lining the meduallary cavities.
|
|
|
Osteoblasts
|
immature cell that secretes matrix to form new bone. Becomes an ostreocyte. found on the inner and outer surface of a bone
|
|
|
Osteoid
|
the organic components of bone matter secreted by the osteoblasts.
|
|
|
Osteocytes
|
mature bone cells. (osteon or bone).
|
|
|
Lacunae
|
small chambers that contain osteocytes.
|
|
|
Osteoclasts
|
Cells that secrete acids that dissolve the bony matrix and release amino acids and the stored calcium and phosphates. They are multinucleate cells that are derived from the same cells that produce monocytes and neutrophils.
|
|
|
Resorption Lacuna
|
a pit or groove in developing bone that is undergoing resorption; frequently found to contain osteoclasts.
|
|
|
Bone Resorption
|
process by which osteoclasts break down bone[1] and release the minerals, resulting in a transfer of calcium from bone fluid to the blood.
|
|
|
Osteolysis
|
the process of bone erosion that releases calcium and phosphate into the blood stream.
|
|
|
Composition of Bone Matrix
|
|
|
|
Hydroxyapatite
|
a naturally occurring mineral form of calcium apatite. Up to fifty percent of bone is made up of a modified form of the inorganic mineral hydroxylapatite.
|
|
|
Spongy Bone
|
made up of branching, paralell struts called trabeculae (aka spicules)
|
|
|
Trabeculae
|
a small, often microscopic, tissue element in the form of a small beam, strut or rod, generally having a mechanical function, and usually but not necessarily composed of dense collagenous tissue.
|
|
|
Parallel Lamellae
|
|
|
|
Diploe
|
central layer of spongy, porous, bony tissue between the hard outer and inner bone layers of the cranium.
|
|
|
Compact Bone
|
aka dense bone. Relatively dense tissue that forms the walls of bones.
|
|
|
Osteon
|
aka haversian system. Cylindrical basic functional unit of mature bone.
|
|
|
Central/Haversian Canal
|
the space which is surrounded by osteocyte arranged in cocentric layers
|
|
|
Concentric Lamellae
|
cylindrical lamellae of each osteon that are align parallel to the long axis of the bone.
|
|
|
Canaliculi
|
channel that radiate from lacuna to lacuna toward free surfaces and adjacent blood vessels
|
|
|
Perforating/Volkmann Canal
|
passageway that extend perpendicular to the surface that allow blod vessels to service the medullary cavity
|
|
|
Circumferential Lamellae
|
forms the outer surface and inner surfaces of the bone.
|
|
|
Interstitial Lamellae
|
fills the spaces between the osteons in compact bone.
|
|
|
at what stage of development does intermembranous ossification begin
|
8th week of embryonic development.
|
|
|
Intramembraneous Ossification
|
bone develops from the mesenchyme or fibrous connective tissue. Forms flat bone like the clavicle, mandible, and the flat bones of the face and skull.
|
|
|
Mesenchyme
|
loosely packed, unspecialized cells that are set in a gelatinous ground substance, from which connective tissue, bone, cartilage, and the circulatory and lymphatic systems develop during embryonic development
|
|
|
Ossification Centers
|
site where bone begins to form in a specific bone or part of bone as a result of the accumulation of osteoblasts in the connective tissue
|
|
|
Osteoid Calcifications
|
|
|
|
Woven Bone
|
disorganized structure with a high proportion of osteocytes in young and in healing injuries.
|
|
|
Lamellar Bone
|
the hard, rigid form of connective tissue constituting most of the skeleton of vertebrates, composed chiefly of calcium salts.
|
|
|
Compact Bone
|
is one of the two types of osseous tissue that form bones. SEE PICTURE
|
|
|
Spongy Bone
|
aka trabecular bone. Is an open network of struts and plates. Forms the inner layer that surrounds the medullary cavity
|
|
|
Endocondral Ossification
|
bone replaces existing cartilage. Forms the vertibral column, limbs and other weight bearing bones. MOST OF THE BONES IN THE BODY ARE FORMED THIS WAY.
|
|
|
Fetal Hyaline Cartilage Model
|
in week 8-12 of development bone are made of hyaline cartilage and serve as the model for the bone.
|
|
|
Periosteal Bone Collar
|
cuff of periosteal bone that forms around the diaphysis of the hyaline cartilage model in developing long bones.
