![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
72 Cards in this Set
- Front
- Back
|
The nerve which supplies the lobule of the ear is the |
A
From Anatomy for Anaesthetists: "The great auricular nerve (C2, 3) is the largest cutaneous branch of the cervical plexus. It hooks around the mid-point of the posterior border of sternocleidomastoid, then passes across it in the direction of the angle of the mandible. On this muscle it breaks up into three terminal branches. 1. Auricular - supplying the lower two-thirds of the medial aspect of the external ear and the lateral surface of the lobule. 2. Mastoid - to the skin over the mastoid process. 3. Facial - to the skin over the masseter and the parotid gland." |
|
|
Fibres contained in the recurrent laryngeal nerve include
A. motor supply to the crico-thyroid muscles B. motor supply to the crico-arytenoid muscles C. sensory fibres from the epiglottis D. sensory fibres from the crico-thyroid joint E. sensory fibres from the supra-glottic mucosa |
B
"The recurrent laryngeal nerves provide the motor supply to the intrinsic muscles of the larynx apart from cricothyroid, as well as the sensory supply to the laryngeal mucosa inferior to the vocal cords." |
|
|
At the wrist joint
A. the median nerve lies between the tendons of palmaris longus and flexor carpi radialis B. the median nerve lies medial to the tendon of flexor carpi ulnaris C. the radial artery is usually palpable just medial to the tendon of flexor carpi radialis D. the ulnar artery and nerve enter the hand by passing deep to the flexor retinaculum |
A
• A. True • B. False - see above • C. False - lateral to FCR • D. False - superficial to FR |
|
|
The largest and most direct branch of the internal carotid
artery is the A. ophthalmic B. anterior cerebral C. middle cerebral D. posterior cerebral E. choroidal |
C
"The middle cerebral artery is the larger terminal branch of the internal carotid." (Gray's Anatomy 39thed) |
|
|
A 50 year old patient is admitted with acute chest pain. An
ECG shows tall R waves in lead Vi. The most likely diagnosis is A. occlusion of the anterior descending coronary artery B. a lateral myocardial infarction C. pulmonary infarction D. posterior myocardial infarction E. occlusion of the circumflex artery |
D
D probably the most classically correct answer • A - False. LAD occlusion-> infarction of anterior/anterolateral wall LV + anterior 2/3 of septum -> changes in praecordial leads V2-V4/5/6 + I, aVL. • B - False. • C - True. Pulmonary infarction (PE) can cause tall R wave in V1, if large PE with R strain • D - True. Posterior MI may produce tall R wave in V1. Most likely option. • E - True. LCX supplies posterolateral wall of LV and infarction may produce tall R wave in V1 Some causes of a dominant R wave in lead V1: • Dextrocardia • Normal variant • Misplaced electrodes • Posterior myocardial infarction • Right bundle branch block • Right ventricular hypertrophy • Wolff-Parkinson-White syndrome with a left-sided accessory pathway |
|
|
Sickle cell disease (homozygous haemoglobin SS) is
frequently associated with A. cardiomyopathy B. chronic respiratory dysfunction C. nephropathy D. peripheral neuropathy E. all of the above |
E
Cant find specific reference for D, but the rest are true so must be E Stoelting: • Sickle cell anemia, the homozygous form of Hb S disease, presents early in life with a severe hemolytic anemia and vaso-occlusive disease involving the marrow, spleen, kidney, and central nervous system • Recurrent splenic infarction culminating in loss of splenic function in the first decade of life • The renal medulla is another prime target, with loss of concentrating ability an early feature of the disease progressing to chronic renal failure usually in the third or fourth decade of life • Lung damage results from chronic progressive lung damage due to persistent inflammatory reactions punctuated by acute chest syndrome, a pneumonia-like complication characterized by a new pulmonary infiltrate involving at least one complete lung segment and at least one of the following: chest pain, fever higher than 38.5°C, tachypnea, wheezing, or cough • Neurologic complications may include stroke, usually infarctive in adolescence and hemorrhagic later in adult life Harrisons: • "A sickle cell cardiomyopathy and/or premature coronary artery disease may compromise cardiac function in later years |
|
|
During an epidural block, an indication that all
sympathetic cardio-accelerator fibres have been blocked would be an upper sensory level at the A. tip of the xiphoid B. nipple line C. apex of the axilla D. inner aspect of the upper arm E. little finger |
E
Little finger = C8 dermatome, so if have a sensory level at C8 you know you have blocked T1 and below. Cardio-acceleratory fibres arise from T1-T4. |
|
|
Established Legionnaires' disease is best treated with
A. aminoglycosides B. cephalosporins C. chloramphenicol D. crystalline penicillin E. erythromycin |
E
• Erythromycin (plus rifampicin if severe) • "Historically, erythromycin was used for L pneumophila infection, but doxycycline, azithromycin, macrolides, and quinolones are more active against legionnaires disease (LD) than erythromycin." Emedicine - Infectious diseases. • "Treatment is with erythromycin; 4-quinolones (i.e. nalidixic acid, ciprofloxacin, norfloxacin) have also been used." Yentis, 3d. ed., p.316. |
|
|
In infants with congenital pyloric stenosis
A. dehydration is associated with early hyponatremia B. plasma chloride levels seldom fall below 85 mmo1.1-1 C. renal conservation of hydrogen and potassium ions occurs D. the urine is initially alkaline, then may become acidic E. vomiting causes a loss of potassium ions |
D
Anaesthesia & Intensive Care Medicine Volume 9, Issue 4, April 2008: "Vomiting normally results in equal loss of gastric acid and alkaline duodenal fluid. However, with gastric outlet obstruction, gastric acid along with a variable amount of Na+ and K+ is lost in vomitus without loss of HCO3− from the duodenum. The resultant systemic alkalosis overwhelms the capacity of the proximal convoluted tubule to reabsorb HCO3−, producing an alkaline urine. As extracellular fluid volume depletion increases, aldosterone is secreted, leading to renal conservation of Na+ in exchange for K+. Eventually hypokalaemia forces Na+ exchange preferentially with H+ instead of K+ in the renal tubules. This produces the characteristic ‘paradoxical acid urine’ in the face of systemic alkalosis." |
|
|
A 7 year old 30 kg. boy was booked for repair of an inguinal
