![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
62 Cards in this Set
- Front
- Back
|
What is the width and length of the spinal cord? |
2cm and 42-45cm |
|
|
Where does the spinal cord start? Where does it end in adults? Where does it end in newborns? |
- medulla oblongata - L1/L2 - L3/L4 |
|
|
What is the name of the 2 enlargements found in the spinal cord and where are they found? What do they do? |
- cervical enlargement (C4-T1) and lumbar enlargement (T9-T12) - cervical enlargement: point of entry for nerves to and from upper limbs - lumba enlargement: point of entry for nerves to and from the lower limbs |
|
|
What is the name for the region of the spine where the spinal cord ends? What anchors the spinal cord to the coccyx? |
- conus medullaris - filum terminale |
|
|
How many pairs of spinal nerves are there and how many in each region? |
- 31 - cervical 8 - thoracic 12 - lumbar 5 - sacral 5 - coccygeal 1 |
|
|
Which roots in the spinal cord are responsible for sensory and motor functions - respectively |
- dorsal roots: sensory - ventral roots: motor |
|
|
What is the name of the collection of spinal nerves which extend beneath T2? |
- cauda equina |
|
|
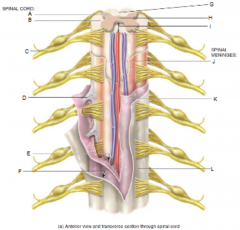
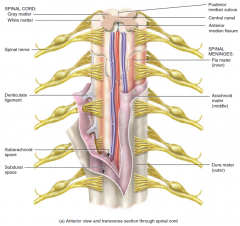
From superficial to deep, what are the three layers of the meninges? |
- dura mater, arachnoid mater and pia mater |
|
|
From superficial to deep, an including all spaces, what are the layers of the meninges (7)? |
- subpial space - pia mater - subarachnoid space - arachnoid mater - subdural space - dura mater - epidural space
|
|
|
Which space of the meninges contains CSF? Which space of the meninges contains interstitial fluid? |
- subarachnoid space - subdural space |
|
|
|
|
|
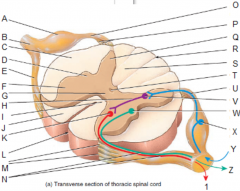
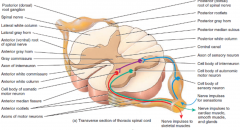
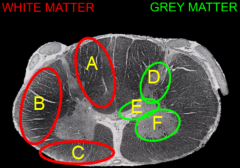
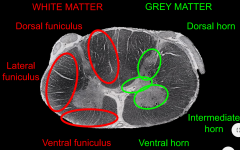
What is present is white matter? What is present in grey matter (4)? |
- bundles of unmyelinated axons - dendrites, neuronal cell bodies, unmyelinated axons and neuroglia |
|
|
What is the function of neuroglia? |
- maintainhomeostasis, form myelin, and provide support and protection forneurons in the central and peripheral nervous systems |
|
|
What divides the left and right horns in grey matter? |
- grey commissure |
|
|
What is the name of the anterior and posterior grooves o the spinal cord? |
- anterior medianfissure and the posterior median sulcus |
|
|
What types of nerve fibres are located in the dorsal and ventral horns, respectively |
- dorsal: sensory - ventral: motor |
|
|
Which regions of the spinal cord have additional horns in their grey matter? What is their function? |
- thoracic and lumbar - autonomic motor nuclei which regulate cardiac and smooth muscle and glands |
|
|
What is the difference between ascending and descending tracts in white matter? |
- ascending: sensory - descending: motor |
|
|
What are the different regions of white matter? |
- anterior (ventral) columns - posterior (dorsal) columns - lateral white columns |
|
|
|
|
|
|
|
|
Describe gray matter looks diffferent in different regions of the spinal cord |
- larger ventral horns corresponds to greater motor involvement - larger dorsal horns corresponds to greater sensory involvement |
|
|
Describe the dermatomes of the body |

|
|
|
Describe the myotomes of the lower limbs |
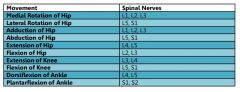
|
|
|
What are the 4 different types of nerve fibre? Describe their speed What are their sensory receptors? |
- A alpha, A beta, A delta and C - 80-20, 35-75, 5-30 and 0.5-2 (metres/second) - proprioceptors of skeletal muscle; mechanoreceptors of skin; pain and temperature; and temperature pain and itch |
|
|
Define nociceptors |
- free and branchingunmyelinated nerve endings that signal when body tissue is beingdamaged, or at risk of being damaged |
|
|