|
|
|
Primary Ossification Center
|
see picture, Medulliary cavity
|
|
|
Secondary Ossification Centers
|
see picture, epiphyseal plate
|
|
|
Epiphyseal Plate
|
(aka growth plate) made of hyaline cartilage and doesn’t calcify until adulthood.
|
|
|
Zone of Resting Cartilage
|
part of 1 endochondrial ossification. Zone contains normal resting hyaline cartilage
|
|
|
Zone of Proliferating Cartilage
|
part of 2 endochondrial ossification. chondrocytes undergo rapid mitosis, forming distinctive looking stacks
|
|
|
Zone of Hypertrophic Cartilage
|
part of 3 endochondrial ossification. chondrocytes undergo hypertrophy (become enlarged). Chondrocytes contain large amounts of glycogen and begin to secrete alkaline phosphatase.
|
|
|
Zone of Calcified Cartilage
|
part 4 endochondrial ossification. chondrocytes are either dying or dead, leaving cavities that will later become invaded by bone-forming cells. Chondrocytes here die when they can no longer receive nutrients or eliminate wastes via diffusion. This is because the calcified matrix is much less hydrated than hyaline cartilage.
|
|
|
Zone of Ossification
|
|
|
|
Epiphyseal Line
|
line that is formed when the epiphyseal plate is calcified at maturity
|
|
|
Bone Growth
|
|
|
|
Bone Remodeling
|
the bone continues to reshape itself throughout a person’s lifetime in a constant process of bone resorption and deposition.
|
|
|
Blood Supply for bone
|
The nutrient artery and vein enter through the " Bone is highly vascularized, especially in regions containing red bone marrow.periosteum.
|
|
|
Nutrient Artery & Vein
|
enter the bone through the periosteum and supplies the areas that contain bone marrow.
|
|
|
Metaphyseal Arteries & Veins
|
see image
|
|
|
projections
|
|
|
|
What is a process?
|
bone marking that describes anything that sticks out
|
|
|
Crest
|
a narrow ridge like projection
|
|
|
epicondyle
|
projection adjacent to a condyle
|
|
|
line
|
low ridge
|
|
|
ramus
|
angular extenstion of a bone relative to the rest of the structure.
|
|
|
spine
|
pointed slender process
|
|
|
trochanter
|
massive, rough projection found only on the femur.
|
|
|
tubercle
|
small, round projection
|
|
|
tuberosity
|
large rough projection
|
|
|
depressions
|
|
|
|
alveolus
|
a deep pit or socket in the mandible or maxilla
|
|
|
fossa
|
flattened or shallow depression
|
|
|
sulcus
|
narrow groove
|
|
|
Atriculating surfaces
|
|
|
|
Condyle
|
large, smooth round oval structure
|
|
|
facet
|
small flat shallow articulating surface
|
|
|
head
|
prominent rounded epiphysis
|
|
|
trochlea
|
smooth grooved pulley-like articular surface.
|
|
|
Openings
|
|
|
|
Canal (meatus)
|
passageway through a bone
|
|
|
Fissure
|
narrow slit like opening
|
|
|
Foramen
|
rounded passageway though a bone
|
|
|
Sinus
|
cavity or hollow space in a bone.
|
|
|
What is the major function of the skeletal system
|
1. Support 2. storage ofcalium and phosphate ions 3. Blood cell production 4. Protection of delicate tissues and organs 5. Leverage
|
|
|
Osseous tissue
|
bone
|
|
|
Lamellae
|
layers of calified matrix that sandwich lacunae
|
|
|
osteogenisis
|
process of making new bone
|
|
|
marrow
|
a loose connective tissue that may be dominated by adipocytes
|
|
|
name the 3 types of lamellae in long bone
|
concentric, interstitial, circumferential
|
|
|
what are the functional differences between compact and spongy bone.
|
compact bone forms the outside surface of bone and spongy bone forms the inside support of the the bone.
|
|
|
what are the 3 steps of intramembranous ossification?
|
1. mesenchymal cells differentiate into osteoblasts and secretes the the organic compound that makes up the matrix. 2. small struts grow outward from the OSSIFICATION CENTER to form Spicules. 3. more ossification centers form and newly deposited bone assumes the structure of spongy bone.
|
|
|
what are the 4 steps of endochondrial ossification
|
1. cartilage enlarges near the center of the of the shaft. Cells of the perichondrium differentiate into osteoblasts to form a BONE COLLAR, a layer of thin compact bone around the shaft. 3. calcified cartilagenous matrix breaks down and is replaced by spongy bone. 4. ostecyte erode the center to form the medullary cavity.
|