hernia. He was noted to have muscular looking arms and legs. Following midazolam premedication anaesthesia was induced with thiopentone intravenously and N20/02 by mask. Airway difficulties led to his being given 30 mg. of suxamethonium. He showed vigorous fasiculation followed by generalised muscular rigidity. The rigidity persisted despite another 30 mg. of suxamethonium intravenously. The probable cause of this response to suxamethonium is A. atypical pseudocholinesterase B. Duchenne's muscular dystrophy C. familial periodic paralysis D. hyperkalaemia E. myotonia congenita |
E
From OHA p. 308: "Myotonia Congenita (Thomsen's disease): Defective skeletal muscle chloride channel (failure of muscle relaxation), widespread dystrophy and/or hypertrophy, unresponsive to non-depolarising muscle relaxants, palatopharyngeal dysfunction, aspiration risk, cardiomyopathy, no apparent association with MH, can be precipitated by cold/durgery/diathermy/anticholinesterases, suxamethonium may cause myotonia with difficult intubation/ventilation." |
|
|
Anti-retroviral agents for HIV infection include
A. nucleoside r-transcriptase inhibitors (NRTIs) which are associated with diarrhoea and intravascular volume depletion B. protease inhibitors which have important effects on the cytochrome P450 system C. non-nucleoside r-transcriptase inhibitors (N-NRTIs) which may cause elevations in liver function tests D. protease inhibitors which can lead to problematic hypoglycaemia |
B, A and C all also seem true
Repeat of an old type K question (selected A, B & C then) HAART = Highly active anti-retroviral therapy = 3 drugs including a protease inhibitor. Nucleoside reverse transcriptase inhibitor: - zidovudine, didanosine, lamivudine, zalcitabine - SEs: GI upset -> volume depletion, incr LFT, anemia, neutropenia, neuropathy, pancreatitis Non-nucleoside reverse transcriptase inhibitor: - etavirenz, nevirapine - SE: incr LFT, dizzeness, vivid dreams Protease inhibitors: - saquinavir, indinavir, ritonavir - SE: P450 inhibition (thus caution with benzos & opioids), GI upset, incr LF |
|
|
The lowest incidence of pneumothorax following
supraclavicular brachial plexus block will be achieved by A. placing the patient in the head down position during insertion of the needle B. preventing entry of air through the needle C. asking the patient to breath-hold during insertion of the needle D. using a short fine-gauge needle E. taking routine chest x-rays |
D
The only thing suggested to reduce the risk is operator experience. Perhaps safer if you use a short, fine guage needle. Routine CXR is not justified (Miller). Miller online: • The three trunks are clustered vertically over the first rib cephaloposterior to the subclavian artery, which can often be palpated in a slender, relaxed patient. The neurovascular bundle lies inferior to the clavicle at about its midpoint. The first rib acts as a medial barrier to the needle's reaching the pleural dome and is short, broad, and flat, with an anteroposterior orientation at the site of the plexus. • The patient is placed in a supine position, with the head turned away from the side to be blocked. The arm to be anesthetized should be adducted, and the hand should be extended along the side toward the ipsilateral knee as far as possible. In the classic technique, the midpoint of the clavicle should be identified and marked. The posterior border of the sternocleidomastoid can be easily palpated when the patient raises the head slightly. The palpating fingers can then roll over the belly of the anterior scalene muscle into the interscalene groove, where a mark should be made approximately 1.5 to 2.0 cm posterior to the midpoint of the clavicle. Palpation of the subclavian artery at this site confirms the landmark • A 22-gauge, 4-cm needle is directed in a caudad, slightly medial, and posterior direction until a paresthesia or motor response is elicited or the first rib is encountered. If the first rib is encountered without elicitation of a paresthesia, the needle can be systematically walked anteriorly and posteriorly along the rib until the plexus or the subclavian artery is located • The modified, plumb-bob approach uses similar patient positioning, although the needle entry site is at the point at which the lateral border of the sternocleidomastoid muscle inserts into the clavicle. The needle is inserted while mimicking a plumb-bob suspended over the needle entry site. This reduces the risk of pneumothorax. |
|
|
In a normal pregnant woman laboratory tests would show
A. an arterial pH of 7.4 B. an increase in functional residual capacity (FRC) C. decreased oxygen consumption D. an arterial base excess of +5 mmo1.1-1 E. a PaCO2 of 50 mmHg |
A
• A - True. "The bicarbonate level is typically reduced enough to return arterial pH to within the normal range." Brandis, Revised Edition, p. 249. • B - False. "Decreased FRC in pregnancy due to decreased RV and ERV." Brandis, Revised Edition, p. 248. • C - False. "Oxygen consumption at term is 20% higher than the pre-pregnant value." Brandis, Revised Edition, p. 249. • D - False. ". . . and base excess decreases to 3.0mEq per L." Bonica's Management of Pain By Loeser et al. p. 1395. Edition: 3, Published by Lippincott Williams & Wilkins, 2001 • E - False. "At term the arterial pCO2 is about 32 mmHg" Brandis, Revised Edition, p. 249. |
|
The following capnograph tracing is most likely to represent
A. partial obstruction of sampling tube B. sticking ventilator bellows C. incomplete neuromuscular blockade D. air entrainment into sampling tube E. partial obstruction of endotracheal tube |
D
Entrainment of air into sample line → normal flat plateau with terminal peak just before inspiration End-tidal CO2 excretion waveform and error with gas sampling line leak. Anesth Analg 1988;67: "In summary, when there is a loose connection between an end-tidal CO, sampling line and the CO, analyzer (Saracap), the CO, excretion waveform is very unusual and consists of a long plateau followed by a brief peak, rather than the usual square CO, excretion waveform. The long CO, plateau is caused by entrainment of room air through the leaky connection by the continuous CO, analyzer suction, and the brief CO, peak is caused by the next PIP, which transiently pushes undiluted end-tidal gas through the sampling line into the CO, analyzer. Because the 0, and N,O values digitally displayed by the Saracap are mean exhalation values, the 0, and N20 concentrations are a function of both the size of the leak and the PIP." |
|
|
A patient suddenly collapses 36 hours after gastrectomy.
