![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
the GIT has to deal with a lot of bad stuff. How does it protect itself? |
puts out mucus has semipermeable epithelial sheet to keep some things out has junctional complexes in between cells |
|
|
layers and sublayers of the general architecture of GIT |
mucosa: epithelium, lamina propria, muscularis mucosa
submucosa
muscularis externa: inner circular and outer longitudinal. myenteric parasymp plexus between the two
serosa/adventitia: adventitial CT holding to adjacent viscera and serosa smooth mesothelial later to support with vascular and lymphatics |
|
|
different regions of mucosa |
epithelium: invaginates wall as glands, evaginates into lumen as villi
lumina propria: loose CT
muscularis mucosa: inner circular and outer longitudinal smooth muscle |
|
|
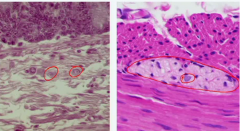
large pale nucleus indictes nerve cell
L: Meissner's or submucosal plexus
R: Auerbach's or myenteric plexus |
|
|
what is the epithelium like in esophagus?
what unique features to esophagus? |
nonkeratinizing, stratified squamous epithelium with thick BM and numerous mitotic figures lamina propria has papillary insertions to epithelium and cardiac glands throughout length of Eso muscularis muscosae is all longitudinal arranged and not in upper 1/3 of eso
submucosa has folds to allow dilation during swallowing. Has submucosal glands for mucus along entire length
muscularis externa: upper 1/3 eso skeletal, middle 1/3 mixed, lower 1/3 smooth
has adventitia but no mesothelial layer |
|
|
why is the esophagus graded in the skeletal and smooth muscle composition of the muscularis externa? |
swallowing is initiated voluntarily but has to be completed by autonomics |
|
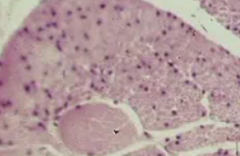
type of muscle |
upper portion smooth muscle
lower portion skeletal |
|
|
what functions does the stomach serve |
storage
digestion with HCl, protein breakdown, chyme
absorption of amino acids, alcohol, water |
|
|
what is unique about the stomach lining? |
surface epithelial are simple columnar and invaginate to gastric pits which are continuous with mucosal glands in mucosa lamina propria: almost nonexistent since tightly packed mucosal glands, is between gastric pits muscularis mucosa: has the two distinct layers
muscularis externa: has 3 layers, inner most obliquely-oriented, then middle, and longitudinal. Pyloric sphincter is thickened region of the circular layer
serosa: simple squamous epithelium = mesothelium, serous secreting |
|
|
what are the different regions of a gastric/fundic gland |
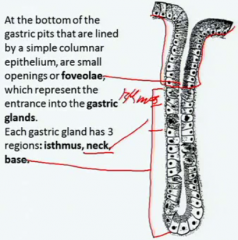
surface: simple columnar. Neck secrete acid. parietal (oxyntic) cells also in neck: secrete HCl and intrinsic factor. Base: chief cells making pepsinogen |
|
|
what controls activity of gastric gland? |
secretin and vagus nerve |
|
|
what does intrinsic factor do |
it's for vit B12 absorption |
|
|
how does the stomach keep from getting eaten by itself? |
surface mucous cells - the simple columnar ones in the gastric pit- secrete a neutral mucous |
|
|
entero endocrine cells general
in stomach |
throughout epithelium of stomach to colon, near the base. Local control of digestive processes using hormones- making it largest endocrine organ in body.
Unicellular galnds that secrete basically in paracine fashion into underlying capillaries. Some go to lumen "open type cells" or not "closed type cells"
in stomach: gastrin producing cells stimulate acid and pepsinogen. Somatostatin producing cells inhibit gastrin release, reducing pepsinogen and acid |
|
|
functions of the small intestine |
transports chyme completes digestion absorption of nutrients secretion of hormones |
|
|
small intestine special histo in mucosa |
mucosa specialized to increase SA plicae circularis: semicircular folds into lumen esp jejunum. Have submucosa core villi: outgrowths epithelium and lamina propria, loose CT core and lymphatic lacteal. Muscularis mucosae not in the villi
enterocytes, tall columnar cells covered with microvilli. Use junctional complexes.
intestinal glands= crypts of Lieberkuhn: invaginations of epithelium to lamina propria. |
|
|
how does the intestine maintain the cells |
cells migrate towards apex of villi and are sloughed up. Coming up out of the crypts that have stem cells. |
|
|
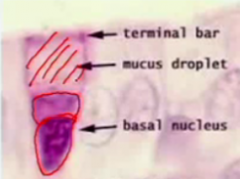
goblet cell
sit in between absorptive cells, increasing in number from duodenum to ileum
secrete acidic mucous, lubricating wall, protecting from pancreatic enzymes and bacteria. Secretion product is 80% carb, 20% protein |
|
|
paneth cells |
live in base of crypts
have secretory granules- acidophilic. Have lysozyme as antibacterial as well as TNF-alpha and defensins |
|
|
what do the enteroendocrine cells release in the intestine? |
cholecystekinin CCK to increase pancreatic enzyme secretion and gallbladder contraction and slow gastric emptying via pyloric sphincter
gastric inhibitory peptide GIP decreases gastric acid production and inhibits motilin which increases gut motility
secretin: in response to acid and fatty acids for bicarbonate release from pancreas and enhances insulin secretion from beta cells in islets of Langerhans |
|
|
how are different nutrients taken into the cell
amino acids monosaccharides small lipids larger molecules
where do these get dumped? |
aa and ms by facilitated diffusion
small lipids diffuse
pinocytosis
put out into blood and lymph |
|
|
what happens to lipids inside enterocytes |
made into triglycerides in the sER and put into chylomicrons which are put into vesicles at golgi apparatus and moved to basolateral plasma for exocytosis into lymphatic apillaires |
|
|
in intestine how are the non-mucosa layers like |
lamina propria has increased amounts of lymphoid tissue the further along since increased epithelial permeability
submucosa: duodenum has elaborate submucosal glands of Brunner that secrete alkaline fluid to raise pH. |
|
|
what is the function of the muscularis externa like in the intestine |
mixing contractions 10/min peristaltic contractions 3-10/hr
distension initiates activity |
|
|
how do you tell the duodenum jejunum and ileum apart |
Brunner's glands in submucosa
tallest plicae
peyer's patches
goblet cells and lymphatic structures increase further along, so more in ileum. |
|
|
what is the function of the large intestine |
storage water resorption complete digestion via bacterial flora |
|
|
unique histo of bowel |
no villi increased mucus secretion- more goblet cells prox to distal
no paneth cells.
outer longitudinal muscle in muscularis externa is in 3 bands = taeniae coli that shorten length |
|
|
unique histo of veriform appendix |
no villi
complete ring of lymphoid nodules in lamina propria
outer longitudinal muscle of ME is a complete layer |

