![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
38 Cards in this Set
- Front
- Back
|
Post-Renal AKI:
Definition Causes |
Obstructive uropathy; interruption of urine outflow
Causes: Children: congenital Males: Prostate disorder Females: Gynecological tumors |
|
|
Post-Renal Obstruction:
Partial vs Complete Obstruction |
Partial:
Continued filtration and preservation of GFR due to PGs (vasodilation of afferent arteriole) If prolonged and high grade (>4-5hrs): Thromboxane (vasoconstriction)-->Decline in GFR Complete obstruction: Filtration continues initially Increased tubular pressure Cessation of filtration-->Anuria |
|
|
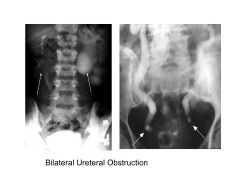
What post-renal changes are required for a decline in GFR?
|
Blockage of BOTH kidneys
Severity of decline depends on duration of blockage and degree of obstruction |
|
|
______ present with post-renal obstruction is a medical emergency.
|
Infection
|
|
|
Post-Renal AKI:
Treatment Complications |
Relieve obstruction at site of blockate (foley--bladder outlet obstruction, nephrostomy tube--ureter, ureteral stent--ureter, ureteropelvic junction)
Replace fluid losses if pt has large volume diuresis (polyuria due to loss of tubular concentrating ability) Complications: Distal tubular injury: Post-obstructive diuresis (impaired Na+ reabsorption, insensitive to ADH) Inability to excrete H+ (normal AG metabolic acidosis) |
|
|
What is the degree of recovery expected in a patient with post-renal obstruction? Provide answers by DURATION of obstruction.
|
<2 weeks: Complete recovery
Up to 3 mos: Residual impairment >3 months: No recovery |
|
|
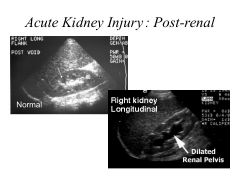
What ultrasound finding indicates a poorer prognosis in patients with post-renal AKI?
|
Thin renal cortex
|
|
|
Pre-Renal AKI:
Definition Causes |
No intrinsic renal pathology
Decline in GFR due to poor blood flow through kidneys Causes: Volume depletion Systemic decline in renal perfusion Selective decline in renal perfusion |
|
|
Systemic Hypoperfusion
|
Hypotension in setting of shock (sepsis, anaphylaxis)
CHF Cirrhosis (hepatorenal syndrome, decreased intravascular volume) |
|
|
Hepatorenal Syndrome
|
Decreased intravascular volume due to poor oncotic pressure; results in poor renal perfusion in otherwise normal kidney (dec GFR)
Poor perfusion despite volume repletion bc splanchnic vasodilation due to low systemic vascular resistance (blood diverted away from kidneys) |
|
|
Selective Renal Hypoperfusion
|
Afferent arteriolar vasoconstriction (NSAIDs)
Efferent arteriolar dilatation (ACEI, ARBs) |
|
|
Effects of Renal Artery Stenosis
What medicines should be avoided in its treatment? |
Not AKI, this is a chronic process
Results in chronically constricted efferent arteriole; ARF induced in setting of ACEI or ARB administration |
|
|
Pre-Renal AKI:
Treatment Prognosis |
Tx: removal or treatment of inciting event
EXCELLENT PROGNOSIS (unless can't make precipitating event go away, e.g., cirrhosis) |
|
|
Intrinsic Renal Disease:
Definition Causes |
Renal parenchymal dz
Renal failure due to pathology of any portion of filtering unit (vascular dz, glomerular dz, interstitial inflammn, tubular dz: ischemic or toxic insult) Cause: Most common = ACUTE TUBULAR NECROSIS Others: vasculitis, GN, interstitial nephritis |
|
|
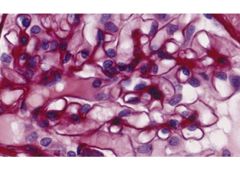
Why are renal tubules so prone to ischemic injury? Which region of the kidney is most susceptible?
|
Medulla is hypoxic and prone to ischemia due to hairpin loop structure
Ascending LOH most susceptible to ischemia Also affected by reperfusion injury (Ca2+, oxygen radicals_ |
|
|
Why are the kidney tubules so prone to toxic injury?
What substances cause tubular necrosis? |
Tubular cells are exposed to drugs/toxin levels far exceeding plasma levels:
20% of CO allocated to kidney; high renal blood flow-->inc'd exposure to drugs/toxin High intracellular and intraluminal concentrations Toxic injury substances: Aminoglycoside abx Heme pigments (Hg, myoglobin) Cis platinum IV contrast dye |
|
|
In intrinsic AKI:
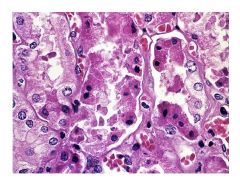
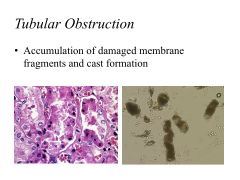
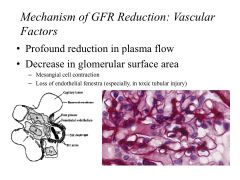
Mechanisms of GFR reduction Mechanisms of Tubular Obstruction |
GFR reduction: tubular injury, but intact glomerulus
Tubular obstruction: Accumulation of damaged membrane fragments and cast formation |
|
|
How does back leak of glomerular filtrate occur?
|
In intrinsic AKI, injured tubules are no longer impermeable to filtrate and allow indiscriminate reabsorption of filtered substances; results in minimal clearance
|
|
|
Risk factors for intrinsic AKI.
|
**DM
**Cirrhosis Chronic Kidney Dz Heart Surgery (hypoperfusion) IV contrast dye |
|
|
Intrinsic AKI:
Prognosis |
50% mortality
Recovery usually occurs w/resoln of primary illness Not a risk factor for chronic kidney dz Most have COMPLETE recovery Poorer prognosis with repeated insults of poor systemic hemodynamics; with pts with persistent oliguria (low urine output) |
|
|
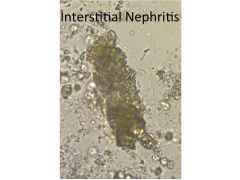
Acute Interstitial Nephritis:
Causes Onset Presentation Lab Findings |
Causes:
Infections Medications (most common cause): cephalosporins, PCNs; NSAIDS including COX-2 inhibitors (celecoxib), diuretics Onset: 2-3 weeks (rapid onset with allergic reaction; delayed onset--months--with diuretics, NSAIDs) Not dose dependent; recurrent with re-exposure Presentation: Fever, constitutional syx, rash Lab: Eosinophilia, eosinophilURIA, WBC casts and WBCs in urine (mild proteinuria) |
|
|
Acute Interstitial Nephritis:
Treatment Prognosis |
Tx: Withdrawal of medication, treatment of underlying cause, corticosteroid therapy
Most recover after cessation of medication |
|
|
Nephrotic vs Nephritic Syndrome:
Physical exam and lab findings |
Nephrotic:
>3g proteinuria daily Hypoalbuminemia Edema Nephritic: Hematuria HTN (hypervolemia) Azotemia |
|
|
|
|

