![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
27 Cards in this Set
- Front
- Back
|
What are two forms of heart failure and what factors are associated with them?
|
High Output - CO is normal just isn't enough for body's metabolic needs
Low Output - Primary Heart Fialure (due to mechanical or metabolic disease) or Secondary Heart Failure (attributed to diseases in other organs) |
|
|
Describe the various stages and associated symptoms of heart failure patients.
|
Asymptomatic - CO is decreased with no symptoms
Moderate - Fatigue on exertion or exercise with nocturnal dyspnea Severe - exreme fatigue on exertion, congested lungs, peripheral pitting edema |
|
|
What type of Cardiomegaly would be present in a condition of CHF?
|
Eccentric or cardiac dilation
|
|
|
What comprises the vicious cycle of CHF?
|
Decreased blood mobility due to mechanical dysfunction perpetuating baroreflex response and RAS response yeilding increased TPR, HR, preload, and reabsorption of sodium and in addition a hypervolemic state.
|
|
|
What are the two types of Heart Failure patients that will be treated with pharmacotherapy and through what route will they be treated?
|
Compensated - oral drugs
Decompensated - parenteral drugs |
|
|
What are the positive ionotropic agents used to treate heart failure and how do they function?
|
They are cardiac glycosides (digitalis drugs) that increase force of contraction int he heart and raise CO. Cardiac glycosides include Digoxin, Digitoxin, and Oubain
Dopamine Dobutamine Phosphodiesterase Inhibitors |
|
|
What is the route of elimination for Digoxin and Digitoxin and their half lives?
|
Digoxin - 1.5 days renal excretion
Digitoxin - 7 days Hepatic Metabolism |
|
|
How do the cardiac glycosides actually work?
|
They inhibit Na/K ATP-ase which is used to reestablish the resting membrane potential during diastole by pumping Na out and K in. This is coupled to a Na/Ca exchanger which gets rid of Extra Ca in exchange for one Na. So block ATPase block Ca from leaving (cake!) Increased Ionotropy!
|
|
|
What are some other effects of glycosides besides the ATPase pump effect?
|
Increased Baroreflex sensitivity (I wonder if this should be decreased)
Decreased Sympathetics Decreased sensitivity to Catecholamines Increased parasympathetic tone and increased cardiac sensitivity to Ach |
|
|
What are the more severe side effect of digitalis?
|
Incredibly toxic with narrow therapeutic dose
Large effects on serum K levels (hypokalemia) AV Block! Ventricular tachycardia Drug interactions |
|
|
How does Dopamine work for Heart Failure?
|
DA1, DA2 (Increase NE), Beta1, and Alpha 1 agonist.
Increases HR, increases ionotropy DA1 effects are vasodilation of renal and splanchnic arteries, increased GFR, and increased urine |
|
|
How does Dobutamine work for Heart Failure?
|
Beta 1 agonist that at low doses can increase ionotropy without increasing HR, essentially increasing CO without increasing demand (I say Bullshit! but whatever)
Side Effect - Long term use tolerance |
|
|
How do Phosphodiesterase Inhibitors work and what are 2?
|
Inamrinone and Milrinone
Heart: Selectively blocks Phosphodiesterase III causing increased cAMP --> increased contraction Peripheral Vasculature: Blocks phossphodiesterase III increasing cGMP --> vasodilation --> decrease preload and afterload (sounds like peripheral backup to me haha) |
|
|
What are the Heart Failure vasodilator drugs and what do they do?
|
Na-nitroprusside - NO --> dilation of arteries and veins reducing preload and afterload (CN poisoning in renal failure patients)
Nitroglycerin - Venodilator reducing preload (at higher doses arterial dilator reducing afterload) Nesiritide - BNP --> Natriuretic, diuretic, and vasodilator (IV, no proarrhythmic potential) |
|
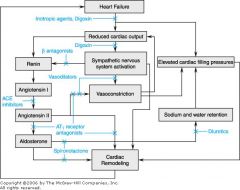
Do you Like Pictures??
|
Goood!!!
|
|
|
What vasodilators would you use acutely and which would you use chronically for Heart Failure Control?
|
Acute - Sodium Nitroprusside, Nitroglycerine, Nesiritide
Chronic - Hydralazine, Isosorbide dinitrate |
|
|
What effect does Hydralazine have and what is a primary side effect?
|
Causes arterial vasodilation leading to decreased afterload
Side effect - orthostatic hypotension leading to syncope Low compliance due to Q4hr |
|
|
What effects does isosorbide dinitrate have?
|
Decreases preload by venodilation
|
|
|
What are the benefits of captopril and enalapril and what are they?
|
They are ACE inhibitors.
They can be used to treat heart failure by reducing preload and afterload. AngII is a powerful vasoconstrictor and potentiates NE release and action - Blockade reverses these effects. AngII also causes Aldosterone release |
|
|
What is a major heart remodeling effect of Angiotensin II and a secondary heart remodeling effect?
|
Ang II is a cardiac growth hormone (hypertrophic agent)
It causes release of aldosterone which is also a hypertrophic agent (so not just big but biggie biggie can't you see?) |
|
|
What are the angiotensin receptors and what do they do?
|
AT1 - major vasoconstrictor
AT2 - ?? maybe counteracts aldosterone so Vasodilator (possibly) |
|
|
What are some side effects of ACEi
|
contraindicated in pregnancy (I don't know why!)
Persistent dry cough due to bradykinin (which is normally broken down by ACE) escape phenomenon because of alternative production of Ang II |
|
|
What are the angiotensin Receptor Antagonists and what do they do?
|
They are Saralasin and Candisartin
They block AT1 but not AT2 They prevent escape phenomenon and maintain breakdown of bradykinin |
|
|
What are some diuretic drugs that can be used for treatement of Heart Failure?
|
Loop Diuretics - Furosemide, bumetanide, torsemide
Thiazides K-Sparing drugs - Spironolactone (causes reverse remodeling in the ventricles) |
|
|
What are the beta agonists that Dr. Varner wants us to know huh?
|
Carvedilol and Metoprolol
|
|
|
What does Carvedilol do and how does it work?
|
It is a beta1, beta2, and alpha1 blocker (ratio of 10:1 beta alpha) Causes blockade of beta plus vasodilation from alpha
|
|
|
How many stages of heart failure is there and what are they treated with (ambulatory patients)?
|
Four stages I-IV
All treated with Diuretic All treated with ACEi (replace with ARBs, Hydralazine/Isosorbide dinitrate if intolerant) Almost all treated with beta blocker Digoxin is reserved for a-fib or a-flutter b/c it can control reentry circuits, slow AV conduction, and increase ionotropy |