His blood pressure is 80/30 mmHg, his pulse rate 100/minute, his central venous pressure +2 cm (from the sternal angle) and his temperature 39°C. The most likely diagnosis is A. acute dilatation of the stomach B. anastomotic disruption C. haemorrhage D. pulmonary embolism E. septicaemia |
B
E true too, but because of B |
|
|
The diagram below represents a transgastric short axis view
of the heart obtained using transoesphageal echocardiography. The structure labelled A is the A. anterolateral papillary muscle B. non-coronary leaflet of the aortic valve C. posterior mitral valve commissure D. posterolateral papillary muscle E. posteromedial papillary muscle |
E
This structure is the posteromedial papillary muscle. The other shaded bulge transected by the horizontal (0 to 180 degrees) line is the anterolateral papillary muscle. |
|
|
Major complications of mediastinoscopy include all of the
following EXCEPT A. compression of great vessels B. air embolism C. pneumothorax D. major haemorrhage E. phrenic nerve damage |
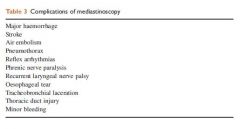
A
Comperssion of brachiocephalic artery can occur |
|
|
A patient has a history of polyuria and has an elevated
serum calcium, normal parathyroid hormone level and an elevated serum angiotensin converting enzyme level. The most likely diagnosis is A. milk alkali syndrome B. primary hyperparathyroidism C. malignancy D. sarcoidosis E. multiple myeloma |
D
A: False – hyperCa, alkalaemia, renal insufficiency. Caused by excessive intake of milk (vit D, Ca), and alkali (NaHCO3, MgCO3) usually by patients with peptic ulcers. The alkalosis decr the urinary excretion of Ca. B: False. Would have elevated PTH (can be normal). No effect on ACE C: False. HyperCa > 3.5mmol/L (often), plasma PTH low/ suppressed. A normal or elevated PTH conc virtually excludes malignancy as a cause of hyperCa D: Trueish. 10-20% get hypercalcaemia. Although PTH is often suppressed. Elevated ACE in 75% of cases. serum ACE is a possible marker of active sarcoidosis, and hypercalcaemia is consistent. E. ??Trueish. Hypercalcaemia suppresses PTH. An example of a haematological malignancy in which hyperCa appears only with metastatic bone involvement. |
|
|
When providing general anaesthesia to a patient with a
history of asthma A. thiopentone should NOT be used as it may cause bronchospasm B. intravenous and topical tracheal lignocaine are equally effective in preventing bronchial hyperreactivity C. ketamine provides little benefit in a patient with active wheezing D. induction with propofol is effective in reducing the incidence of wheezing following intubation E. isoflurane is as effective a bronchodilator as halothane when given in MAC equivalent doses |
D
|
|
|
In pregnant patients with kyphoscoliosis
A. Harrington rods (or equivalent) are an absolute contraindication to administration of epidural analgesia or anaesthesia B. thoracic cage deformity severe enough to reduce vital capacity below one litre is not usually compatible with a successful fetal outcome C. the severity of the extra-pulmonary restrictive pattern of pulmonary function is inversely proportional to the scoliosis angle D. of the idiopathic type, there is an association with symptomatic mitral valve prolapse E. there is a risk of progression of the scoliosis with consequent reduction in lung volumes |
B
A - false: not an absolute contraindication, but may lead to failure or inadequate analgesia/anaesthesia and increased risk of dural puncture. B- True: "As a rule, patients with severe restrictive lung disease (i.e., vital capacity < 1 L) should be advised to avoid pregnancy or consider therapeutic abortion." but from Oxford Specialist Handbooks Obstetric Anaesthesia Pg 104. "successful pregnancy is possible in patients with severe disease and a vital capacity of as little as 1000mL" and mechanical ventilation has been used in this group of patient with success. C- the wording of "inversely proportional" seems wrong. Angle increase as scoliosis worsens. severity of pulmonary restriction should be directly proportional? Lung volume is inversely proportional to the Cobb's angle. D - false: 25% can have association with asymptomatic MVP E- false. Pregnancy does not appear to affect curve progression. Nor does scoliosis appear to affect pregnancy outcome [8]. Although early studies suggested that scoliotic curves progressed during pregnancy, subsequent studies have demonstrated otherwise. UpToDate |
|
|
Correct statements regarding chronic fatigue syndrome are
that A. cognitive behavioral therapy is a primary treatment of the condition B. it is associated with alcohol abuse (> 40g/day) C. it is associated with morbid obesity (BMI > 30) D. it is a major depressive disorder E. SSRIs (selective seretonin re-uptake inhibitors) are the mainstay of treatment |
A
"CBT and graded exercise therapy (GET) are the only interventions found to be beneficial." Lancet 2006; 367: 346–55 |
|
|
In the treatment of phantom limb pain
A. calcitonin infusion is NOT effective B. gabapentin reduces the pain C. intravenous lignocaine reduces the pain D. ketamine provides long-term pain relief E. opiates are NOT effective |
B
Key messages - Pain Book 2010. p.240 1. Continuous regional blockade via nerve sheath catheters provides effective postoperative analgesia after amputation, but has no preventive effect on phantom limb pain 2. Calcitonin, morphine, ketamine, gabapentin, amitriptyline and tramadol reduce phantom limb pain 3. Sensory discrimination training and motor imagery reduce chronic phantom limb pain 4. Ketamine, lignocaine (lidocaine), tramadol and amitriptyline reduce stump pain 5. Perioperative epidural analgesia reduces the incidence of severe phantom limb pain |
|
|
Which statement about the use of Entropy depth of
anaesthesia monitoring is true? A. artefacts caused by cardiac pacemakers produce a high RE (Response entropy) value B. RE only assesses the EEG (electroencephalogram) range from 32-47Hz (high frequency) C. SE (State entropy) values range from 0-100 D. SE is a stable indicator of the effect of hypnotics on the cortex E. the RE algorithm filters the EMG (electromyogram) component |
D
Filters out - ECG, pacer, movement, cautery Includes - EEG, EMG SE 0 to 91, takes in 0.8 to 32Hz RE 0 to 100, takes in 0.8 to 47 Hz |
|
|
Following one-lung ventilation there is an increased risk of
lung injury if plateau airway pressure (during one-lung ventilation) exceeds A. 20 cm water B. 30 cm water C. 40 cm water D. 50 cm water E. lung injury is not related to ventilation pressure |
B
According to One-lung anaesthesia. BJA CEPD Reviews. Vol2(3) 2002. |
|
|
A 30-year-old man presents to the Emergency Department
following a high speed motor vehicle accident. He has a Glasgow Coma Score of 7 and arrives with a cervical collar in situ and an 18 gauge intravenous cannula in his right hand. You first priority in managing this patient would be to A. insert a large bore intravenous cannula B. perform a CAT scan of the brain C. perform a cervical spine X-ray D. perform a plain chest and pelvic X-ray E. secure the airway with an endotracheal tube |
E
GCS<8; Secure airway with in-line C-spine imobilisation |
|
|
A fifty-five-year-old man on antihypertensive medication,
including an ACE (angiotensin-converting enzyme) inhibitor, has a total knee replacement. Red cell transfusion is begun in recovery through a leukocyte reduction filter after brisk bleeding into his drains. A recognised complication of the use of this filter in this situation is A. air embolism B. clotting factor depletion C. haemolysis D. increased risk of postoperative infection E. severe hypotension |
E
