![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
36 Cards in this Set
- Front
- Back
|
what are the 5 key biological roles of Calcium |
1) muscle contraction 2) nerve excitation 3) blood coagulation 4) intracellular messenger 5) enzymes of intermediary metabolism |
|
|
what are the % figures for Serum Calcium |
FREE --> 47% BOUND to albumin --> 47% COMPLEXED --> 6% |
|
|
which portion of the serum calcium ( free bound or complexed) regulates the feedback mechanisms of the body and is physiologically important |
the FREE fraction (47%) |
|
|
why is total calcium as well as free calcium measures when measuring calcium levels |
if a patient has a low albumin conc. then total Ca will also be low, but FREE Ca will be quite normal |
|
|
what is conc of calcium above which would be regarded as hypercalcaemia |
>2.6mmol/l |
|
|
what is conc of calcium below which would be regarded as hypocalcaemia |
<2.2mmol/l |
|
|
what organs are involved in Ca homeostasis |
-kidney -gut -bone -parathyroid glands --Ca sensing receptors
|
|
|
what are the 2 main hormones of metabolic control of Ca |
parathyroid hormone 1,25 - dihydroxycholecalciferol |
|
|
where does Ca absorption mainly take place |
-small intestine --> duodenum + jejunem
|
|
|
what are the 2 pathways for Ca absorption |
1) cell-mediated active transport (controlled by 1,25 DHCC) 2) passive diffusion (depends on lumenal Ca conc) and unaffected by 1,25 DHCC |
|
|
under what circumstances will 1,25 DHCC increase fractional absorption of Ca |
-pregnancy -lactation -dietary intake falls - GROWTH |
|
|
what part of the kidney transport Ca to where |
65% reasborbed in PROXIMAL convoluted tubule
20% in cortical thick ascending loop of henle 15% in distal convoluted tubule (both these increased by effect of PTH) |
|
|
what regulates the secretion of parathyroid hormone by the parathyroid glands |
FREE Calcium which is sensed by calcium sensing receptors |
|
|
as Ca levels rise what happens to PTH levels |
they fall its an inverse relationship dudeo |
|
|
what type of cells are calcium sensing receptors and what is their mode of action |
they are chief cells their MOA is G-protein coupled receptors |
|
|
what happens When calcium sensing receptors sense high calcium levels in the renal tubules |
It decreases the reabsorption of calcium and increases its excretory rate |
|
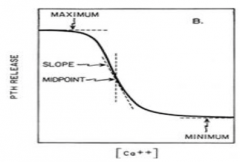
this is the steep inverse sigmoidal curve of changes in ionised Ca vs PTH change. what does the midpoint of the graph show? |
the sensitivity of the parathyroid gland calcium sensing receptors to ionised Calcium |
|
|
primarily in which 2 organs is vitamin D synthesised |
liver and kidneys |
|
|
what step does the PTH have an effect on the synthesis of 1,25 DHCC |
the second step which is a hyroxylation step |
|
|
what can the 2 main causes of hypocalcaemia be |
PTH problem vitamin D problemo |
|
|
what is the cause of the PTH problem which leads to hypocalcaemia |
hypoparathyroidism -neck surgery -idiopathic -Mg defficiency |
|
|
what are the 2 causes of the Vitamin D problem which leads to hypocalcaemia |
vitamin D defficiency - can be because of malabsorption or little exposure to sunlight
renal disease - kidneys fail to make active form of vitamin DHCC |
|
|
what are the 3 main causes of hypercalcaemia |
PTH problem vitamin D problem malignancy
|
|
|
what is the main cause of the PTH problem which leads to hypercalcaemia |
hyperparathyroidism - adenoma of parathyroid gland this leads to Calcium increases and PTH increases
(adenoma -a benign tumour formed from glandular structures in epithelial tissue) |
|
|
what is the main cause of the vitamin D problem which leads to hypercalcemia |
inappropriate dosage of vitamin D dosage |
|
|
what is the main cause of the malignancy which leads to hypercalcaemia |
PTH related peptide - lung cancer, breast cancer, multiple myeloma calcium increases and PTH suppressed |
|
|
what is the main role of phosphate in the body |
skeletal development and bone mineralisation
also
compositon of cell membranes, nucleotide structure and cell signalling |
|
|
what are the main organs involved in phosphate homeostasis |
kidneys gut bones |
|
|
what are the main hormones involved in phosphate homeostasis |
PTH FGF 23 1, 25 - DHCC |
|
|
is the absorption of phostphate in the intestine more or less rigidly regulated than Ca |
less rigidly regulated |
|
|
what increases the amount of phosphate |
1,25-DHCC |
|
|
is phosphate plentiful in diet? |
yes... |
|
|
what % of phosphate is protein bound |
15-20% |
|
|
where are the 2 places in the kidney where phosphate gets reabsorbed |
proximal and distal convoluted tubule |
|
|
what is the relative percentages of phosphate reasbsorption in the proximal convoluted tubule and the distal convoluted tubule |
75 % reabsorbed in proximal convoluted tubule 25 % reabsorbed in distal convoluted tubule |
|
|
through the renal tubule what are the the 2 hormones which inhibit reabsorption in the kidney? |
FGF-23 PTH |

