![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
ADC vs DWI |
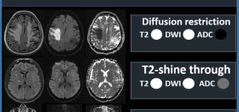
Facilitate diffusion: DWI dark, ADC bright Restricted diffusion : DWI bright, ADC dark (if ADC here is also bright than- T2 shine through). |
|
|
Spectroscopy mri |
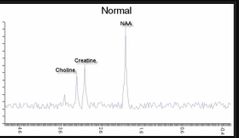
Stroke Lactate ⬆️ (anaerobic metabolism) NAA⬇️ (N Acetyl Asparate- neuronal density and integrity)
Tumor Choline ⬆️ (membrane turnover) NAA⬇️ (N Acetyl Asparate- neuronal density and integrity) Rest |
|
|
Restricted diffusion
DWI (bright) low ADC (dark) |
1. Abscess 2. Acute phase stroke (cytotoxic edema) 3. Highly cellular tumor: glioblastome (not necrotic center), lymphoma, medulloblastoma. 4. Epidermmoid cyst (also can have T2 shine through). |
|
|
Anterior fontanelle typically close? |
Between 12 and 18 months of age. Closure at 6 months may be normal. Large fontanelle or persistence beyond 18 months - sign of hypothyroidism |
|
|
The posterior fontanelle typically closes? |
between 3 and 6 months of age. |
|
|
CN IV |
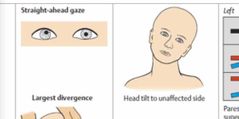
Trochlear nerve Innervate the superior oblique muscle. |
|
|
Most common neurologic examination finding (ophthalmology) in paediatric Pseudotumor cerebri? |
Aside from papilloedema, sixth nerve (CN VI) palsy is the most common neurologic examination finding in paediatric IIH. |
|
|
CN V (trigeminal nerve) Motor component: |
muscles of mastication (temporalis and masseter muscles) and the muscle involved in keeping the jaw open (lateral pterygoid muscle). |
|
|
CN XII |
Hypoglossal nerve Paresis of the hypoglossal nerve results in ipsilateral deviation of the protruded tongue to the side of weakness and associated ipsilateral atrophy of the tongue. |
|
|
When tone is increased, it is important to differentiate spasticity from rigidity. |
When tone is increased, it is important to differentiate spasticity from rigidity. Spasticity results from damage to the descending corticospinal or pyramidal tracts, whereas rigidity results from damage to the basal ganglia. Spasticity is the hallmark of an upper motor neuron lesion (pyramidal tract injury) and results in a characteristic pattern of increased tone in the extremities—flexion of the upper extrem- ities and extension of the lower extremities. |
|
|
Clasp knife phenomenon (spasticity sign) |
It is velocity dependent! Initial resistance to passive movement of the joint, followed by sudden reduction in tone allowing the limb to move freely and unrestricted through the rest of the range of movement for that joint). |
|
|
Upper motor neurons lesion |
1. Hyperreflexia 2. Babinski’s response (extensor toe) 3. +/- clonus 4. spasticity. |
|
|
Spasticity in infants 👶 |
Spasticity typically develops over the course of the first year of life in an infant as myelination of the white matter tracts occurs, and in the first few months of life, upper motor neuron lesion of the infant may result in hypotonia before hypertonia develops. Early hand preference (i.e., a strong hand preference before 12–18 months of age) is abnormal and is generally indicative of weakness or impairment of the opposite arm. |
|
|
Rigidity |
Rigidity results in increased tone in all directions of movement of the joint that is not velocity- dependent (so-called lead pipe rigidity). Resistance is present in both agonist and antagonist muscles. |
|
|
Cogwheel rigidity |
Cogwheel rigidity is present when there is a tremor superimposed on the rigidity, giving a “ratchet” feeling to the increased tone. |
|
|
Lower motor neurons lesion |
1. Hypotonia or flaccidity is decreased or absent resistance of passive movement of a limb ( or cerebellar/cerebellar pathway lesions). 2. Hyporeflexia/areflexia and hyperextensibility of the joint. 3. Muscle wasting 4. fasciculation may also be seen. |
|
|
Disorders or lesions of the cerebellar hemispheres- |
1. ipsilateral appendicular ataxia 2. dysmetria (impaired judgment of distance with past pointing), 3. dysdiadochokinesia (abnormal or impaired rapid alternating movements). |
|
|
Disorders or lesions of the cerebellar hemispheres- |
1. ipsilateral appendicular ataxia 2. dysmetria (impaired judgment of distance with past pointing), 3. dysdiadochokinesia (abnormal or impaired rapid alternating movements). 4. Intention or action tremor |
|
|
Midline lesions of cerebellum- |
produce gait and truncal ataxia. |
|
|
To be certain that the ataxia is of cerebellar origin, |
