![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
138 Cards in this Set
- Front
- Back
|
ATP METABOLISM
- Aerobic pathway shuttle pathways - how much ATP is made for each? |
Malate-Aspartate shuttle (32 ATP)
Glycerol-3-Phosphate shuttle (30 ATP) |
|
|
ATP METABOLISM
- Malate-Aspartate shuttle utilized where? - Glycerol-3-Phosphate shuttle utilized where? |
- Heart
- Liver - Muscle |
|
|
ATP METABOLISM
- Anaerobic metabolism of glucose produces how many ATPs? |
- 2 ATP
|
|
|
NADPH
- is a product of what pathway? |
- HMP shunt
|
|
|
NADPH
- used in what/where? x5 |
(NADPH GRAPE)
- Glutathione Reductase - Respiratory Burst - Anabolic processes - P450 - Electron ACCEPTOR (universal) |
|
|
NAD+ is used in what processes?
|
- Catabolic
|
|
|
NADPH is used in what processes?
|
- Anabolic
(the "A" of GRAPE) |
|
|
GLUCOKINASE vs. HEXOKINASE
- Glucokinase is where? - Hexokinae is where? |
- Beta cells of Pancreas
- Liver cells - Ubiquitous - Everywhere |
|
|
GLUCOKINASE vs. HEXOKINASE
- which has high Km ? - which has high Vmax? |
- Glucokinase
- Glucokinase |
|
|
GLUCOKINASE vs. HEXOKINASE
- which has high Affinity? - which as high Capacity? |
- Hexokinase
- Glucokinase |
|
|
GLUCOKINASE vs. HEXOKINASE
- which one is INSULIN-INDUCED? |
- Glucokinase
|
|
|
GLUCOKINASE vs. HEXOKINASE
- these 2 enzymes do what same function? |
1st Step of Glycolysis
(Phosphorylation of Glucose to yield Glucose-6-Phosphate) |
|
|
Phosphorylation of Glucose
to yield Glucose-6-Phosphate is the 1st step of what process(es)? (Glucose + ATP ==> G6P) |
- Glycolysis
- Glycogen Synthesis (in the Liver) |
|
|
GLUCOKINASE vs. HEXOKINASE
- Direct Feedback Inhibition of Glucokinase? |
- none
|
|
|
GLUCOKINASE vs. HEXOKINASE
- Direct Feedback Inhibition of Hexokinase? |
- Glucose-6-Phosphate
|
|
|
Glucose phosphorylation by which enzyme occurs immediately AFTER MEALS?
- Where? - Why? - What does this allow for? |
- Glucokinase
- Liver - Phosphorylation traps glucose in Liver - Allows Liver to serve as a BLOOD GLUCOSE BUFFER |
|
|
GLYCOLYSIS
- Glycolysis net reaction equation |
Glucose + Pi + ADP + NAD+
==> 2 pyruvate + 2 ATP + 2 NADH + 2H2O + 2H+ |
|
|
GLYCOLYSIS
- List the reactions that require ATP including the enzyme involved. |
Step 1: Glucokinase/Hexokinase
Glucose ==> Glucose-6-Phosphate Step 3: PFK-1 (rate-limiting step) F6P ==> F1,6-BP |
|
|
GLYCOLYSIS
- List the reactions that generate ATP including the enzyme involved. |
Step 7: PG Kinase
1,3-BPG ==> 3-PG Step 9: Pyruvate Kinase PEP ==> Pyruvate |
|
|
GLUCOKINASE/HEXOKINASE
- what are the inhibitor(s) - what are the stimulator(s) |
- G6P inhibits Hexokinase
(does NOT inhibits Glucokinase) - none |
|
|
PFK - 1
- what are the inhibitor(s) - what are the stimulator(s) |
- Citrate
- ATP - Fructose-2,6-BP - AMP |
|
|
PYRUVATE KINASE
- what are the inhibitor(s) - what are the stimulator(s) |
- Alanine
- ATP - Fructose-1,6-BP |
|
|
PYRUVATE DEHYDROGENASE
- what are the inhibitor(s) - what are the stimulator(s) |
- Acetyl-CoA
- NADH - ATP - none |
|
|
