![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
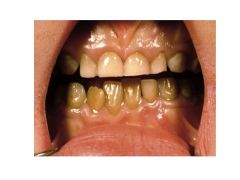
What is jaundice?
Best places to detect? |
Yellowish discoloration of tissue resulting from deposition of bilirubin
Most apparents in sclera and underneath tongue |
|
|
RBC destroyed-->unconjugated bilirubin released from heme degradation-->liver (to make unconj'd bilirubin water soluble)-->bile duct-->intestine-->colonic bacteria metabolize-->excreted
|
...
|
|
|
What are the major sources of bilirubin?
|
Senescent RBCs (70%)
Prematurely destroyed RBCs (20%) Turnover of hemoproteins (myoglobin, cytochromes)--10% |
|
|
How is unconjugated bilirubin formed? Describe each step.
Where does this take place? |
During RBC breakdown, heme is catabolized to unconjugated bilirubin:
Heme-->Biliverdin (via Heme oxygenase) + CO Biliverdin-->Bilirubin (via biliverdin reductase)--AKA unconj'd bilirubin This occurs in liver, spleen. |
|
|
Describe the steps by which unconjugated bilirubin becomes conjugated.
Include transport of molecules, enzymes, receptors. |
Unconj'd bound to albumin-->liver-->UCB taken up by hepatocytes via OATP2 (albumin dissociates)-->UCB bound by ligandin (GST) to prevent efflux into liver sinusoids
Unconj'd Bilirubin-->bilirubin via UGT |
|
|
Why must bilirubin be conjugated?
|
Unconj'd bilirubin isn't soluble.
Conjugated bilirubin is water soluble and facilitates rapid excretion into bile. |
|
|
Why are neonates often born with jaundice?
|
Low physiologic activity of UDP (UDP-Glucuronosyl Transferase--GST) enzyme at birth (low levels of conjugation).
Inc'd intestinal reabsorption due to lack of gut flora to degrade bilirubin |
|
|
What becomes of conjugated bilirubin?
Begin in hepatocyte. Describe all steps. |
Enters bile canaliculus via MRP2
Drained into duodenum Hydrolyzed by colonic bacteria to UROBILOGEN; excreted in feces 10-20% re-enters portal system and reexcreted by liver. Small fraction filters across renal glomerulus and excreted in urine. |
|
|
Conjugated bilirubin AKA
|
Direct bilirubin
|
|
|
Conjugated vs Unconjugated Bilirubin:
Which is present in higher serum levels? |
Indirect bilirubin (unconjugated)
|
|
|
Why is unconjugated bilirubin in urine always an abnormal finding?
|
Unconj'd bilirubin always bound to albumin; shouldn't have a protein slipping through glomerulus!
|
|
|
Causes of hyperbilirubinemia.
|
Overproduction of bilirubin (hemolysis)
Impaired uptake, conjugation, excretion of bilirubin Regurgitation of bilirubin from damaged hepatocytes/bile ducts |
|
|
Causes of indirect hyperbilirubinemia.
|
Hemolytic disorder
Gilbert's Syndrome Cringler-Najjar Syndrome Rifampin Probenacid |
|
|
Causes of direct hyperbilirubinemia.
|
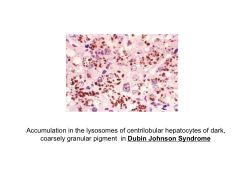
Dubin-Johnson Syndrome
Rotor's Syndrome |
|
|
What would cause an increased production of bilirubin?
|
Hemolysis
Ineffective erytrhopoiesis Hematoma |
|
|
Effect of hemolysis on bilirubin.
When does hemolysis occur? |
Modest increase in production of UNCONJUGATED bilirubin (<5 mg/dl)
Spherocytosis, G6PD deficiency, autoimune disorders |
|
|
Effect of ineffective erythropoiesis.
When does ineffective erythropoiesis occur? |
Increased production of UNCONJUGATED bilirubin.
Causes: Fe deficiency B12 deficiency Folate deficiency Pb poisoning |
|
|
Laboratory evidence of hemolysis.
|
Schistocytes
Elevated retic count Dec'd haptoglobin |
|
|
What drugs reduce hepatic clearance of bilirubin?
How? |
Rifampin, probenacid compete with bilirubin binding ligand (Ligandin--AKA GST) needed to prevent efflux of unconj'd bilirubin back into circuln.
|
|
|
This syndrome exhibits no UGT activity.
What is plasma bilirubin like? |
Crigler-Najjar Type I Syndrome; plasma INDIRECT bilirubin 20-50!
|
|
|
This syndrome exhibits markedly reduced UGT activity.
What is plasma bilirubin like? |
Crigler-Najjar Type II Syndrome
Plasma indirect bilirubin 6-25 |
|
|
This syndrome exhibits decreased UGT activity.