proprioceptive loss has to be excluded; *** The Romberg sign (positive test) removes the visual and vestibular components that contribute to maintaining balance and can thus identify a proprioception-related neurologic disease. |
|
|
Cerebellar lesions |
1.Gait ataxia- stand with the feet wide apart for stability and sways side to side with walking, often falling to the side of the lesion (if unilateral). 2.Impairment of the visual pathways with resultant nystagmus (maximal toward side of lesion) 3. impairment of speech (scanning dysarthria and staccato speech) are often accompaniments to cerebellar lesions. |
|
|
Walking in children timing |
Walking is typically achieved by 12 to 18 months of age with fast walking and running by 18 to 24 months of age. |
|
|
Involuntary movements |
Damage or dysfunction of the basal ganglia results in involuntary movements (dyskinesias) that may be broadly classified into either an excess of move- ments (hyperkinesia) or a paucity of voluntary movements (hypokinesia) unrelated to weakness or spasticity. Collectively, these movements are known as extrapyramidal symptoms. |
|
|
Hyperkinetic movements include: |
Extra pyramidal symptoms (basal ganglia damage) 1. Chorea 2. Athetosis 3. Tremors 4. Ballismus 5. Dystonia (sustained or intermittent muscle contractions causing abnormal movements and posture of the limbs, trunk, or neck). 6. Tics 7.Myoclonus-sudden, brief,rapid involuntary jerking of a muscle or group of muscles; may be focal, multifocal, or generalized. |
|
|
Hypokinetic movements include: |
Extra pyramidal symptoms (basal ganglia damage) 1. Bradykinesia (slowness of movement). 2. Akinesia (difficulty initiating and terminating movement). 3. Rigidity (stiffness and/or inflexibility of a limb or trunk). |
|
|
Sensory systems |
— Primary sensory testing includes assessment of 1. pain, temperature and crude touch (spinothalamic tracts) 2. proprioception and vibration (dorsal columns). Cortical sensory modalities include graphesthesia, two-point discrimination, and stereognosis, tactile localization (extinction), and point localization—- Parietal lobe |
|
|
Gerstmanm syndrome |
Gerstmann’s syndrome is caused by specific brain lesions which affect the posterior lobule of the parietal lobe in the dominant hemisphere resulting in tetrad of symptoms which include 1. acalculia 2. finger agnosia 3. agraphia 4. left-right disorientation |
|
|
Atlas ? Axis ? |
Atlas -C1 Axis- C2 |
|
|
Fasciculus gracilis ? cuneatus? |
Gracilis - below T6 Cueatus- above T6 |
|
|
Anterior and lateral spinothalamic tracts?? |
Pain and temperature fibers enter the lateral spinothalamic tract. Light touch and pressure fibers enter the anterior spinothalamic tract |
|
|
Hypercapnia CO2 rentation |
Due to hypoventilation. Result in cerebral vasodilation which lead increase CBF and ICP |
|
|
Hypercapnia CO2 rentation |
Due to hypoventilation. Result in cerebral vasodilation which lead increase CBF and ICP |
|
|
Hypocapnia |
Due to hyperventilation. Result in cerebral vasoconstriction which decreases CBF and thus ICP |
|
|
Pleomorphic Xanthoastrocytomas |
-WHO II (worst outcome than LGG). -PXAs with anaplastic features have been described and tend to have worse outcome. -very rare. ~1% of all pedis brain tumors. -peripheral or cortical mass com- posed of cystic and solid components and hetero- geneous enhancement. - must have staging with neuroaxis. -have the highest frequency of BRAF V600E mutations out of all CNS neoplasms. -GTR is the primary goal as it is a strong predictor of PFS. -PXAs have very variable outcome. Five-year PFS is reported to be 40 to 68% and 5-year OS rate is 76 to 87%. -There has been no difference in pediatric PXA with and without anaplastic features regarding outcome. Prognosis is overall worse in children than in adults |
|
|
Atypical Teratoid Rhabdoid Tumors |
-Part of group of embryonal tumors. -Highly malignant. -Mostly in infants. Around 80% of the patients diagnosed with ATRT are children younger than 3 years. - 50% infra, 50% supratentorial. -A supratentorial tumor with a thick, wavy (irregular) heterogeneously enhancing wall sur- rounding a central cystic region is suggestive of ATRT,as it is a distinctive and unusual pattern. -Neuroaxis MRI mandatory. -The main histologic characteristics of rhabdoid tumor cells are abundant cytoplasm with juxtanuclear eosi- nophilic inclusions and nuclei that display a sin- gle, prominent nucleolus in clear, uncondensed chromatin. ● SMARCB1. A defect in the INI 1 gene (SMARCB1) leading to loss of expression is associated with rhabdoid tumors and is used for diagnosis. *** Those tumors that do not have alterations of either INI1 or BRG1 are classified as embryonal tumors with rhabdoid features. -5-year survival is 28%. -The median OS is about 10 months and metastatic disease correlates with a worse prognosis. |