Contact activation results in BradyKinin release. Together with ACE-i, leads to high levels of BK (lack of breakdown); thus leading to hypotension. From FDA - Hypotension and Bedside Leukocyte Reduction Filters: Since 1994, FDA has received over 80 reports of patients developing significant hypotensive events while receiving blood products transfused through a bedside leukocyte reduction filter. It is estimated that approximately 20 million bedside leukocyte reduction filters were used during this period. Although some sources have attributed several of these events to the use of angiotensin converting enzyme (ACE) inhibitors and the use of negatively charged filter surfaces, FDA’s analysis of these reports indicated that neither ACE inhibitor therapy nor exposure to negatively charged filter surfaces were consistently associated with these events. The reactions occurred with a variety of blood products, although the majority of events occurred during platelet transfusions. The common variable in almost all of the hypotensive events appeared to be bedside leukocyte reduction filtration. A review of the literature indicates that many authors believe these reactions occur more frequently in patients receiving ACE inhibitor therapy. It is hypothesized that these reactions are due to the ACE inhibitors' tendency to retard degradation of bradykinin, a potent vasodilator. Some authors have shown evidence that bradykinin may be generated as a result of filtration at room temperature or when the storage period for filtered blood is insufficient to inactivate bradykinin. Others have discussed the possibility that these reactions occur when the negatively charged membranes in these filters activate Factor XII, one of the blood clotting factors, which triggers a production of bradykinin. However, there have also been adverse events reported with the use of positively charged filters. |
|
|
A common finding in hereditary prolonged QT syndrome is
A. bifid T waves B. inverted P waves C. prolonged QRS duration D. right axis deviation E. short PR interval |
A
T wave and U wave abnormalities are common in LQTS. T waves may be larger, prolonged, or have a notched, bifid or biphasic appearance. A pathognomonic feature of LQTS is so-called T wave alternans, where there is beat-tobeat variation in T wave amplitude. This sign of enhanced electrical instability is a highly specific but very insensitive marker for LQTS |
|
|
A 30-year-old man presents to the Emergency Department
following a high speed motor vehicle accident. He has marked abdominal distension, a pulse rate of 130 and a blood pressure of 80/50 mmHg. The most appropriate initial investigation would be A. abdominal angiogram B. abdominal paracentesis C. CAT scan of the abdomen D. plain X-ray of the abdomen E. FAST (focussed abdominal sonography for trauma) scan |
E
|
|
|
The administration of blood contaminated with Yersinia
Enterocolitica will typically produce symptoms of infection A. during the transfusion B. within 6 hours C. within 12 hours D. within 24 hours E. within a week |
A
Depends on bacterial load of the PRBC and clinical context. But presuming heavy contamination, then clinical features of high temperature, tachycardia and hypotension should begin during transfusion due to gram negative endotoxins |
|
|
The weight of a child can be estimated using the formula
A. (age + 2) x 3 B. (age + 4) x 2 C. (age x 2) + 4 D. (age x 3) + 2 E. age x 4 |
B
From age 1-8: wt= 2(age+4) From age 8-12 wt = (age in years) x 3 Though Archives of Disease in Childhood 2007;92:412-415 concluded: “The formula weight = 2(age+4) underestimated children’s weights by a mean of 18.8%” “This study shows that the current estimation formula provides a significant underestimate of children’s weights. The formula weight(kg) = 3(age)+7 provided a safe and more accurate estimate of the weight of today’s child.” |
|
|
A 60-year-old man with BMI (body mass index) of 30 is
having an inguinal hernia repair. He has a LMA-Proseal® in place and you plan positive pressure ventilation. If the device is properly seated the maximum pressure in cm of water before leaking during positive pressure ventilation should be A. 15 B. 20 C. 30 D. 40 E. 50 |
C
Proseal 30cm H2O (an not exceed 8ml/kg TV), LMA 20cm H2O from the product manual |
|
|
The local anaesthetic agent LEAST likely to cause cardiac
toxicity with inadvertent intravenous injection is A. bupivacaine B. etidocaine C. levo-bupivacaine D. lignocaine E. ropivacaine |
D
Barash Clinical Anaesthesia CVS/CNS Ratios: Bupivicaine 2.0 Etidocaine 4.4 Levo-bupivicaine 2.0 Lignocaine 7.0 Ropivacaine 2.0 Tetracaine 2.0 Mepivacaine 7.1 Prilocaine 3.1 Procaine 3.7 Chloroprocaine 3.7 |
|
|
A previously healthy 20-year-old male is undergoing open
reduction and internal fixation of a fractured tibia. The limb was exsanguinated and the tourniquet appropriately applied and inflated to 250 mmHg prior to surgery. A small amount of continued bleeding is noted after surgical exposure. The tourniquet still seems appropriately inflated. The patient's blood pressure is 110/70 mmHg. You should A. accept that a tourniquet does not stop all bleeding B. check the patient's coagulation profile C. inflate the tourniquet to a higher pressure D. reduce the patient's blood pressure E. re-exsanguinate the limb and re-apply the tourniquet |
E
A is true, but should try E first |
|
|
In severe bupivacaine toxicity, drugs likely to improve the
cardiac conduction abnormalities include A. clonidine B. lignocaine C. ketamine D. metoprolol E. propofol |
A
There are some case reports of clonidine helping: Regional Anesthesia & Pain Medicine:May/June 2007 - Volume 32 - Issue 3 - p 270-271 "Let me bring the use of clonidine to this list of treatments, which is effective in reversing the impairment of ventricular conduction induced by bupivacaine. This electrophysiologic effectiveness was demonstrated in animal models and proved in a clinical case experienced by our team years later, in which a second bolus of 150mcg of i.v. clonidine injected after 55 minutes of resuscitation probably reversed bupivacaine- induced ventricular dysrhythmias." Would think you would want to avoif giving more LA (i.e. Lignocaine) to treat arrhythmia Propofol is not a substitute for intralipid (doses required would cause significant haemodynamic effects) |
|
|
Which of the following contributes the LEAST to motor
neuropathy following the lithotomy position? A. age B. BMI (body mass index) > 25 C. diabetes D. peripheral vascular disease E. smoking |
B
Morgan & Mikhail - High BMI may be protective (padding) From Anesthesiology 2000; 93:938 – Lower Extremity Neuropathies Associated with Lithotomy Positions: A number of patient characteristics (e.g., thin body habitus, history of smoking, diabetes, familial neuropathies, alcoholism; and the presence of subclinical neuropathies or anatomic anomalies), surgical factors (e.g., duration in lithotomy position, use of intrapelvic self-retaining retractors, or positioning of extremities beyond the comfortable range of motion when the patient is awake), and anesthetic techniques (e.g., central-axis needle placement) have been identified as possible risk factors for perioperative lower extremity neuropathies. |
|
|
A new test has been developed to diagnose a disease. To
determine the SPECIFICITY of this new test it should be administered to A. a mixed series of patients i.e. some known to be suffering from the disease and some known to NOT be suffering from it B. a series of patients known to NOT be suffering from the disease C. a series of patients known to NOT be suffering from the disease and an estimate of the prevalence of the disease in the population obtained D. a series of patients known to be suffering from the disease E. a series of patients known to be suffering from the disease and an estimate of the prevalence of the disease in the population obtained |
B
Specificity equals to TN/(TN+FP). Thus only need patients known NOT to have the disease. Any positive result from the new test will be false positives |
|
|
Detrimental post-operative effects of hypothermia following
general anaesthesia in the elderly include each of the following EXCEPT A. delayed emergence B. hypercoagulability C. increased body metabolism D. reduced elimination of anaesthetic agents E. shivering |
B
|
|
|
An 8-year-old boy who is wheelchair bound with cerebral