What is plasma bilirubin like? |
Gilbert's Syndrome
Bilirubin <3-6 |
|
|
These syndromes result in direct hyperbilirubinemia.
|
Dubin-Johnson Syndrome
Rotor's Syndrome These are both uncommon and benign. |
|
|
These syndromes interfere with UGT activity.
|
Crigler-Najjar I, II
Gilbert's Note: This results in indirect hyperbilirubinemia |
|
|
These syndromes interfere with MRP2 activity.
|
Dubin-Johnson
Rotor Note: This results in direct hyperbilirubinemia (MRP2 = transport prot for conj'd bilirubin to bile canaliculus) |
|
|
Absolute height of ALT elevation does not ________.
|
Height of ALT does NOT correlate with severity of clinical outcomes!
|
|
|
Causes of elevated ALP.
|
Bile duct obstruction
Intrahepatic cholestasis |
|
|
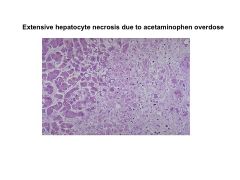
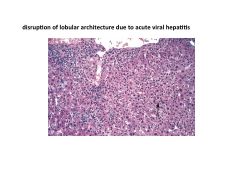
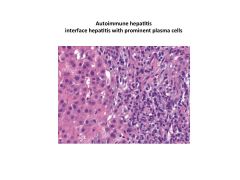
Causes of elevated ALT/AST.
|
Viral hepatitis
Tylenol (predictable, dose-dependent) EtOH Isoniazid (unpredictable dose-independent) Autoimmune hepatitis |
|
|
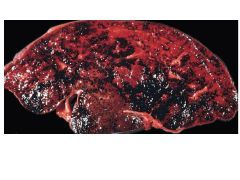
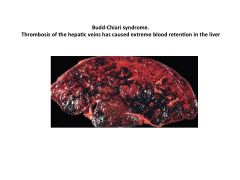
What is Budd-Chiari syndrome?
|
Thrombosis of hepatic veins causing extreme blood retention in liver. Causes elevated AST/ALT.
|
|
|
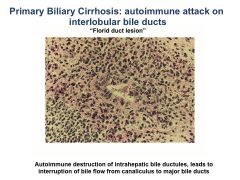
What is cholestasis?
Effects? |
Interruption of bile formation
Hepatic retention of products normally secreted into bile (bile salts) Presentation: Jaundice hypercholesterolemia If progressive, fibrosis, cirrhosis, liver failure |
|
|
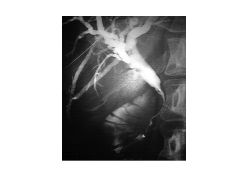
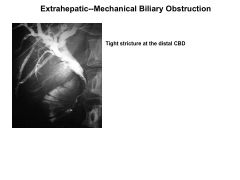
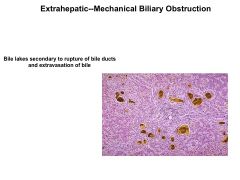
Extrahepatic vs Intrehepatic Cholestasis:
Causes |
Extrahepatic: biliary obstruction--cholangiocarcinoma, panc ca, ampullary ca
choledocholithiasis (obstruction of CBD) Primary sclerosing cholangitis AIDS cholangiopathy Chronic pancreatitis Intrahepatic: transport protein defect; Will not exhibit signs of obstruction; Drug toxicity***--Abx Nonhepatobiliary sepsis TPN ALP: >3x ALT/AST: <5x |
|
|
PFIC1 vs PFIC2 vs PFIC3:
Gene defects Effect Symptoms |
PFIC1: FIC1 (defective phospholipid, bile salt transport)
PFIC2: BSEP (bile salt export pump) PFIC3: MDR3 (phospholipid export) All result in intrahepatic cholestasis All exhibit PRURITIS, inc'd serum bile acid |
|
|
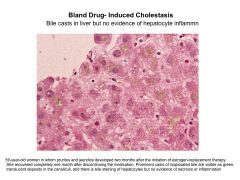
Bland cholestasis:
Presentation Lab Values Drug Causes |
Severe pruritis
Minimal rise in ALT Causes; E2, anabolic steroids, tamoxifen |
|
|
Cholestasis with hepatitis:
Presentation Lab Values Drug Causes |
Abdominal pain
Jaundice Pruritis ALT>2-5x Causes: Chlorpromazine, erytrhomycin, amox-clavulanate, NSAIDs |
|
|
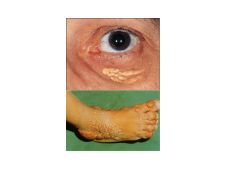
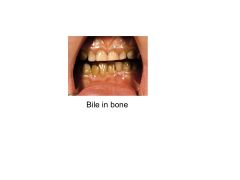
Complications of retention of bile within liver.
|
Pruritis
Bile acids destroy membranes, promote apoptosis, fibrosis Lipid retention results in xanthoma, neuropathy |
|
|
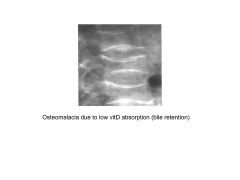
Complicaitons of retention of less bile in bowel (due to retention in liver).
|
Steatorrhea, weight loss
Low Vit A/D/E/K (night blindness, osteomalacia, neuropathy, easy bruising--respectively) |
|
|
Pruritis:
Treatment |
Cholestyramine--resin that sequesters bile acids; results in bad tase, bloating, constipation
Liver transplantation in severe intractable pruritis |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|

|
|
|
|
|
|
|