|
|
Desmoplastic Neuroepithelial Tumors |
-The presenting symptom is often seizures. characteristically, it causes intractable partial seizures. -DNET is a grade I glioneuronal tumor -DNETs are characterized as hav- ing a “bubbly” appearance, are multilobulated, are hypointense on T1 in a wedge-shaped configura- tion, and hyperintense on T2-weighted images. FLAIR imaging shows a characteristic bright rim. -DNETs have one of the highest ADC values among benign tumors. (Meaning they facilitate diffusion = bright). -surgery is curative if can be completely resected. |
|
|
Gangliogliomas |
- Seizures are the most common presentation. -Two different cell types (combination of neuronal and glial cell). - mostly Who I. Rarely can be anaplastic WHo III - very good prognosis with GTR. -The majority of gangliogliomas are localized in the temporal lobe, but can occur throughout the CNS. -Well-differentiated, slow-growing neuroepithelial tumor composed of neoplastic, mature ganglion cells alone (gangliocytoma) or in combination with neoplastic glial cells (ganglioglioma). -Five-year PFS rate is 81.2% and the OS rate is 97.4%. |
|
|
Interesting about NF2 |
After vestibular schwannoma, the next most common tumor type in NF2 is meningioma, which is encountered in roughly half of the cases. |
|
|
BRAF mutation |
Pleomorphic xan- thoastrocytoma (PXA), ganglioglioma, and a small subset of extracerebellar PA have BRAF V600E mutations. |
|
|
Supratentorial LGG |
The aim of surgery in supratentorial hemispheric LGGs is GTR. If GTR cannot be achieved, further surveillance is indicated, as residual disease can be stable (progression-free disease) in up to 55%. |
|
|
Most common type of craniopharyngiomas in Pedis |
Adamantinomatous tumors are the most common subtype, particularly in the pediatric population.
These tumors are characterized by keratinized cells that face a cyst lumen, and “wet” keratin nodules consisting of desquamated epithelial cells. The nodules may become calcified over time. The cystic regions of adamantinomatous craniopharyngiomas contain fluid with a “motor oil” consistency, rich in cholesterol. |
|
|
Above the red nucleus |
Lesions above the red nucleus produce decorticate posturing: flexion of upper limbs and extension of lower, rubrospinal tract function. M3 |
|
|
Decorticate posturing |
Lesions above the red nucleus produce decorticate posturing: flexion of upper limbs and extension of lower, rubrospinal tract function. |
|
|
Decorticate posturing |
Lesions above the red nucleus produce decorticate posturing: flexion of upper limbs and extension of lower, rubrospinal tract function. |
|
|
Lesions Below red nucleus |
Those below the red nucleus produce decerebrate posturing: extension in upper and lower limbs, vestibulospinal tract function. Normal flexion (M4) constitutes flexion with supinatio |
|
|
Decorticate posturing |
Lesions above the red nucleus produce decorticate posturing: flexion of upper limbs and extension of lower, rubrospinal tract function. M3 |
|
|
Lesions Below red nucleus |
Those below the red nucleus produce decerebrate posturing: extension in upper and lower limbs, vestibulospinal tract function. M2 |
|
|
Decerebrate posturing |
Those below the red nucleus produce decerebrate posturing: extension in upper and lower limbs, vestibulospinal tract function. M2 |
|
|
Which one of the GCS components differentiate the severity of the injury? |
Of the three divisions (eye opening, verbal response, and motor response) the motor response is most likely to differentiate the severity of injury. |
|
|
Gerstmann’s syndrome |
Lesions of the dominant parietal lobe . It includes tetrad of symptoms : 1. impairment in performing calculations (acalculia). 2. discriminating their own fingers (finger agnosia). 3. writing by hands (agraphia). 4. impairment of distinguishing left from right (left-right disorientation). |
|
|
Contralateral neglect |
Non dominant parietal lobe lesion. Usually left side neglect due to right side lesion. |

