![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
58 Cards in this Set
- Front
- Back
|
DISEASE ALTERS FUNCTION OF GI TRACT BY: |
decreased synthesis/ release of secretions for digestion alters motility -inflames/ damages GI tract -Alters transit time |
|
|
4 Main Structures of the Digestive Process |
oral cavity, esophagus, stomach, small intestine & lage intestine |
|
|
4 Main Accessory Organs |
-Pancreas -Liver -Gallbladder -other accessory organs: salivary glands, oral cavity, pharynx, |
|
|
The Lumen of the Digestive Tract's 4 Layers |
Mucosa: exocrine/ endocrine function--> epithelium, lamina propria, muscularis mucose Submucosa: connective tissue, lymphoid tissue, submucosal plexus Muscularis Externa: circular/ longitudinal smooth muscle, myenteric plexus Serosa or Adventitia: connective tissue, visceral peritoneum |
|
|
Salivary Glands |
-Parotid -submandibular -sublingual |
|
|
Enzymes in Saliva |
-Lingual Lipase -amylase |
|
|
ESOPHAGUS |
-moved bolus from oral cavity to stomach - swallowing: voluntary, pharyngeal, esophageal -Peristalsis -Gastroesophageal sphincter
|
|
|
Antrum/ Distal Pyloric Region |
-grinds food & mixes with gastric juices to form chyme -strong peristalsis for gastric emptying
|
|
|
4 Main Regions of Stomach |
-cardia region -fundus -body -antrum or distal pyloric region -size of stomach when empty: 60ml -size of stomach when full: 1.5L
|
|
|
Pyloric Sphincter |
regulates the flow of chum from the stomach into the upper or proximal small intestine (duodenum) a sphincter separates a small from large bowel |
|
|
Lower Esophageal or Gastroesophageal Sphincter |
regulates the flow of food from the esophagus into the stomach |
|
|
Stomachs 3 Layers of Muscle |
-longitudinal -circular -diagonal -forceful contractions of these muscles enable food to mix with gastric juice form chyme |
|
|
Gastric Glands |
-Cardiac (near LES) -Oxyntic (fundus) - Pyloric (antrum) |
|
|
Enteroendocrine G-Cells |
produce the hormone gastrin, which stimulates parietal and chief cells |
|
|
HCL (Gastric Juice) |
-converts pepsinogen to pepsin (protease) -denatures protein -releases nutrients from organic complexes -acts as bacteriocide (we consume a lot of bacteria, leading to suppressed immune system feeding through post-phylon tube, so its important to make sure nothing is expired -important for iron absorption
|
|
|
Intrinsic Factor |
-Super important for B12 -absorb B12, protects it from environment, and releases it from ilium |
|
|
The Stomach Functions |
-Limited chemical digestion takes place in the stomach - initiation of protein hydrolysis -limited initiation of starch hydrolysis -absorbs H20, alcohol, a few drugs, and a few minerals |
|
|
Hormones and Peptides that Inhibit Gastric Secretions |
-Peptide YY, enterogastrone, secretin, NO (vasodilator: widens blood vessels and secretes blood pressure), Somatostatin, prostaglandins |
|
|
Hormones and Neuropeptides that Stimulate Gastric Secretions |
-Bombesin, gastrin, coffee, AA, alcohol, Ca++, peptides |
|
|
STOMACH DISEASES THAT ALTER MOTILITY |
-Gastroparesis, pyloric stenosis, gastric bypass, partial resection for cancer/pud, toxicity to mucosa |
|
|
Stomach Diseases That Cause Inflammation to GI Tract |
-H Pylori -Meds: ASA (Aspirin), NSAIDS (Aspirin/ ibuprofen), alcohol |
|
|
Pyloric Stenosis |
when pylorus doesn't open or close |
|
|
Effects of Dietary Fiber on Stomach Motility |
food remains in stomach longer/ you feel fuller longer |
|
|
FAT |
Delays gastric emptying |
|
|
SMALL INTESTINE |
-surface area: 300m2 - 3' Duodenum (<1) -Jejenum/ Ileum (>91) Peptide YY: which decreases secretion -has CCK: which stimulates bile secretion from Pancreas
|
|
|
Villi |
-finger-like projections in small intestine -each villus is made of absorptive cells called enterocytes -enterocytes are covered with microvilli each villus contains a capillary network and a lymphatic vessel (lacteal) |
|
|
Microvilli |
hair-like extensions in small intestine -cover enterocytes which project into intestinal lumen |
|
|
Folds of Kerckring |
large circular folds of mucosa and submucosa |
|
|
Crypts of Lieberkuhn |
cell turnover |
|
|
VIP (Vasoactive intestinal polypeptide) |
-present in neurons within the gut -increases motility within the small intestine - |
|
|
MALT (Mucosa-associated lymphoid tissue) |
-leukocytes, T& B lymphocytes, plasma cells, NK Cells, macrophages |
|
|
GALT |
gut-associated lymphoid tissue (non-mucosal layer) |
|
|
PANCREAS |
-Endocrine cells secrete hormones into the blood (Insulin, glucagon, somatostatin) -Exocrine cells secrete digestive enzymes into pancreatic duct -Pancreatic Juice contains: bicarbonate, electrolytes (Na+, K, Cl-, Ca), and pancreatic digestive enzymes (amylase and lipase) -has an acid-base dump that can dump acidic food into small portion of small intestine because some things are absorbed better in alkaline environment and others in acid environmentla
