![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
6 Cards in this Set
- Front
- Back

Hx:67yo F sustained an ACL tear while playing basketball when she was 35yo. She has noted progressive leg deformity and episodes of giving way, and now has pain preventing activity. Non-op has failed to provide relief. Treatment should consist of? 1-Opening wedge high tibial osteotomy with autograft; 2-Closing wedge proximal tibial osteotomy; 3-Medial interpositional arthroplasty
4-Medial UKA; 5-TKA |

Total knee arthroplasty can be used to provide predictable pain relief in a patient with unicompartmental and tricompartmental degenerative disease and varus malformation of the knee and for this patient is the best option.Ans 5
|
|

Hx:71yo M s/p L THA x10 ys ago. 18 mths ago he began having hip and thigh pain. Over the past 6 weeks, the pain has become excruciating and he has been unable to ambulate, even with the aid of a walker. He has mild pain with passive internal and ER of the hip. He is unable to ambulate in the office. Laboratory values are notable for a WBC of 10,300, CRP of 0.2, and ESR of 13. A radiograph is provided in figure A. Which is the best treatment option? 1-Radionuclide bone scan and MRI
2-ORIF w/ a cable plate and allograft strut 3-Revision arthroplasty with a fully coated cementless stem, cable wiring, and bone graft 4-Revision arthroplasty with a modular, tapered stem and bone grafting of the diaphyseal fixation 5-Revision arthroplasty with a total femur prosthesis |
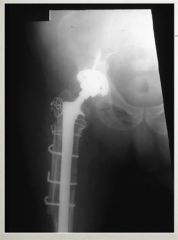
periprosthetic femur fracture, with a loose femoral stem, and a Paprosky IIIA femoral defect. This is best treated with a fully-coated cementeless stem with metaphyseal onlay allograft, Type IIIA: severe metaphyseal bone loss with greater than 4 cm of diaphyseal bone preservation for distal fixation.
Type IIIB: severe metaphyseal bone loss and less than 4 cm of diaphyseal bone preservation for distal fixation Type IV: extensive metaphyseal and diaphyseal bone loss. Of importance, Type IIIA may be treated with a fully coated stem. Type IIIB should consider a tapered, modular stem and/or bone grafting. Type IV likely need a megaprosthesis. In this patient, given the preserved diaphyseal bone, revision arthroplasty with a fully coated femoral stem is the most appropriate treatment.Ans3 |
|

Hx:91yo M w/ a hx of chronic leukemia and dementia falls and sustains the hip fx . He undergoes a hemiarthroplasty through a posterior approach. 3 wks later he dislocates the hip arising from the toilet seat. The patient undergoes a CR and is placed in a hip abd brace. 1 mth later he returns to clinic complaining of pain and inability to bear weight through the leg. Which of the factors has MOST likely contributed to the instability of the hip hemiarthroplasty? 1-Femoral stem subsidence; 2-Inadequate anteversion of the femoral component; 3-Inadequate fem stem neck length; 4-Post approach; 5-Pt gender
|

two greatest factors contributing to the instability include the patient's dementia and the posterior approach to the hip. The posterior approach has been shown in numerous studies to lead to a greater rate of dislocation in both hemiarthroplasty and THA when compared to lateral, anterolateral, and anterior approaches.Ans4
|
|

Hx:72yo F returns to clinic for 15 yr f/u of LTHA. She ambulates w/out any assistive devices, has no pain, and denies any recent fevers or systemic illness. A xray is provided in fig A. Which of the following is the best treatment option? 1-F/u xray in 1 yr
2-F/u xray in 5 ys; 3-Revision surgery with fem head and polyethylene exchange and retroacetabular bone grafting; 4-Revision of acetabular component with jumbo cup and femoral head exchange 5-Revision of acetabular component with jumbo cup and femoral stem revision |

osteolytic lesions behind the acetabular cup and eccentric wear of the polyethylene with superior migration of the femoral head within the cup. Options 1 and 2 are poor choices because the osteolysis must be addressed to prevent further bone loss and eventual loosening of the implant. The acetabular cup remains in acceptable position and does not need to be revised unless found to be grossly loose intraoperatively. The osteolytic lesions need to be addressed with bone grafting to prevent cavitary bone loss. The femoral stem shows no indication of loosening or osteolysis around the stem and can be retained.Ans 3
|
|

Fig A hip xray of a 72yo F who had had a R THA 15 yrs previously. CT imaging of the affected hip shows non-contained defects in both the anterior and posterior columns of the peri-acetabular region affecting >50% of the wt bearing surface. Which of the following revision procedures would restore the most acetabular bone stock and be most appropriate for this patient? 1-Morselized allograft and/or autograft bone, combined with a cemented acetabular component; 2-Acetabular revision with use of a bilobed cementless component and morselized allograft; 3-Morselized allograft and/or autograft bone, combined with a cementless acetabular component; 4-Revision using an ilioischial reconstruction ring acetabular component and structural corticocancellous graft
5-Revision using a roof ring acetabular component and structural corticocancellous graft |

ilioischial reconstruction rings performed by 1 surgeon over a 15-year period. On the acetabular side, allograft failure was the most common complication. Illustration A shows an example of an ilioischial reconstruction ring, and Illustration B shows this reconstruction ring in situ, In cases of minor, contained, acetabular defects, morcellized allograft and/or autograft bone, combined with a cemented or cementless acetabular component can lead to successful reconstruction.Ans4
|
|

Performing an isolated release of the popliteus tendon during a TKA is most appropriate in which of the following scenarios? 1-Valgus deformity that is tight in extension; 2-Varus deformity that is tight in extension 3-Valgus deformity that is tight in flexion; 4-Valgus deformity that is tight in both flexion and extension; 5-Varus deformity that is tight in flexion
|

An isolated release of the popliteus tendon during TKA is most appropriate in the setting of a valgus knee deformity that is tight in flexion.
Lateral collateral ligament release is most appropriate for a valgus deformity that is tight in both flexion and extension. Iliotibial band release is indicated if the knee is tight in extension. For varus knee deformities, femoral and tibial osteophyte removal, release of the deep MCL, release of the posteromedial corner, release of the attachment of the semimembranosus, and partial superficial MCL release may be sequentially indicated to achieve coronal balancing.Ans3 |

