![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
21 Cards in this Set
- Front
- Back
|
Systemic circulation vs pulm circ
how does pulmonary and bronchial vessels compare? in terms of bp, % of CO, and resistance |
pulm: 15/5, 100% CO, low vascular resistance bronchial: 100/0, <1% of CO, high vasc resistance |
|
|
the large surface area of pulm blood going into lung is described as
this is also doing what job? |
sheet flow
providing nutrient supplies to lung parenchyma and respiratory bronchioles |
|
|
the top of the lung doesn't get as much pulm blood flow as base. Why? use equations |
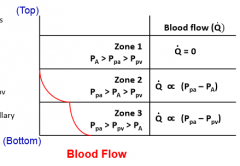
gravity on blood pulls down transmural pressure (low at apex, high at base), so Pa (pressure alveoli here) is what's changing in the different regions relative to the Ppa and Ppv |
|
|
exhale passively. how |
the lungs recoil. they get stretched out and want to return to normal on their own. don't need to do work for that. |
|
|
how do lungs respond to hypoxia?
how does this happen? |
if only part of the lung is hypoxic, then constriction to the hypoxic areas, so that the blood will go to the alveoli with higher chance of ventilation
if whole lung hypoxic: constrict everything, can eliminate zone 1 (htn, so what was zone 1 -> zone 2 type) and improve diffusion capacity via pulm htn.
direct effect of hypoxia is inhibiting voltage-gated K channel, so get resulting membrane depolarization to increase [Ca] of vascular smooth muscles -> vasoconstrict |
|
|
so what all factors affect pulm vasc resistance? |
neurohumoral
neural: ***symp by alpha aderenoceptors like NE for vasoconstriction. General parasym causes vasodilation
humoral: endogenoous: histamine, thromboxanes, prostaglandin E2 and F2alpha for constricting. Prostacyclinc PGI2, NO cause vasodilation |
|
|
how does pulm vasc resistance change with lung volume? |
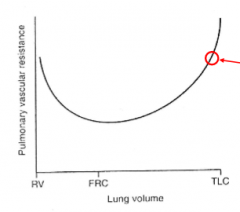
it's lowest at FRC
at TLC alveoli so inflated, compress alveolar vessels (right next to them)
at RV, lung is at minimum volume, so extra-alveolar vessels compressed |
|
|
how do the lungs adjust for increased or decreased cardiac output?
how is that accomplished? two ways |

increased CO, reduce pulm vasc resistance. Decreased CO, increase pulm vasc resistance.
in htn: recruit more vessels that aren't normally used. distension is opening vessels for less resistance. |
|
|
metabolic functions of the lungs- why is have the lungs do these a good approach?
notable metabolic functions lungs serve: 5 |
all the blood has to go through there eventually
prostaglandins E F almost completely removed leukotrienes almost completely removed serotonin 90% removed bradykinin 80% inactivate Angiotensin I 70% converted to Ang II |
|
|
in asthmatic pt laboring to exhale, how does Zone 1 area compare to normal pt? |
zone 1 area will be bigger since alveolar pressure will be higher everywhere as trying to generate air flow
zone 2 Ppa> Palv > Ppv becomes zone 1 Palv > Ppa > Ppv |
|
|
what is the law about gas diffusion across a biological membrane?
what does it depend on? what is the equation like? |
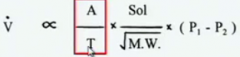
Fick's Law of diffusion
physical properties of membrane A/T, physiochemical properties of the gas Sol/vMW, pressure gradient across the membrane p-p
a area, t thickness, solubility |
|
|
so for Fick's Law. which parts is actually about the lung? |
total surface area = 70 m^2 thickness: .15-5 microns with surface lining, alveolar epithelium, BM, capillary endothelium
these change in dz states |
|
|
how does CO2 compare to O2 in solubility
MW?
how do their partial pressures compare in venous and alveolar gas |
CO2 is 20x more soluble
molecular weight is only slightly higher than CO2
O2 40 vs 100 CO2 46 vs 40 |
|
|
so keeping the factors of the lungs and the gases in mind: how would you describe the diffusion of O2 from air to blood in lungs?
during exercise?
if lung dz? |
in normal, "change of oxygen tension" is maximized/completed in .25s even though it has .75s in the lung
this is good because during exercise and hyperventilation, the oxygen still reaches equilibrium even though air and blood stays less time
might only reach equilibrium after the full .75s. If grossly abnormal, might never reach balance, so reduced diffusion capacity (membrane thicker or less surface area) |
|
|
so dz could be what changes? as per Fick's law |
airways smaller in surface area
walls thicker |
|
|
How to describe CO2 gas exchange? |
again only .25s to reach the CO2 equilibrium
CO2 has good diffusion capacity even though the pressure difference (46-40 vs 100-40 for ox) isn't very large because it's so soluble. |
|
|
when testing pt's diffusion capacity, what do they use? why? |
carbon monoxide
takes the same path as oxygen across membrane, has high affinity for hemoglobin, easy to measure since Pco is normally zero in the blood |
|
|
diffusion capacity equation
typical value for CO relative value for O2
what are the factors that will affect diffusion capacity? |
D_L_ = V`/(P1-P2) for healthy lungs CO is 25 ml/min/mmHg. (DL is diffusion capacity of lung; V` is diffusion rate since a constant; also this is Ohm's equation)
DL of O2 = 1.23 x DL CO = 31
membrane and hemoglobin |
|
|
why is hemoglobin such a huge component of diffusion capacity?
equation that includes hemoglobin factor uses what variables |
when O2 attached to Hb that O2 doesn't participate in the Po2 allowing more O2 to be diffusing into blood.
rate of rxn of O2 with hb blood volume |
|
|
what abnormal conditions decrease diffusing capacity and why |
thickening of barrier: interstitial edema, interstitial fibrosis (from sarcoidosis or scleroderma)
decreased surface area: emphysema, tumor, low pulm blood volume
decreased RBC uptake: anemia, low pulm blood volume
ventilation-perfusion mismatch |
|
|
describe N2O and CO diffusion capacity |
N2O: perfusion limited- how much blood is going through, it's going to equilibrium very fast
CO: diffusion limited. It's not going to saturate the blood, so it's diffusing the entire time |