What type of channels are involved in the activation of nociceptors? |
- mechanically gated ion channels |
|
|
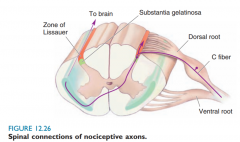
Nociceptors use which types of nerve fibre? |
- A delta and C |
|
|
Define hyperalgesia, primary and secondary hyperalgesia |
- hyperalgesia: sensitisation to pain after initial insult - primary hyperalgesia: hyperalgesia at the site of injury - secondary hyperalgesia: hyperalgesia in surrounding tissues due to the release of sensitising chemical adjacent |
|
|
What three factors might be responsible for hyperalgesia |
- reduced threshold - increase in stimuli - spontaneous pain |
|
|
Give examples of 3 substances which can cause sensitisation |
- bradykinin - prostaglandins - substance P - |
|
|
Regarding nociception, how do NSAIDs reduce pain? |
- inhibit prosatglandins - prostaglandins increase sensitivit of nociceptors |
|
|
Draw a diagram illustrating the differnce in speed at which pain is felt between A delta and C fibres |
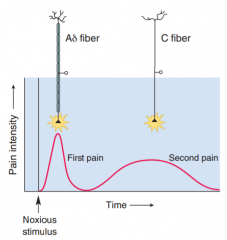
|
|
|
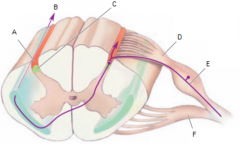
What is the zone called where A delat and C fibres travel up and down the spinal cord? |
Zone of Lissauer |
|
|
|
|
|
Whta is the neurotransmitter for pain afferents? What substance is likely required to experiencemoderate-intense pain |
- glutamate - substance P |
|
|
Define referred pain Give 2 examples of referred pain |
- occurs when there is crosstalk between and visceral and cutaneous stimui - angina and appendicitis |
|
|
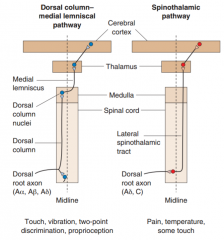
Draw diagram comparing the spinothalamic and dorsal column lemnisacl pathways |
|
|
|
What is the trigeminal pathway? |
- pain andtemperature pathway which travels from the face and head |
|
|
Describe the gate theory of pain |
- neurons in thedorsal horns – which project axons into up into the spinothalamictract – are excited by unmyelinated pain axons, and larger diametersensory axons. - The neuron which is involved in the projection isinhibited by a interneuron, which is excited by larger sensory axonsand inhibited by smaller pain axons. - As such, if the largemechanoreceptor axon fires at the same time, the inhibitoryinterneuron is activated – suppressing nociceptive signals up thespinothalamic pathway |
|
|
Regarding the modulation of pain, what is downward regulation |
- major zone isthe periqueductal grey matter (PAG) - sends signalsthrough descending axons to the raphe nuclei (serotonin), whichdepresses activity of noiceptive neurons in the dorsal horns |
|
|
Name 3 classes of endogenous opiate What are the 3 types of opiode receptor? |
- endorphins, enkephalins and dynorphins - mu (u), kappa (k)and delta |
|
|
What fibres are involved in perception of cold What fibres are involved in perception warmth |
- A delta and C - C |
|
|
What receptors are involved in perception of cold? What receptors are involved in perception of heat? |
- TRPM8 - TRPV1 |
|
|
List 5 non-modifiable risk factors of LBP |
- middle age - male gender - family/previoushistory - pregnancy - previouscompression fracture - surgery - congenital spineproblems |
|
|
List 5 modifiable risk factors of LBP |
- sedentarylifestyle - profession i.e.sitting, lifting, bending, twisting, repetitive motions, vibrations - smoking - obesity - poor posture - stress |
|
|
Desceibe the epidemiology of back pain |
- prevalence of49-70% (at least one episode over life) - ~85% of patientscan not be given a precise clinical diagnosis – no obviouspathology - acute LBP hasfavourable outcome, though recurrence within a year is common - imaging mayonly be indicated in patients with red flags. Generally imaging ispoor - classificationof types of back injury is poor – hindering progress - acute: <6weeks - subacute: 6weeks-3 months - chronic: >3months
- typical onset:30-50 - most commoncause of work-related injury- recovery acuteinjury is generally rapid (~70% recover in 2 weeks) |
|
|
