![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
31 Cards in this Set
- Front
- Back
|
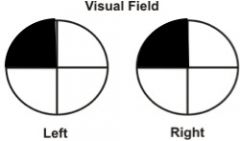
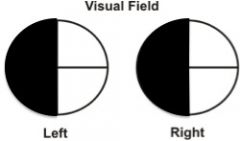
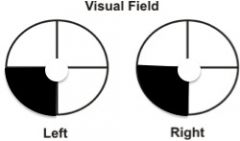
Left Optic Nerve
|
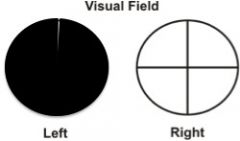
Left Eye Monocular Anopia or
Left Monocular Vision Loss |
|
|
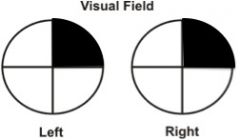
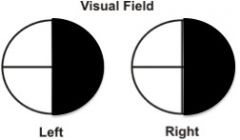
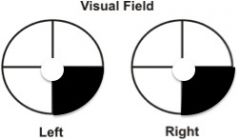
Optic Chiasm
|
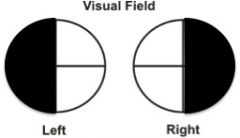
Heteronymous bitemporal hemianopia
|
|
|
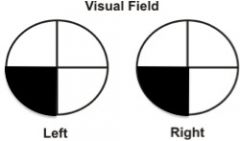
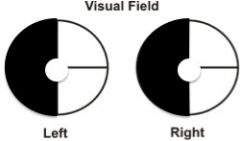
Right Optic Tract
|
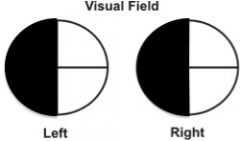
Left homonymous hemianopia
|
|
|
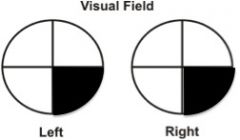
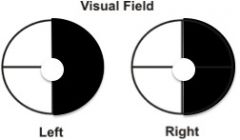
Left Optic Tract
|
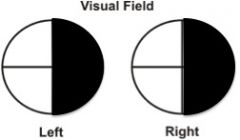
Right homonymous hemianopia
|
|
|
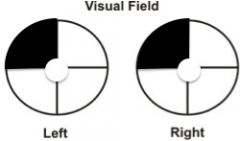
Right Meyer's Loop
|
Left superior homonymous quadrantanopia
(pie in the sky disorder) |
|
|
Left Meyer's Loop
|
Right superior homonymous quadrantanopia
(pie in the sky disorder) |
|
|
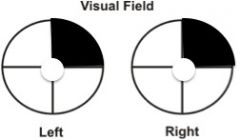
Right Parietal Loop
|
Left inferior homonymous quadrantanopia
(pie in the floor disorder) |
|
|
Left Parietal Loop
|
Right inferior homonymous quadrantanopia
(pie in the floor disorder) |
|
|
Right Optic Radiation
|
Left homonymous hemianopia
|
|
|
Left Optic radiation
|
Right homonymous hemianopia
|
|
|
Right lingual gyrus
(inferior banks of calcarine fissure of V1) sparing macula region |
Left superior homonymous quadrantanopia with macular sparing
|
|
|
Left lingual gyrus
(inferior banks of calcarine fissure of V1) sparing macula region |
Right superior homonymous quadrantanopia with macular sparing
|
|
|
Right cuneus gyrus
(superior banks of calcarine fissure) sparing the macula region |
Left inferior homonymous quadrantanopia with macular sparing
|
|
|
Left cuneus gyrus
(superior banks of calcarine fissure) sparing the macula region |
Right inferior homonymous quadrantanopia with macular sparing
|
|
|
Right V1
sparing macula region |
Left homonymous hemianopia with macular sparing
|
|
|
Left V1
sparing macula region |
Right homonymous hemianopia with macular sparing
|
|
|
Right Optic Nerve
|
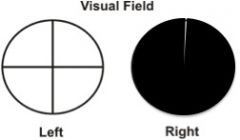
Right eye monocular anopia or
Right monocular visual loss |
|
|
pituitary adenomas |
lesions often compress the optic chiasm disrupting inferior nasal crossing fibers. Damage equals bitemporal superior quadrantanopsia |
|
|
injuries to the optic chiasm, lateral geniculate bodies, or occipital cortex cause what type of visual field loss |
contralateral quadrantanopsia or hemianopsia |
|
|
what is rare but might be the only physical manifestation of a contralateral temporal lobe lesion (i.e., residual temporal lobectomy) |
homonymous superior quadrantanopia (i.e., pie in the sky" |
|
|
when does macular sparing happen? |
in the occipital lobe (i.e., back part of optic radiations) |
|
|
eye deviation from cerebral lesions |
partial seizures push the eyes contralaterally; stroke pushes the eyes to look toward the lesion. |
|
|
conjugate eye movement |
supranuclear gaze centersinnervate pontine (nuclear) gaze centers, which innervated nearby oculomotor (CN3), trochlear (CN4), and abducens (CN6) |
|
|
progressive supra-nuclear palsy |
damage of the cortical bulbar tracks abolishing voluntary conjugate gaze. PSP patient's cannot voluntarily look upward or downward, and then later to either side. seen in Parkinsonian and Dementia, |
|
|
what does the pontine gaze center due to? |
a pontine center pulls the eyes towards its own side. So a stroke on one side of the pons allows the eyes to be pulled to the opposite side. Ex: Damage to right pontine gaze Center the eyes would deviate to the left. Left-sided hemiparesis would also be evident. With brainstem lesions the eyes look towards the paralysis. |
|
|
what is medial longitudinal fasciculus syndrome (AKA intranuclear opthalmoplegia). |
spares the cranial nuclear eye and nerves and causes a classic pattern of ocular movement impairment identified by inability of the eye ipsilateral to the lesion to adduct past midline. often seen in MS and brainstem strokes |
|
|
nystagmus |
rhythmic horizontal, vertical, or rotary oscillations of both eyes. While often seen in CNS injuries it may be the most prominent physical finding from alcohol or drug intoxication including Wernicke's-Korsakoff syndrome. |
|
|
oculomotor (CN3) nerve palsy |
Causes diplopia. often comes with ptosis, lateral deviation of the eye, and dilated/blown pupil. Often most pronounced when the patient attempts to abduct the eye |
|
|
abducens (CN6) Nerve injury |
causes diplopia and inability of abduction |
|
|
what medications can cause transient visual difficulties |
tricyclic antidepressants due to anticholinergic side effects (i.e., amitriptyline) |
|
|
Optic Neuritius |
The loss of vision, accompanied by an impaired direct light reflex, but preserved consensual response, indicates that the problem is in the optic nerve. This cranial nerve forms the afferent limb of the light reflex. The pain indicates nerve inflammation, i.e., neuritis. In optic neuritis, the “patient sees nothing and the ophthalmologist sees nothing.” Optic neuritis as an isolated condition or a manifestation of multiple sclerosis (MS) occurs relatively commonly among young adults. |