FRUCTOSE BISPHOSPHATASE 2
- active in which state? |
- Fasting state
|
|
|
PHOSPHOFRUCTOKINASE 2
- active in which state? |
- Fed state
|
|
|
FRUCTOSE BISPHOSPHATASE 2
- FBP-2 enzyme does what reaction? |
Fructose-2,6-BP ==> Fructose-6-P
|
|
|
PHOSPHOFRUCTOKINASE 2
- PFK-2 enzyme does what reaction? (what reaction done by PFK-1) |
Fructose-6-P ==> Fructose-2,6-BP
(F6P ==> F-1,6-BP) |
|
|
FASTING STATE vs. FEEDING STATE
- which state experiences increased Glucagon? - Glucagon has what effect to intracellular secondary messengers? |
- Fasting state
- Increases cAMP |
|
|
FASTING STATE vs. FEEDING STATE
- which state experiences increased Insulin? - Insulin has what effect to intracellular secondary messengers |
- Feeding state
- Decreases cAMP |
|
|
FASTING STATE
- hormone effect - secondary messenger effect - enzymatic effect - effect on FBPase-2 - effect on PFK-2 |
- increased Glucagon
- increases cAMP - increases Protein Kinase A - increases FBPase-2 activity - decreases PFK-2 activity |
|
|
FEEDING STATE
- hormone effect - secondary messenger effect - enzymatic effect - effect on FBPase-2 - effect on PFK-2 |
- increases Insulin
- decreases cAMP - decreases Protein Kinase A - decreases FBPase-2 activity - increases PFK-2 activity |
|
|
Fructose-2,6-Bisphosphate
- is a positive feed-forward stimulator of? |
PFK-1
(rate limiting enzyme for glycolysis) |
|
|
PFK-2
- drives what pathway? |
- Glycolysis
(b/c in fed state) |
|
|
FBPase-2
- drives what pathway? |
- Gluconeogenesis
(b/c in fasting state) |
|
|
Fructose-1,6-BisPhosphate stimulates what enzyme?
Fructose-2,6-BisPhosphate stimulates what enzyme? |
- Pyruvate Kinase
- PFK-1 |
|
|
PYRUVATE DEHYDROGENASE COMPLEX
- Reaction equation |
Pyruvate + CoA + NAD
==> Acetyl-CoA + CO2 + NADH |
|
|
PYRUVATE DEHYDROGENASE COMPLEX
- how does exercise effect it? - exercise effects via what changes? x3 |
- Activates Pyruvate DHase
Increases: - Ca2+ - ADP - NAD+/NADH ratio |
|
|
Alcohol metabolsim effects on Niacin based ratio.
Exercise effects on Niacin based ratio. |
Increases NADH/NAD+ ratio
Increases NAD+/NADH ratio |
|
|
PYRUVATE DEHYDROGENASE COMPLEX
- effects of Arsenic on Pyruvate DHase - how so? |
- inhibits Pyruvate DHase
- by inhibiting cofactor Lipoic Acid (B4) |
|
|
PYRUVATE DEHYDROGENASE COMPLEX
- Arsenic poisoning symptoms |
Garlic breath
Vomiting Rice-water stools |
|
|
PYRUVATE DHase DEFICIENCY
- Acquired or Congenital? |
- Both
|
|
|
PYRUVATE DHase DEFICIENCY
- Acquired PyrDHase Deficiency seen in what population groups? - why? |
- Alcoholics
- causes B1 deficiency (TPP is a cofactor of PyrDHase) |
|
|
PYRUVATE DHase DEFICIENCY
- causes backup of what substrate? - substrate backup leads to what condition? - symptoms? |
- Pyruvate
- Alanine - Lactic Acidosis - Neurologic defects |
|
|
PYRUVATE DHase DEFICIENCY
- Treatment? - give examples of treatment? |
- Increase intake of Ketogenic nutrients
(so you have less glucogenic AA) - High Fat content diet - Diet high in Leucine & Lycine |
|
|
List the only 2 pure Ketogenic amino acids.