|
|
|
Islets of Lagerhans |
-secretes hormones |
|
|
Proteases |
-Protein digestion enzyme from pancreas -digests 50% of protein |
|
|
Alpha-Amylase |
-Carbohydrate Digestion Enzyme (50%) |
|
|
Pancreatic Lipase |
-80-90% of fat digestion |
|
|
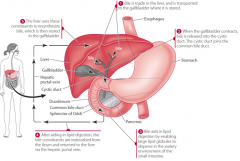
Liver |
- has 2 lobes -largest organ in the body -portal circulation -synthesizes bile from cholesterol -stores glycogen, helps people keep normal blood sugar when they are not eating -Filters toxins from blood (main function) to put them in state to where they can circulate during the bloodstream |
|
|
Gallbladder |
-bile concentration and storage -bile excretion (stimulated by CCK) |
|
|
Bile: |
-secreted from gallbladder -stimulated by CCK -inhibited by somatostatin -bile emulsifies fat -enterohepatic circulation of bile and cholesterol occurs twice per meal -Bile emulsifies fat cells (breaks down fat) |
|
|
Digestion |
Occurs in small bowel |
|
|
Lipid Digestion Process Flowchart |
|
|
|
Lipid Digestion Process (Step-by-Step) |
1) Bile is made in the liver 2) When the gallbladder contracts, its released into the cystic duct. The cystic duct joins the common bile duct. 3)Bile aids in lipid digestion by enabling large lipid globules to disperse in the watery environment of the small intestine. 4) After aiding in lipid digestion, the bile constituents are reabsorbed from the ileum and returned to the liver via hepatic portal vein. |
|
|
Digestive/ Absorptive Processes |
-Digestion: breaking nutrients down -occurs in lumen & at brush border -most digestion & absorption occur in proximal small intestine - accomplished through enzymes with help from bile -absorption may be by diffusion, facilitated diffusion, active transport, or pinocytosis/ endocytosis - |
|
|
Mechanism of Digestive System |
-Mechanism of Absorption depends on: * Solubility (fat vs water) * Concentration or electrical gradient * Size of molecule -Whatever matters remain unabsorbed move onto colon and make fuel source for bacteria |
|
|
Colon/ Large Intestine |
-contracts to mix materials -proximal epithelia absorb Na, Cl, H20 (absorb 90-95% of it) - Materials dehydrated (1 liter of chyme yields 200g defecation) -passage through colon is 12-70 hr
|
|
|
Intestinal Bacteria (Microflora) Fermentation |
intestinal bacteria ferments anaerobic breakdown of CHO and protein by bacteria generates lactate & SCFA & gases -composition of microflora is affected by substrate availability, pH, meds, diet |
|
|
Probiotics |
-foods containing live bacterial cultures
|
|
|
Prebiotics |
food ingredients that promote bacterial growth |
|
|
Benefits of Probiotics |
-enhance immunity (IgA) - Prevent colonization by pathogens -lower colon pH -Transform/ promote excretion of toxic substances (e.g. nitrosamine) |
|
|
Microbiome |
-humans carry 2 sets of genes which interact: those encoded in their own genome and those encoded in their microbiota genome - You inherit 1% of genes from parents and 99% of genes from the environment in which we are born (breast milk, birth canal) - Symbiotic relationship/ interactome -there are trillions of bacteria in your gut, making it the most colonized organ (trillions of microbes) |
|
|
Dysbiosis of the Gut |
-microbial imbalance on or inside the body - leads to diseases like IBS, Chronic fatigue syndrome, obesity, cancer, and colitis
|
|
|
Pathogens Effect on the Microbiome |
-interferes with transcription, translation, and DNA repair at the cellular level -dysregulates the Vitamin D nuclear receptor (VDR), which expresses more than 913 genes, may be connected to autoimmune system and auto inflammatory processes; any microbe capable of disregulating the VDR impairs the innate immune response |
|
|
Mucin |
heavily glycosylated proteins are the major organic components of the mucus layer (the protective layer covering the epithelial cells in many human and animal organs , including the entire gastro-intestinal tract -benefits microbes because they can get nutrients, experience physicochemical protection, and adhere, resulting in increased residence time.
|
|
|
Conditions that Affect the Density of Colonization & Composition of the Resident Microbe Communities in the STOMACH AND SMALL BOWEL |
-low microbial colonization is caused by: * low PH * Oxygen exposure * Rapid transit time |
|
|
Large Intestine |
-large microbial concentration is caused by: high pH -Anaerobic environment -slow transit time
|
|
|
Enterotype |
-classification of living organism based on its bacteriological ecosystem in the gut micro-biome -3 types: *prevotella: favors low-fat diet * Bacteroides: favors high-fat diet *Ruminococcus |
|
|
Time and Gut Microbiome |
short-term dietary interventions do no not significantly alter the gut micro biome, though microbial gene expression and functional profiles adapt to changes in diet rapidly |

