![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
What is the normal rate for the SA node, above which is tachycardia and below which is bradycardia?
|
60 - 100 bpm
|
|
|
What are 3 ways to determine rate on an EKG?
|
1. (complexes/6 seconds)*10 where 6 seconds = 30 boxes
2. 300/number of large boxes between two QRS complexes 3. 100, 150, 100, 75, 60, 50 |
|
|
In what sequence and in what pace do alternative pacemakers jump in when the SA node fails? And what is it called when SA node causes no other node to fire?
|
Atrial ectopic foci - 60 to 80 bpm
AV node - 40 to 60 bpm Ventricular ectopic foci - 20 to 40 bpm it's called overdrive suppression |
|
|
Define the following: PR interval, PR segment, QRS interval, QT interval, ST interval, ST segment, RR interval.
|
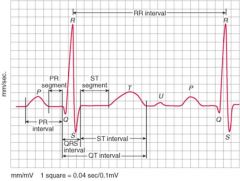
PR interval - beginning of P wave to beginning of Q wave
PR segment - end of P wave to beginning of Q wave QRS interval - beginning of Q wave to end of S wave RR interval - peak of one R wave to the next ST segment - end of S wave to beginning of T wave ST interval - end of S wave to end of T wave QT interval - beginning of Q wave to end of T wave |
|
|
What is the first characteristic to look for when defining normal sinus rhythm (NSR)?
|
P of aVR is always negative
P of II is always positive |
|
|
Describe the quality of a Wandering Atrial Pacemaker rhythm.
|
since the pacemaker discharges from different atrial locations, the P wave has different shapes and the PR intervals (representing the time it takes for the P wave to get to the ventricles) will also vary.
if HR > 100, WAP => multifocal atrial tachycardia |
|
|
Describe the quality of Sinus arrhythmia.
|
all the P waves and PR intervals are identical because they come from the same sinus node, but the rate will be variable. it's common for this to manifest as an HR increase during inspiration and a decrease during expiration.
|
|
|
What are the five supraventricular arrhythmias?
|
1. premature atrial & AV junctional (nodal)
2. paroxysmal supraventricular tachycardias 3. AV junctional rhythms 4. atrial flutter 5. atrial fibrillation |
|
|
What causes a premature atrial or AV junctional premature beat?
|
some ectopic foci in the left or right atria that is NOT the SA node
|
|
|
What are the six major features of APBs (atrial premature beat) and PACs (premature atrial contraction)?
|
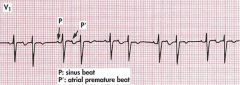
1. Atrial depolarization is premature
2. QRS of the PAC often preceded by a P wave with a slightly different shape or PR interval 3. After the PAC there is generally a slight pause 4. QRS of the PAC is usually identical or very similar to normal beats 5. Occasionally result in aberrant ventricular conduction so that the QRS is wider than normal 6. PAC can be so premature that it is not conducted because AV is still in refractory period |
|
|
What is the cause of an APB or a PAC in a normal heart and what could it be the precursor to?
|
causes: stress, caffeine, sympathomimetic agents
may be the precursor of A-fib or flutter |
|
|
What constitutes a Paroxysmal Supraventricular Tachycardia (PSVT) and what are the three major types?
|
premature beat occurring in a sudden run of three or more beats. there is a marked constant HR usually.
1. atrial tachycardia 2. AV nodal reentrant tachycardia 3. AV reentrant (bypass tract) tachycardia |
|
|
What is the quality of an atrial tachycardia PSVT?
|
1. three or more consecutive PACs
2. ectopic pacemaker in the R or L atrium |
|
|
What is the quality of an AV nodal reentrant tachycardia (AVRNT) PSVT?
|
1. rapid (140-250 bpm) but regular rhythm
2. P waves hidden in QRS 3. when visible, P waves are negative in II because of retrograde condution 4. impulse is rapidly circulating, to P wave location will predictably cycle through positions |
|
|
What is the quality of an AV reentrant tachycardia PSVT?
|
1. due to abnormal tract of cardiac muscle that connects the atria and ventricles, circumventing the AV node
2. normal impulse will stimulate ventricles, but then travel back up to the atria via the bypass tract 3. negative or isoelectic P wave will occur after the QRS complex |
|
|
What is the EKG p wave result of AV junctional rhythms and why?
|
Because of the resulting vector and retrograde atrial stimulation, the P wave will be reversed of normal in the aVR and II leads.
Normal P vector will go toward II, so II will be + and aVR will be - AV junctional rhythm P wave vectors stimulate the atria from below, so the II lead P wave will be (-) and aVR will be (+) |
|
|
Where in respect to the QRS will a P wave exist in an AV junctional rhythm?
|
they can be before, after, or buried in a QRS
|
|
|
How is atrial flutter defined?
|
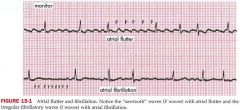
reentrant arrythmia per atrial stimulation ~ 300 bpm. ventricular rate varies depending on ability of AV junction to transmit atrial signal. looks like a series of P waves that don't get propogated, so has a very defined sawtooth pattern.
|
|
|
Define atrial fibrillation.
|
one of the most common arrythmias, atrial fibrillation has an atrial depolarization rate of 350 to 600 bpm. there are irregular wavy F waves like the sawtooth waves, but very irregular... not really sawtoothy, but caused by similar stimulation. the ventricular rate is irregularly irregular.... yeah...
|
|
|
What is lone atrial fibrillation and what is holiday heart syndrome?
|
lone atrial fib is a recurrent or chronic AF in pts without other clinical evidence of heart disease
holiday heart syndrome is onset of AF because of excessive alcohol consumption |
|
|
What is the cause of 15-20% of CVAs (cerebrovascular accidents) in nonrheumatic pts?
|
atrial fib
|
|
|
What are the three broad types of AF?
|
paroxysmal - stops spontaenously within 7 days and usually within 48 hours
persistent - last more than 7 days and requires cardioversion permanent - last indefinitely and persists even if cardioversion is attempted |
|
|
What are the three objectives of AF treatment?
|
1. achieving rate control
2. restore NSR 3. decrease CVA risk |
|
|
What are digitalis and intravenous calcium channel blockers used for and when should they not be used?
|
digitalis, IV Ca channel blockers like diltiazem are AF rate controlling pharmaceuticals, but are contraindicated with Wolff-Parkinson_White syndrom and atrial fibrillation
|
|
|
What is first line pharmaceuticals for AF tx?
|
class IC agents like flecainidice or propafenone
|
|
|
What is the mechanism of action of an IC class antiarrhythmic agent?
|
Class Ic antiarrhythmic; slows conduction in cardiac tissue by altering transport of ions across cell membranes; causes slight prolongation of refractory periods; decreases the rate of rise of the action potential without affecting its duration; increases electrical stimulation threshold of ventricle, His-Purkinje system; possesses local anesthetic and moderate negative inotropic effects
|
|
|
Warfarin has been effective in decreasing the risk of emboli by 45-85% of pts with nonrheumatic AF. What is the criteria for tx?
|
international normalized ratio (INR) is from 2.0 to 2.5
INR is a ratio of pts prothrombin time (time for blood to clot) over a normal prothrombin time |
|
|
Of the three rapid ectopic rhythms, paroxysmal tachycardia, flutter, and fib, what are their associated ranges of rate? Also, what is paroxysmal mean?
|
150 - 250 paroxysmal
250 - 350 flutter 350+ fib paroxysmal - sudden onset, cessation, or both |