List 6 red flags for LBP |
- onset either <20or >55 years - non-mechanicalpain i.e. not related to activity - thoracic pain - history ofcarcinoma, steriods or HIV - feeling unwell - weight loss - widespreadneurological symptoms - spinaldeformity |
|
|
List other significant indicators for PBP |
- saddleanaethesia - reduced analtone - hip/kneeweakness - generalneurological deficit - progressivespinal deformity - urinaryretention |
|
|
What is cauda equina? |
- extremepressure and swelling of the nerves at the end of the spinal cord |
|
|
List 6 symptoms of cauda equina |
- bilateralleg pain - back pain - urinaryretention - perianal sensoryloss - erectiledysfunction - reduced analtone |
|
|
What are the 3 most common causes of back injury |
- musculoligamentous injuries - age-related degenerative processes - spinal stenosis and disc herniation |
|
|
List 5 mechanical causes of spinal injury |
- trauma - musclular and liamentous pain - fibrostitic nodulosis - postular back pain - lumbar spondylosis - facet joint syndrome - spinal and root canal stenosis - spondyloliisthesis |
|
|
- List 3 metabolic causes of LBP |
- osteoporotic spinal fractures - osteomalacia - Paget's disease |
|
|
Define a disc prolapse |
- nucelus polposuscan herniate through the annulus fibrosis – disc prolapse.Typically occurs in cervical and lumbar (most common (load bearing))regions - generally occursposteriorly towards the interverterbal foramen and spinal nerves –poor support anteriorly and posteriorly by the ligaments |
|
|
Which spinal nerves are associated with sciatica? What is sciatica? |
- L4-S3 - painaffecting the back, hip, and outer side of the leg, caused bycompression of a spinal nerve root in the lower back, often owing todegeneration of an intervertebral disc. |
|
|
List 6 treatments for non-specific back pain |
- NSAIDs - muscle relaxants(side-effect: sedation) - spinalmanipulation and physical therapy for acute and subacute – benefitsthought to be limited - acupuncture –evidence for benefits is lacking - massage –lacks evidence but results are positive - for mostpatients, recommendation is to resume normal activities as quickly aspossible, with neither bed rest or absence of exercise during theacute phase – within limits - surgery islacking in evidence except for in sciatica, pseudoclaudication andspondylisthesis -Cognitivebehaviour therapy, supervised exercise therapy, brief educationalinterventions, and multidisciplinary (biopsychosocial) treatmen |
|
|
Describe thr role of the GP for back pain (5) |
- initial triageand referral to specialists as required - education,advice, reassurance, simple treatments, encouragement and support - support withwork-related issues - referral tosupportive care – e.g. physiotherapists and chiropractors - initial point ofcontact and coordination |
|
|
Describe the role of the physiotherapist for back pain (5) |
- improveassociated muscle strength - prevention andmanagement - based inhospitals or the community – health centres or patients own home - passivemodalities e.g. electrical stimulation - role is providepain relief and restore function > return to daily life |
|
|
Describe the role of the osteopath and chiropractor for back pain (5) |
- instantpain relief but no cure - principles ofchiropractor: disorders can be traced back to malalignment of bones,having an impact on nerves and muscles. Involves manipulation –typically of vertebrae - principles ofosteopathy: based on the theory that many systemic diseases relateback to the MSK system. Involves palpation, manipulation and massage - work with bones,muscles and connective tissue using hands to treat abnormalities ofstrucure and function – i.e. manual therapy - community andprivate sector |
|
|
Describe the psycho-social impact of chronic back pain |