|
|
|

|
|
|
|
|
|
|
|
|
|
Causes of glomerular disease with low complement. Provide primary and secondary causes.
|
Low complement:
Primary Renal Dz: Membranoprolif GN Systemic/Secondary: These are all immune mediated: Post Strep/Infectious GN Lupus Nephritis Hep B/C related GN Cryoglobulinemia |
|
|
Causes of glomerular disease with normal complement. Provide primary and secondary causes.
|
Primary: AntiGBM dz, Minimal Change Dz, IgA nephropathy
Secondary: These are all systemic dz's w/glomerular dz: Goodpastures, Microscopic polyangitis, HIC assoc nephropathy |
|
|
Formula for fractional excretion of substance X.
|
FEx = Clx/GFR x 100%
= (Ux/Px)/(Ucr/Pcr) x 100% |
|
|
Pre-Renal vs Intrinsic Renal Disease:
BUN/Cr Ratio Uosm Urinary Na FE Na Urinalysis |
Pre-Renal; Renal
BUN/Cr: 20:1; 10-15:1 Uosm: >500; <350 Urinary Na: <10-20; >40 FE Na: <1%; >2% Urinarlysis: Normal; ATN: muddy brown granular casts, tubular epithelial cells, AIN: WBC casts, GN: RBC casts, dysmorphic RBCs |
|
|
Complications of AKI
|
Volume overload
Hyperkalemia Metabolic Acidosis Uremia Hypocal, Hyperphos |
|
|
Low urine sodium is indicative of ______-renal injury.
|
Pre-renal
|
|
|
Calculate FeNa for:
Urine Na: 10 Serum Na: 140 Urine Cr: 20 Serum Cr: 2.0 Is this pre-renal or intrinsic-renal? |
FeNa = (UNa/PNa)/(UCr/PCr)x100%
=(10/140)/(20/2.0)x100% =0.7% This is pre-renal (<1%) |
|

|
|
|

|

|
|

|
|

