![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
26 Cards in this Set
- Front
- Back
|
What is the difference between glucocorticoids, corticosteroids, and mineralcorticoids?
|
Glucocorticoids (naturally cortisol) and mineralcorticoids (Naturally aldosterone) are encompassed by corticosteroids
|
|
|
What is the primary hormone of stress?
|
Cortisol
|
|
|
What percentage of corticosteroid hormones float free and what do the rest bind to?
|
10 percent is free and 90% are bound to corticosteroid binding globulin (CBG)
|
|
|
What affects corticosteroid binding globulin levels?
|
Increased CBG - Pregnancy, estrogen, and hyperthyroidism
Decreased CBG - Protein deficiency, hypothyroidism, and genetic defects |
|
|
What is the core compound/structure used to synthesize all glucocorticoids?
|
Cholesterol
|
|
|
How do steroids induce their effects?
|
Steroids once near their target cell dissociate from the binding protein and enter the cytoplasm where they bind to receptors which dissociates heat shock proteins from the receptor allowing the steroid receptor complex to enter the nucleus and bind to a DNA promoter region causing expression modifications resulting in cellular effects
|
|
|
What are the effects of anti-inflammatory steroids?
|
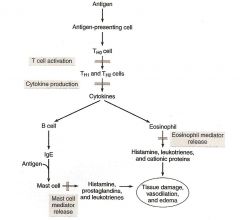
They inhibit:
T-cell activation Cytoking production Mediatory release They decrease: Capillary permeabillity expression of COX-2 prostaglandin, Leukotriene, and platelet activating factors |
|
|
What is the most common route of administration for glucocorticoids and what can be done if they are unable to tolerate that route?
|
Most commonly oral route is used. However, if a patient cannot tolerate it typically IM or SC is used.
|
|
|
What is the primary site of glucocorticoid inactivation?
|
Phase I metabolism by Cytochrome P450 in the liver followed by phase II glucuronidation
|
|
|
What is the primary mode of excretion for the glucocorticoids?
|
Renal clearance and uinary excretion as glucuronide metabolites
|
|
|
What is the difference between biological half life and plasma half life of a drug?
|
Biological half life is concerned with the amount of time increase in transcription persists after drug administration
Plasma half life deals with how long before drug is converted to its metabolite |
|
|
What is meant by mineralcorticoid potency?
|
Some drugs have aldosterone like effects as well. It is the measure of this overlap
|
|
|
What is meant by glucocorticoid potency?
|
Strength of the drug's anti-inflammatory effects
|
|
|
How are glucocorticoid divided and does mineralcorticoid function play a role in this division process?
|
Glucocorticoids are divided into short, intermediate, and long acting drugs. However, mineralcorticoid potency does not increase ie long acting glucocorticoids very potent glucocorticoid activity but practically no mineralcorticoid activity
|
|
|
What are the adverse effects of long term glucocorticoid therapy?
|
Brittle bones
Decreased resistance to infections Psychological dependence (due to hypothalamic negative feedback) Suppression of hypothalamic-pituitary-adrenal (HPA) axis Impaired wound healing moon face, hump on the back, and a thick trunk Purpura Excess Acne Muscle weakness (due to Hypokalemia) Glaucoma Retardation of growth Shakiness and Tremor Weight gain (mineralcorticoid activity) |
|
|
What are the short acting corticosteroids?
|
Hydrocortisone
Cortisone |
|
|
What is the utility of hydrocortisone?
|
Short-acting corticosteroid:
biological half life - 8-12 hrs. plasma half life - 30min Localized inflammatory conditions and over the counter creams Relative anti-inflammatory potency is 1 (all others are based on hydrocortisone so this one is 1) |
|
|
What are the intermediate-acting corticosteroids?
|
All have biological half life of 18-36 hours
Prednisone Prednisolone Methylprednisolone Triamcinolone |
|
|
What is the utility of prednisone?
|
Intermediate-acting corticosteroid:
arthritis, astham, copd, ulcertative colitis, Crohn's Disease, rheumatoid arthritis, and dermatologic disorders Relative anti-inflammatory potency: 4 Metabolized in the liver to active metabolite Plasma Half life 60 min - oral only |
|
|
What is the utility of prednisolone?
|
Intermediate-acting corticosteroid:
opthalmic disorders and respiratory distress Plasma life - 60 min Oral and injectable |
|
|
What is the utility of methylprednisolone?
|
Intermediate acting corticosteroid:
rheumatoid arthritis, ulcerative colitis, severe alcoholic hepatitis Plasma life 60 min oral injectable Many side effects |
|
|
what is the utility of triamcinolone?
|
Intermediate-acting corticosteroid:
No mineralcorticoid activity Opthalmic disorders and respiratory disease Plasma life 60 min oral injectible |
|
|
What are the long acting corticosteroids?
|
All have biological half lives of 36-54 hours used in individuals not responding to NSAIDS as a last resort:
Betamethasone Dexamethsone |
|
|
What is the utility of Betamethasone?
|
Long-acting corticosteroids:
Respiratory diseases, respiratory distress syndrome, local inflammatory conditions Relative anti-inflammatory potency 25 plasma life +300 min oral, topical, injectible |
|
|
What is the utility of Dexamethasone?
|
Long-acting corticosteroid:
Lupus and Rheumatoid Arthritis Relative potency 25 Plasma life 110-210 min. oral, topical, injectable |
|
|
What is a major insulin related side effect of corticosteroid therapy?
|
By inhibiting the functionality of insulin and increasing circulating glucose the potential for symptomatic type II diabetes effects increases
|