|
Leucine & Lycine
|
|
|
Products of Pyruvate
- that goes to the Cytosol - include the enzymes responsible |
- Lactate (Lactate DHase)
- Alanine (ALT) |
|
|
Products of Pyruvate
- that goes to the Mitochondria - include the enzymes responsible |
- Oxaloacetate (Pyr. Carboxylase)
- Acetyl-CoA (Pyruvate DHase) |
|
|
Products of Pyruvate
- which product requires ATP (& CO2)? |
- OxaloAcetate
|
|
|
Products of Pyruvate
- which product requires NAD+? |
- Acetyl-CoA
|
|
|
Products of Pyruvate
- which product requires B1? |
- Acetyl-CoA
(b/c Pyr. DHase requires TPP) |
|
|
Products of Pyruvate
- which product requires NADH? |
- Lactic acid
|
|
|
Products of Pyruvate
- Alanine function? |
- carries NH3 to the Liver
(from Muscle) |
|
|
Products of Pyruvate
- Oxaloacetate function? |
- Replenishes TCA
- used for Gluconeogenesis |
|
|
Products of Pyruvate
- Acetyl-CoA function? |
- Transitions to TCA
|
|
|
Products of Pyruvate
- Lactic acid function? |
- End product of Anaerobic glycolysis
|
|
|
Products of Pyruvate
- Anaerobic glycolysis is the major pathway for what cells? |
- RBC
- WBC - Renal MEDULLA - Testes - Lens - Cornea |
|
|
TCA cycle
- produces what side products? |
1 GTP
1 FADH2 2 CO2 3 NADH |
|
|
TCA cycle
- produces how much ATP per Acetyl-CoA - produces how much ATP per Glucose |
- 12 ATP
- 24 ATP |
|
|
TCA cycle
- Pyruvate DHase Inhibitors - Pyruvate DHase Stimulators |
- ATP
- NADH - Acetyl-CoA - none |
|
|
TCA cycle
- Citrate Synthase Inhibitors - Citrate Synthase Stimulators |
- ATP
- none |
|
|
TCA cycle
- Isocitrate DHase Inhibitors - Isocitrate DHase Stimulators |
- ATP
- NADH - ADP |
|
|
TCA cycle
- Alpha Ketoglutarate DHase Inhibitors - Alpha Ketoglutarate DHase Stimulators |
- ATP
- NADH - Succinyl-CoA - none |
|
|
TCA cycle
- what reaction forms GTP? |
Succinyl-CoA ==> Succinate
|
|
|
TCA cycle
- what reaction forms FADH2? |
Succinate ==> FORMATE
|
|
|
TCA cycle
- what reaction forms NADH? |
Isocitrate ==> Alpha-ketoglutarate
Alpha-ketoglutarate ==> Succinyl-CoA Malate ==> Oxaloacetate |
|
|
Pyruvate (via Pyr. DHase) forms Acetyl-CoA along with what other products?
|
1 NADH
1 CO2 |
|
|
TCA cycle
- which TCA cycle enzyme is Complex II of the ETC? |
- Succinate DHase
|
|
|
TCA cycle
- NADH electrons from Glycolysis & TCA enter ______ via _________ and ________ |
- Mitochondria
- Malate-Aspartate shuttle - Glycerol-6-Phosphate shuttle |
|
|
TCA cycle
- FADH2 electrons from TCA are transferred to which ETC complex? |
- Complex II
|
|
|
ETC & Ox Phos
- Protons enter the Mitochondrial Matrix via what complex? |
Complex V
(ATP synthase) |
|
|
ETC & Ox Phos
- Protons enter the Intermembranous space via what complex? |
Complex I, III, & IV
|
|
|
GLUCONEOGENESIS
- what are the IRREVERSIBLE enzymes? |
(Pathway Producing Fresh Glucose)
- Pyruvate Carboxylase - PEP Carboxykinase - Fructose-1,6-Bisphosphatase - Glucose-6-Phosphate |
|
|
GLUCONEOGENESIS
- which irreversible enzyme is in the mitochondria? - which is in the cytosol? - which is in the ER? |
- Pyruvate Carboxylase
- PEP Carboxykinase - Fructose-1,6-Bisphosphatase - Glucose-6-Phosphate |
|
|
GLUCONEOGENESIS
- which enzyme requires ATP? - which enzyme requires GTP? |
- Pyruvate Carboxylase