palsy and spastic quadriplegia is booked for MRI (magnetic resonance imaging), under general anaesthesia for a rapid deterioration in his epilepsy control. On arrival to the MRI suite (with no premedication) he is distressed and inconsolable. Immediate management of this situation should include A. an inhalational induction with parental/carer presence B. cancellation and rescheduling with sedative premedication C. cancellation of procedure until epilepsy is better controlled D. detailed discussion with parents/carer regarding anaesthetic options E. intramuscular or oral ketamine induction |
D
A, B and E all seem like options you could discuss when doing D Presumably C is not an option as the seizures are what is being investigated |
|
|
The Classic laryngeal mask airway (LMA - ClassicTM)
A. contains plasticisers (phthalates), which may be carcinogenic B. involves a significant risk of prion transfer C. is cheaper to use than disposable LMAs D. is less permeable to N20 than disposable LMAs E. may be reused 40 times |

E
BJA Editorial 2006 "The classic laryngeal mask airway: a tried and tested airway. What now?" • A - False - PVC contain Phthalates which are carcinogenic, mutagenic, and reprotoxic • B - False - Worse case scenario of prion disease transmission from an airway device 1-10 in 100,000 paper cites a study which argues that the risk of morbidity related to using an inferior device (i.e. single-use LMA) would be much higher than this and therefore doesn't warrant change to disposables • C - False - in pounds cLMA = 90 pounds 1-3 pounds to sterilize (x40), single use 3.50-7.00 • D - False - PVC absorb more N2O than cLMA • E - True - Can be used up to 40 times - possibly more if no signs of wear |
|
|
When providing anaesthesia for a patient who is a
Jehovah's Witness, it is NOT acceptable to use A. erythropoietin B. albumin and clotting factors C. cardio-pulmonary bypass D. isovolaemic haemodilution E. blood products for children, if parents insist that they be withheld |

B
Between B and D. Don’t have a good reason for picking B over D • A – False • B – Albumin and clotting factor may be acceptable to some • C – False • D – According to CEACCP article, isovolaemic haemodilution may not be acceptable to some (whilst hypervolaemic haemodilution is acceptable) • E – According to CEACCP article 2004 - Anaesthesia and Jehovah's witness "Children under 16 yrs of age of Jehovah’s Witness parents present a difficult legal management problem. For elective procedures, there should be full and frank discussion between the surgeon, anaesthetist, parents and child (if they are old enough to understand). Most parents will accept that while every attempt will be made to avoid blood, a doctor will not allow a child to die for lack of transfusion. Children under 16 can legally give consent themselves if they can understand the issues involved (Gillick Competence). However, the courts have proved willing to overrule the refusal of specific procedures by children. "If consent for transfusion is refused, and it is felt unreasonable to proceed with surgery without the freedom to transfuse, an application to the High Court for a ‘specific issue order’ can be made; this allows transfusion to go ahead without removing all parental authority. Medical social workers can provide assistance in obtaining this action. Where time does not permit application to the courts, blood should be given. Failure to give life-saving treatment to a child could render the doctor vulnerable to criminal prosecution." |
|
|
A diagnosis of pulmonary embolism is most strongly
suggested by A. intraluminal filling defects or vascular cutoffs on angiography B. Pa02 less than 85 mmHg and an abnormal lung perfusion scan C. Pa02 less than 85 mmHg and an elevated PaCO2 D. right ventricular hypertrophy with right ventricular strain and right axis deviation on electrocardiography E. "unmatched" ventilation-perfusion defects |
A
|
|
|
A 40-year-old man with Marfan's syndrome has undergone
successful thoracoabdominal aortic reconstruction for aortic dissection. He has a CSF (cerebrospinal fluid) drain in situ. 48 hours post-operatively the CSF is noted to be bloodstained and he becomes obtunded. The most appropriate urgent investigation is A. CSF microscopy and culture B. MRI (magnetic resonance imaging) brain C. MRI spine D. non-contrast head CAT scan E. serum electrolytes |
D
This history seems very similar to a case report for 2005 which concludes: Journal of Cardiothoracic and Vascular Anesthesia, Vol 19, No 3 (June), 2005: pp 392-399 "The appearance of new blood-tinged CSF appears to be an indication to obtain a computed tomography scan to rule out any potentially correctable intracranial pathology" |
|
|
Blood donors most commonly implicated in TRALI
(Tranfusion Related Acute Lung Injury) are A. diabetics B. donors previously resident in the United Kingdom C. indigenous Australians D. men under 50 years of age E. multiparous females |
E
http://www.medscape.com/viewarticle/583195_5 “In about half the cases studied, the HLA antibodies in the implicated donor correspond with one or more of the HLA antigens in the recipient. In other cases, neutrophil-specific antibodies (HNA1, HNA-3a) have been identified in the plasma of implicated units. These antibodies are most commonly found in the donations of multiparous women.” |
|
|
You are called to the cardiac catheter lab to assist when a
55-year-old man with unstable angina becomes restless during difficult placement of a right coronary artery stent. When you arrive he is conscious and responding to voice. He is sweating with a pulse of 60 beats per minute in sinus rhythm, blood pressure measured from arterial catheter of 80/50 mmHg and Sp02 of 97%. The arterial pressure wave has an exaggerated fall with inspiration. The most appropriate next clinical intervention would be to A. administer atropine B. commence an adrenalin infusion C. perform a quick transthoracic echocardiograph D. sedate and intubate E. transfer to operating theatre immediately |
C
A. False – Whilst a HR closer to 80 might be better, It would be difficult to titrate to this with atropine. Excessive tachycardia would also be bad in the setting of IHD and would decrease LV filling more in the setting of tamponade B. False - this is unlikely to hurt, but he has adequate cerebral perfusion, perhaps some fluid loading would be in order first C. True - if it was quick, it may reveal tamponade and even facilate percutaneous drainage. This appears to be the best option D. False - this seems a bit premature, given we are clearly told that airway and breathing are adequate E. False - not a bad option to start organising, other things should be done first |
|
|
A 16-year-old arrives in your Emergency Department
having fallen from, and been trampled by, a horse. The ambulance officers report that his initial GCS (Glasgow Coma Scale) was 15 and is now 11. His pulse is 120 and blood pressure 80/60 mmHg. Sp02 is 97% when breathing on a Hudson mask. On auscultation his chest is clear. He has facial bruising and a tender abdomen. Your first priority now is to A. administer an IV (intravenous) fluid bolus B. arrange an urgent CT scan of the head C. administer mannitol D. perform a FAST (focussed assessment with sonography for trauma) examination E. secure the airway by intubation |
A
Given that airway and breathing are okay for now, he needs C sorted Whilst you probably don’t want the BP too much higher with an undifferentiated bleeding source, some IV fluid still seems appropriate A FAST scan would seem the next best thing to do |
|
|
An otherwise healthy 4-year-old presenting for
adenotonsillectomy develops a cough and laryngospasm during gaseous induction. At intubation clear secretions are visible at the glottis and after intubation transient wheezing is noticed. Clear fluid is aspirated from the endotracheal tube. At the end of the case, the child has a Sp02 of 96% with an Fi02 of 0.3. Airway pressures are normal. The most appropriate further management of this suspected aspiration episode is to A. administer broad spectrum antibiotics and otherwise manage routinely B. administer steroids and extubate after 1 hour if chest is clear on auscultation C. extubate and observe in recovery for 4-6 hours D. measure pH of tracheal aspirate and base further management on findings E. perform on-table chest X-ray and base further management on findings |