-painis a highly subjective and personal experience and always has anemotional dimension that we need to appreciate -doctorsand therapists wrongly attribute pain as being either physical orpsychological -Mostlow back pain studies show that the main emotions experienced includeanxiety, increased bodily awareness and fear are helpful in an acuteinjury as a threat warning, however, these accompanied by depressionand anger are maladaptive in sub-acute and chronic pain -Theseemotions are heightened by their pain and disability and if left torun out of control, can aggravate and perpetuate the pain and anxietyexperienced by the patient and become part of the problem -the presence of such psychosocial factorsgreatly increases the risk of an acute episode of LBP developing intochronic LBP (CLBP) with a related high level of disability andincapacity - In a satisfactory consultation, goodrapport is established with the patient, and there is a satisfactoryoutcome, both clinically and occupationally. In a minority of cases,however, something appears to ‘go wrong’, resulting in adisaffected patient, a degree of frustration in the GP, and anoutcome that appears unsatisfactory on both sides - Some consultations are unsatisfactoryfrom a patient’s view because they are left feeling that the doctordoes not appear to understand their concerns or believe in theirsymptoms. It is known that there are common themes in patientanxieties and beliefs which, if not addressed, may lead to chronicdisability. The most frequently held beliefs include: • The wrong movement may cause aserious problem with my back • Avoiding movement is the safest wayto prevent back pain worsening • Something is dangerously wrong • I may be disabled for a long time • I can’t do normal things as it’stoo easy to be injured - As many as one in five patientsbelieve their back pain is due to serious disease. - It is known that telling patientsthat nothing is wrong or that they only have ‘minimal disease’can actually worsen their fears for the future – ‘If I’m in somuch pain now and I’ve only got mild, early disease, what will bethe pain be like when things progress?’ - Patients may become over-reliant onmedication, avoid all activity which they believe might be harmful,and adopt the sick role. - They may become over-reliant onothers and resistant to change.- the yellow and blue flags arefairly easily identifiable and potentially easily managed, but areoften not a specific focus of attention - Although an empathic approach isbest, it must not extend to collusion with the patient and failure tochallenge inappropriate sick behaviour. It is possible to contributeinadvertently to long-term sickness by arranging unnecessaryinvestigations and referrals, or issuing prolonged sick notes. - It is important to begin with thepatient’s account of their problem, and demonstrate that they arebeing listened to. This will often provide helpful cues of areas toexplore. Ultimately, however, it is necessary to focus specificallyon the patient’s beliefs about back pain and the impact on theirfunction, well-being and work. Mistaken beliefs, inaccurateinformation or ‘catastrophising’ attitudes should be respectfullybut firmly challenged and restructured. - It is important to check the patientunderstands the explanation and advice. Although not all GPs areconvinced of the value of educational materials, back-up with writteninformation such as the Back Book 6 can be helpful. - In addition to the provision ofinformation and re-shaping of expectations, it is important torecognise and incorporate the emotional needs of the patient. Makesure that any reassurance is tailored to meet the patient’sunderstanding and health anxiety levels, which may have beeninfluenced significantly by previous experience of illness, forexample, in their family.7 It is often necessary to reduce theirfears for the future by contrasting their situation with that oftheir relatives. |
|
|
Whatare the blue an yellow flags for back pain? |
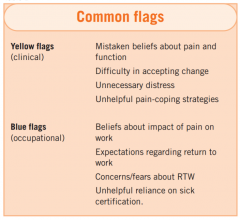
|

