![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
33 Cards in this Set
- Front
- Back
|
what are the generic and expected processes which occur in the body that are associated with old age |
Decreasingamountoftissue Alteredmoleculardispositionofthematrix Accumulation of degraded molecules Reducedefficiencyoffunctionaltissueelements Reducedsyntheticcapacityofdifferentiatedcells Alteredlevelsoftrophichormones,growthfactorsand cytokines, or altered ability of cells to respond Alterationsintheloadingpatternsoftissuesorthe tissues response to loading |
|
|
how does age affect bone |
reduced bone tissue, relative decline in trophic factors favouring osteoclastic over osteoblastic activity, diminished differentiation potential of bone marrow stem cells |
|
|
how does age affect chondroid tissues |
reduced ability to form large hydrophilic complexes leading to decreased swelling pressure, predisposing to OA and IVD degeneration |
|
|
how does age affect ligaments |
altered collagen synthesis leading to reduced elasticity |
|
|
how does age affect the skeletal system |
loss of muscle mass and decreased power due to loss of fibre number and fibre atrophy how |
|
|
how does age affect joints |
Osteoarthritis Rheumatoid arthritis |
|
|
is osteoarthritis thought to be caused by its own factors or as a result of other disorders |
it is the clinical and pathological outcome of a range of disorders |
|
|
what is OA characterised by |
Characterised by loss of, and change in, the composition of cartilage proteoglycans leading to failure of normal responses to stress |
|
|
what are the risk factors for OA |
Risk factors include gender, race/ethnicity, bone density, postmenopausal loss of estrogen, nutritional factors, and heredity |
|
|
what are the symptoms of OA |
Pain – worse on weightbearing and improves with rest - constant (rest) pain with advanced disease Stiffness – Frequently present after a period of inactivity Swelling – exclude other pathology |
|
|
what is the difference between crystal arthropathy and normal arthiritis |
it is acute and very painful? |
|
|
what is also associated with crystal arthropathy that is not in normal arthritis |
Gout – urate crystals Pseudogout – calcium pyrophosphate dihydrate crystals |
|
|
what is gout |
* negatively birefringent refers to its appearance under polarised light |
|
|
where does gout clinically affect the most |
1st MTP of foot |
|
|
what is Calcium Pyrophosphate Crystal Deposition also known as |
pseudogout |
|
|
what is Rheumatoid Arthritis |
Autoimmune disease resulting in a systemic inflammatory disorder that principally attacks synovial joints |
|
|
name 3 metabollic bone dieseases |
Osteoporosis |
|
|
the Diminution of bone mass and quality is associated with what in OA? |
increased risk of fractures |
|
|
what causes osteoporosis |
Imbalance between bone formation (osteoblasts) and bone resorption (osteoclasts) |
|
|
in bone densitometry what is the normal score |
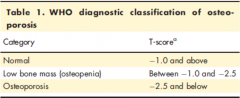
T=0 is normal in young woman |
|
|
what T score does Osteoperosis get |
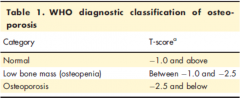
T=-2.5 |
|
|
what is the best way to measure bone density |
Gold standard assessment is by dual energy X-ray absorptiometry (DXA) |
|
|
are there any clinical manifestations of Osteoporosis before there is a fracture |
Osteoporosis has no clinical manifestations until there is a fracture |
|
|
explain fully the treatment options for osteoporosis |
Prevention is better than cure – lifestyle choices and risk factor modification (smoking, alcohol, sedentary) Vitamin D supplementation Drug therapy: Bisphosphonates (Alendronate / Risedronate / Zoledronate) and RANKL inhibitors (Denosumab) – inhibit osteoclast activity Parathyroid hormone analogues (Teriparatide) – truly osteoanabolic |
|
|
what is osteomalacia |
softening of bones - normally due to Vitamin D or calcium deficiency |
|
|
what may develop as a result of osteomalacia |
Proximal myopathy and symptomatic hypocalcaemia may develop |
|
|
what are the results of osteomalacia |
Reduced plasma calcium Raised PTH and ALP |
|
|
how would you treat someone with osteomalacia |
High dose Vit D loading followed by life long supplementation |
|
|
what is Paget's disease of bone |
Chronic condition of bone most often diagnosed in sixth decade of life |
|
|
what happens in Paget's disease of bone |
Increased bone resorption by abnormal osteoclasts leading to increased osteoblastic activity Rapid bone turnover with deposition of woven bone – structurally weak and prone to fracture and deformity Can affect single or multiple sites |
|
|
what is sarcopenia |
A syndrome characterised by progressive and generalised loss of skeletal muscle mass and strength associated with ageing, with a risk of adverse outcomes such as physical disability, poor quality of life and death |
|
|
what are the 4 different types of sarcopenia and what are their causes |
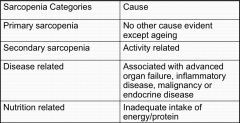
|
|
|
what 2 types of decline occur in sarcopenia |
Quantitative decline (muscle mass – DXA or bioimpedance analysis) Qualitative decline (muscle strength and function – isometric handgrip) |