C
Lots of discussion on wiki about this one Antibiotics and steroids do not change outcome with aspiration Whilst D and E would be reasonable things to do to demonstrate aspiration, a positive or negative result would not change my management, which would be to extubate given they are proving their ability to adequately oxygenate |
|
|
Insertion of a pulmonary artery catheter is relatively
contraindicated if the patient has an ECG (electrocardiogram) showing A. anterior fascicular block B. atrial fibrillation C. left bundle branch block D. posterior fascicular block E. right bundle branch block |
C
American college of cardiology: Conditions in which a relative contraindication to RHC exists 1. Coagulopathy (or anticoagulant therapy that cannot be temporarily discontinued). 2. Recent implantation of permanent pacemaker or cardioverter-defibrillator (in which case placement under fluoroscopic guidance is recommended). 3. Left bundle branch block (see “Acquisition and Interpreta- tion of Data”). 4. Bioprosthetic tricuspid (or pulmonic) valve. Conditions in which an absolute contraindication to RHC exists 1. Right-sided endocarditis. 2. Mechanical tricuspid (or pulmonic) valve prosthesis. 3. Presence of thrombus or tumor in right heart chamber. 4. Terminal illness for which aggressive management is considered futile. |
|
|
The characteristics of a high spinal block do NOT include
A. dyspnoea B. hypotension C. inability to make a fist D. loss of phonation E. tachycardia |
E
Sympathectomy leads to bradycardia |
|
|
Regarding thoracic anatomy, the
A. aorta passes through the diaphragm posteriorly at T10 B. carina most commonly lies at T4 in the adult C. lungs comprise 16 bronchopulmonary segments in total D. oblique fissure runs along the 6th rib on both sides E. right main bronchus runs 45° to the vertical |
B
A. false - Levels at which structures pass through diaphragm : T8 IVC, phrenic n T10 oesophagous, vagi, L gastric a. and v. T12 aorta, thoracic duct, azygous vein B. true - T4/T5 C. false - 19 or 20 depending on if you count left medial basal segment D. false -'Right oblique fissure leaves verterbral column posteriorly at level of 5th rib. ...... left oblique fissure has more variable origin anywhere from 3rd to 5th rib.' (Ellis) E. false - 'the right main bronchus is shorter, wider and more vertical than the left (25deg). After 2.5cm it gives off the R upper bronchus. The left main bronchus is more angled 45deg and is 5cm long' |
|
|
Recommendations for the initial management of post dural puncture headache include
A. ensuring adequate analgesia B. intravenous caffeine infusion C. oral sumatriptan D. prolonged bed rest E. prophylactic blood patching |
A
A. True – best answer B. False – Although caffeine is often prescribed to prevent or treat PDPH, evidence for its efficacy is limited and conflicting C. False – There was no evidence to support the efficacy of sumatriptan in PDPH, although in open-label studies other triptans have been reported to have sufficient benefit to warrant further evaluation D. False – There was no evidence of benefit with bed rest in the treatment or prevention of PDPH E. False – there is conflicting evidence of benefit of prophylactic EBP administration |
|
|
Presenting features of carcinoid syndrome include
A. hypoglycaemia B. mitral regurgitation C. renal failure D. splenomegaly E. supraventricular tachycardia |
E
Can get mitral regurg and hypoglycaemia (according to OHA and Stoelting) but SVT is more common |
|
|
Findings in a patient with serotonin syndrome include each
of the following EXCEPT A. clonus B. diaphoresis C. hyperreflexia D. miosis E. tachycardia |
D
Mydriasis not miosis |
|
|
The glomerular filtration rate of a paediatric patient (in
ml.min-l.m-2) is similar to that of an adult by the age of approximately A. 1 month B. 6 months C. 2 years D. 4 years E. 6 years |
C
GFR reaches adult values by 2 years – OHA p 760 |
|
|
The QT interval may be prolonged by each of the following
EXCEPT A. high intrathoracic pressure B. hypothermia C. magnesium sulphate D. suxamethonium E. volatile anaesthetic agents |
C
Mg does not prolong QT syndrome and is the first line treatment for torsades. |
|
|
The Pringle manoeuvre (a surgical intervention when faced
with exanguinating haemorrhage from the liver) involves clamping the A. aorta above the coeliac axis B. hepatic artery only C. hepatic vein only D. portal pedicle E. splenic artery only |
D
BJA 2004. 93 (2): 204. Effects of Pringle manoeuvre and ischaemic preconditioning on haemodynamic stability in patients undergoing elective hepatectomy: a randomized trial “During hepatic resection, the risk of severe intraoperative bleeding represents a major risk. To avoid massive blood loss, continuous or intermittent vascular clamping of the hepatic artery and portal vein (‘Pringle manoeuvre’) is an efficient method to reduce haemorrhage.” Portal pedicle contains Hep Artery and Portal vein therefore D is correct. Also referred to as portal triad, which is Hep a., Portal v. and bile duct. |
|
|
When using NSAIDs (non-steroidal anti-inflammatory
drugs) and COX-2 (cyclo-oxygenase 2) inhibitors for postoperative analgesia, A. COX-2 inhibitors are more effective analgesics than NSAIDs B. COX-2 inhibitors have less effect on renal function than NSAIDs C. COX-2 inhibitors impair platelet function D. COX-2 inhibitors trigger aspirin induced respiratory disease with a similar likelihood to NSAIDs E. NSAIDs increase the risk of peri-operative bleeding after some types of surgery |
E
• A - False. Coxibs are as effective as NSAIDs in the management of postoperative pain...NNT's comparable with those for conventional NSAIDs for the treatment of mod-severe acute pain (APMSE 2010 Section 4.2.3) • B - False. "Renal and cardiovascular effects of COX-2 inhibitors are similar to conventional NSAIDs." Stoelting, 4th. ed., p.281. • C - False. "These drugs (COX-2 inhibitors) lack effects on platelets at therapeutic doses and may be associated with decreased gastrointestinal side effects in patients with arthritis, compared with nonspecific NSAIDs." and "COX-2 inhibitors have no effect on platelet aggregation, bleeding time or postoperative blood loss." Stoelting, 4th. ed., p.277 & 281. • D - False. Investigation of patients with AERD (aspirin exacerbated respiratory disease) has provided encouraging evidence that coxibs, administered at analgesic doses, do not produce bronchospasm in these patients (APMSE 2010) • E - True. "Preoperative NSAID therapy significantly increases intraoperative and postoperative blood loss in children undergoing tonsillectomy." Stoelting, 4th. ed., p.281. |
|
|
The intraoperative hypothermia for aneurysm surgery trial
(IHAST) showed that cooling to a target temperature of 33°C A. did NOT improve neurological outcome in WFNS (World Federation of Neurosurgical Surgeons) grade I¬-III patients B. did NOT improve neurological outcome in WFNS grade IV-V patients C. improved neurological outcome in WFNS grade I-III patients D. improved neurological outcome in WFNS grade III patients E. improved neurological outcome in WFNS grade IV-V patients |
A
IHAST Trial NEJM 2005: BACKGROUND: Surgery for intracranial aneurysm often results in postoperative neurologic deficits. We conducted a randomized trial at 30 centers to determine whether intraoperative cooling during open craniotomy would improve the outcome among patients with acute aneurysmal subarachnoid hemorrhage. METHODS: A total of 1001 patients with a preoperative World Federation of Neurological Surgeons score of I, II, or III ("good-grade patients"), who had had a subarachnoid hemorrhage no more than 14 days before planned surgical aneurysm clipping, were randomly assigned to intraoperative hypothermia (target temperature, 33 degrees C, with the use of surface cooling techniques) or normothermia (target temperature, 36.5 degrees C). Patients were followed closely postoperatively and examined approximately 90 days after surgery, at which time a Glasgow Outcome Score was assigned. RESULTS: There were no significant differences between the group assigned to intraoperative hypothermia and the group assigned to normothermia in the duration of stay in the intensive care unit, the total length of hospitalization, the rates of death at follow-up (6 percent in both groups), or the destination at discharge (home or another hospital, among surviving patients). At the final follow-up, 329 of 499 patients in the hypothermia group had a Glasgow Outcome Score of 1 (good outcome), as compared with 314 of 501 patients in the normothermia group (66 percent vs. 63 percent; odds ratio, 1.14; 95 percent confidence interval, 0.88 to 1.48; P=0.32). Postoperative bacteremia was more common in the hypothermia group than in the normothermia group (5 percent vs. 3 percent, P=0.05). CONCLUSIONS: Intraoperative hypothermia did not improve the neurologic outcome after craniotomy among good-grade patients with aneurysmal subarachnoid hemorrhage. |
|
|
A 25-year-old male presents for ECT (electroconvulsive
shock therapy) at a free-standing facility. He has a life¬threatening depressive illness that has not responded adequately to medication, however he is still taking tranylcypramine (Parnate). You should A. cancel the procedure, cease the tranylcypramine and perform the ECT in 2 weeks B. proceed with the ECT, but induce with midazolam and remifentanil C. proceed with the ECT, but pre-treat with esmolol D. proceed with the ECT with caution, but with your usual drugs E. transfer the patient to a tertiary centre for their ECT |
D
Tranylcypramine (a MAOI) The concern is that there will be an exaggerated response to sympathetic stimulation with a MAOI. With ECT there is a vagal response, followed by an overwhelming sympathetic surge, which could cause a hypertensive crisis. A – Morgan and Mikhail Ch 27 – "The practice of discontinuing MAO inhibitors at least 2 weeks prior to elective surgery is no longer recommended. With the exception of tranylcypromine, these agents produce irreversible enzyme inhibition; the 2-week delay allows sufficient regeneration of new enzyme. Studies suggest that patients may be safely anesthetized, at least for ECT, without this waiting period” B – Midazolam may supress seizures C – Esmolol pre-treatment could lead to an exagerrated initial vagal response D – This seems sensible E – Unnecessary |
|
|
Cryoprecipitate contains each of the following clotting
factors EXCEPT A. factor VIII B. factor IX C. factor XIII D. fibrinogen E. von Willebrand factor |
B
Contains high levels of FVIII, fibrinogen, Factor XIII, VWF and fibronectin. |
|
|
A patient with bipolar disorder presents for elective
laparoscopic cholecystectomy. She takes lithium and has therapeutic blood levels. The lithium A. may increase her requirement for volatile anaesthetic agents B. may prolong the duration of depolarising muscle relaxants C. may prolong the duration of non-depolarising muscle relaxants D. may prolong the duration of both depolarising and non-depolarising muscle relaxants E. should be ceased 2 weeks pre-operatively |
D
Lithium potentiates both depolarising and non-depolarising muscle relaxants – Stoelting |
|
|
When a new diagnostic test is evaluated in a population of
subjects in whom the diagnosis is known, the following results are obtained Disease known Disease known to be present to be absent New test result positive 80 40 New test result negative 20 180 In this population the NEGATIVE predictive value of this test is closest to A. 10% B. 33% C. 67% D. 80% E. 90% |
E
TN/ TN+FN = 180/180+20 = 90% |
|
|
Immediately following delivery by caesarean section under
regional anaesthesia a previously healthy primigravida complains of chest pain and breathlessness, and then becomes unconscious. The most likely diagnosis is A. accidental administration of suxamethonium B. air embolism C. amniotic fluid embolism D. anaphylaxis to syntocinon E. pulmonary thromboembolism |
C
Timing and presentation make AFE seem likely |
|
|
The most important aspect of the pen-operative
management of a patient with Gilbert's Syndrome is A. avoidance of fasting B. avoidance of stress C. pre-operative transfusion of fresh frozen plasma (FFP) D. prophylaxis against hepato-renal syndrome E. recognition of the aetiology of the laboratory abnormality |
E
Gilbert’s = Asymptomatic familial unconjugated non-haemolytic hyperbilirubinaemia, perioperative jaundice may be precipitated by stress/surgery/starvation. (OHA p297) |
|
|
A 12-year-old boy with spastic cerebral palsy and painful
muscle spasms presents for multilevel osteotomies of his legs. The most effective option for post-operative analgesia would be A. a combination of NSAIDS (non-steroidal anti¬inflammatory drugs) and regular tramadol B. continuous lumbar epidural analgesia with a mixture of local anaesthetic and clonidine C. regular paracetamol and oxycodone D. patient controlled morphine E. spinal morphine |
B
CEACCP 2010 - Cerebral palsy and anaesthesia. Caudal or epidural analgesic techniques combining extradural clonidine with a local anaesthetic agent are proving to be beneficial in combating pain associated with both the operative procedure and muscle spasms. In the authors’ experience, extradural clonidine is more effective in the management of postoperative muscle spasms than a combination of either extradural or systemic opioids administered in conjunction with enteral or parentral benzodiazepines, and it produces less sedation. |
|
|
A 25-year-old man with Marfan's syndrome is scheduled for
aortic arch reconstruction under circulatory arrest. Cooling to 18 degrees is planned. The maximum time for circulatory arrest at this temperature after which the risk of long term neurological injury increases markedly is A. 15 minutes B. 25 minutes C. 35 minutes D. 45 minutes E. 55 minutes |
C
40 Min seems safe Straight Deep Hypothermic Arrest: Experience in 394 Patients Supports Its Effectiveness as a Sole Means of Brain Preservation – Ann Thorac Surg 2007;84:759 – 67 • Based upon these findings and accumulated experience, it appears that the great majority of patients can support unharmed a circulatory arrest of 30 minutes at 18°C, provided that electrocerebral silence has been obtained. • No deficit or only a transient neurologic dysfunction is expected when the ischemic period extends to 40 minutes, provided that rewarming is correctly performed and hemodynamic stability maintained postoperatively. • With an arrest time superior to 40 minutes, neurologic deficit is prone to occur particularly in high-risk patients, such as older patients and those presenting with diabetes or hypertension. |
|
|
Ebstein's abnormality describes a congenital defect of the
A. aortic valve B. mitral valve C. pulmonary valve D. pulmonary veins E. tricuspid valve |
E
Ebstein anomaly is a congenital malformation of the heart that is characterized by apical displacement of the septal and posterior tricuspid valve leaflets, leading to atrialization of the right ventricle with a variable degree of malformation and displacement of the anterior leaflet. Features: 1.Congenital downward displacement of deformed tricuspid valve 2.Atrialisation of RV 3.Maybe no obvious signs 4.Risk of SVT during induction 5.Often also have an ASD |
|
|
A 32-year-old patient is admitted with early acute liver
failure (unrelated to paracetamol ingestion). Management should include A. avoidance of intubation to monitor encephalopathic progress B. consideration for liver transplantation if the INR (international normalised ratio) is over 3 C. limited use of sodium containing fluids during acute resuscitation D. N-acetyl-cysteine as a general hepatoprotective agent E. prophylactic antibiotics |
Which is better out of D and E?
• A – False, Grade III & IV encephalopathy may need intubation • B – King’s College Criteria for liver transplantation includes INR>3.5 as a one criteria for non paracetamol aetiology liver failure. (>6.5 is paracetamol aetiology) • C - As opposed to chronic liver disease, most patients presenting with ALF are not sodium overloaded, hence sodium restriction is not indicated • D - Intensive care management of acute liver failure Current Opinion in Critical Care 2008, 14:179–188: “Previous investigations from this institution and results from a recent multicentre randomized controlled trial of the Adult US Acute Liver Failure Study Group (ALFSG) suggest benefit of NAC also for the treatment of nonacetaminophen etiologies” • E – Same reference as D – “Prophylactic treatment with intravenous antibiotics and antifungal agents is commonly performed. This approach has been shown to significantly reduce the risk of sepsis, decrease the risk of progression to high-grade encephalopathy and increase the potential for successful transplantation; however, survival was not affected” |
|
|
Drugs that may be used for the management of heart
failure, secondary to dilated cardiomyopathy in pregnancy, include each of the following EXCEPT A. ACE (angiotensin-converting enzyme) inhibitors B. beta-blockers C. digoxin D. loop diuretics E. nitrates |
A
Class D drug. BJA 93 (3): 428–39 (2004) Recognition and management of maternal cardiac disease in pregnancy "The use of angiotensin-converting enzyme inhibitors during pregnancy is contraindicated because of the risk of teratogenicity, neonatal anuric renal failure and neonatal death." |
|
|
Which statement regarding the use of opiates for the
management of acute pain is true? A. in adults patient weight is the best predictor of opioid requirements B. metabolism to codeine-6-glucuronide produces the analgesic effect of codeine C. morphine produces more nausea and vomiting than pethidine D. pethidine is superior to morphine in the management of renal colic pain E. tramadol has a lower risk of respiratory depression than other opioids at equianalgesic doses |
E
A. False – age is the better determinant: 100-age = 24 hr morphine dose (p63 APM 2010) B. False – 10% demethylation in liver to morphine, remainder demethylated to inactive norcodeine (Stoelting) C. False – “pethidine induced more nausea and vomiting than morphine when used parenterally in the ED (level III-3) and in first 2 hours after gynaecological surgery (level II, APM 2010) D. False – not proven (level II, APM 2010) E. True – “and it does not depress the hypoxic ventilatory response” (level II APM 2010) |
|
|
A 38-year-old primigravida presents with progressive
dyspnoea in late pregnancy. The strongest indicator for further investigation would be A. a 2/6 systolic ejection murmur B. a raised JVP (jugular venous pressure) C. a third heart sound D. orthopnoea E. peripheral oedema |
B
Stoelting's Anesthesia and Coexisting Disease “The presence of congestive heart failure is suggested by hepatomegaly and jugular venous distention, as these changes do not accompany normal pregnancy” Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition “Any cause of a significant increase in the volume load on the ventricle(s) can cause an S3. Examples include valvular regurgitation, high-output states (anemia, pregnancy, arteriovenous fistula, or thyrotoxicosis), left-to-right intracardiac shunts, complete A-V block, renal failure, and volume overload from excessive fluids or blood transfusion” |
|
|
With regard to peri-operative cardiac risk reduction there is
evidence that all of the following reduce perioperative cardiac morbidity EXCEPT A. intra-operative use of nitrous oxide B. peri-operative use of alpha-two agonists C. perioperative use of diltiazem D. peri-operative use of statins E. tight peri-operative glycaemic control (blood sugar between 3.5 and 6mmo1.1-1) |
A
Questions likely to be from this article - Evidence-based perioperative risk reduction. CAN J ANESTH 2005 / 52: 6 / pp R1–R11 • A – “ Two independently conducted trials have shown nitrous oxide to increase the incidence of perioperative and postoperative myocardial ischemia. Furthermore, nitrous oxide increases homocysteine levels for over 72 hr postoperatively. This may influence both platelet reactivity and endothelial function. Nitrous oxide has the added distinction of doubling the incidence of postoperative nausea and vomiting. Moreover, nitrous oxide is a poor anesthetic agent. There is no reason to use nitrous oxide in patients at high risk for postoperative cardiac complications.” • B – True “In a subsequent meta-analysis alpha 2 agonists were found to reduce the incidence of postoperative ischemia and MI” • C – True – Cardioprotective effects of diltiazem infusion in the perioperative period European Journal of Cardiothoracics Volume 12, Issue 3, Pages 420-427 (September 1997): “The analysis found that calcium channel blockers reduced the incidence of ischemia; postoperative supraventricular tachycardia. Conclusion: The present study demonstrates that diltiazem infusion provides superior anti-ischemic protection and control of supraventricular arrhythmias as compared to nitroglycerin and does not produce any negative inotropic effect, as demonstrated by transesophageal echocardiography.” • D – True Statins Are Associated With a Reduced Incidence of Perioperative Mortality After Coronary Artery Bypass Graft Surgery. Circulation. 2004;110: “The risk of perioperative death was reduced by 30% in patients who had a statin started within two days of surgery. Conclusions: Preoperative statin therapy may reduce the risk of early mortality after primary CABG surgery with CPB.” • E – True – Perioperative glycemic control and the risk of infectious complications in a cohort of adults with diabetes. Diabetes Care September 1999 vol. 22 no. 9 1408-1414 “CONCLUSIONS: In patients with diabetes who undergo coronary artery surgery, postoperative hyperglycemia is an independent predictor of short-term infectious complications. Physicians should consider a glucose concentration target of < or =200 mg/dl to reduce the risk of infection.” |
|
|
Duchenne Muscular Dystrophy is a contra-indication to the
use of A. corticosteroids B. non-depolarising neuromuscular blockers C. suxamethonium D. tramadol E. volatile anaesthetic agents |
C
CEACCP, Apr 2003; 3: 50 - 53. Paediatric anaesthetic pharmacology Cardiac arrest has been reported in several patients, some of whom some were found to have a previously undiag- nosed muscular dystrophy. Children with muscular dystrophy develop severe hyperkalaemia in response to succinylcholine. |