(also requires Biotin) - PEP Carboxykinase |
|
|
GLUCONEOGENESIS
- which enzyme requires Acetyl-CoA to become activated? |
- Pyruvate Carboxylase
|
|
|
GLUCONEOGENESIS
- occurs primarily where? - deficiency causes what plasma changes? |
- Liver
- Hypoglycemia |
|
|
GLUCONEOGENESIS
- what tissues can NOT participate in Gluconeogenesis? - why? |
- Muscle tissue
- lacks Glucose-6-Phosphatase |
|
|
GLUCONEOGENESIS
- which fatty acids can NOT participate in Gluconeogenesis? - why? |
- Even-chain FA
- b/c they yield only Acetyl-CoA equivalents |
|
|
GLUCONEOGENESIS
- Odd-chain FA yields what during metabolism? - these can enter what pathway? - enters pathway as what? |
- Propionyl-CoA
- TCA - as Succinyl-CoA (then undergo gluconeogenesis) |
|
|
HMP SHUNT
- NADPH comes from what intermediate? |
- G6P
|
|
|
HMP SHUNT
- besides NADPH, this HMP also provides what compound? - above compound is useful for? |
- Ribose
- Nucleotide synthesis - Glycolysis intermediates |
|
|
HMP SHUNT
- how much ATP is produced? - how much ATP is used up? |
- none
- none |
|
|
HMP SHUNT
- occurs where? x4 |
- RBC
- Adrenal Cortex - Liver - Lactating mammary glands |
|
|
HMP SHUNT
- Rate limiting enzyme? |
- G6PDHase
|
|
|
HMP SHUNT
- Oxidative phase enzyme? - Oxidative phase substrate? - Oxidative phase products? |
- G6PDHase
- G6P - 2 NADPH - Ribulose - CO2 |
|
|
HMP SHUNT
- Non-oxidative phase enzyme? - Non-oxidative substrate? - Non-oxidative products? |
- Transketolase (B1 cofactor)
- Ribulose - G3P - F6P - Ribose-5-P |
|
|
HMP SHUNT
- which phase is irreversible? |
- Oxidative phase
|
|
|
RESPIRATORY BURST
- involves the activation of what enzyme? - enzyme located where? |
- NADPH Oxidase
- Membrane surface of RBC |
|
|
RESPIRATORY BURST
- results in the rapid release of what? |
Reactive Oxygen Intermediates (ROIs)
|
|
|
RESPIRATORY BURST
- NADPH Oxidase deficiency is called what? |
- Chronic Granulomatous Disease (CGD)
|
|
|
Patients with CGD are at increased risk for infection by what TYPE of species?
- give examples - why are these species so effective in infecting CGD patients? |
- Catalase Positive
- Staph. Aureus - Aspergillus - Catalase positive species can neutralize their own H2O2, thus WBCs cannot make ROIs to fight infection |
|
|
G6PDHase Deficiency
- NADPH is necessary to keep Glutathione _____, because it will detoxify ______ & _________. |
- Reduced
- Free Radicals - Peroxides |
|
|
G6PDHase Deficiency
- Decreased NADPH in RBCs lead to what type of anemia? - this is due to poor RBC defense against what agents? - list some of these agents |
- Hemolytic anemia
- Oxidizing agents - Fava beans - MTX - INH - Sulfonamides - TB-drugs |
|
|
G6PDHase Deficiency
- inheritance pattern? - more commonly seen in what population group? - diseased patients have a unique resistance to what other disease? |
- XLR
- Blacks - Malaria |
|
|
G6PDHase Deficiency
- what type of cells do you see on blood smears? - what causes their morphology? |
Heinz Bodies
- oxidized Hb precipitated on RBC Bite Cells - "bite" removed from phagocytic removal of Heinz bodies by macrophages |
|
|
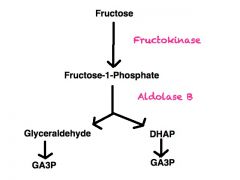
Essential Fructosuria
- etiology? - inheritance pattern? - Sx? |
- Fructokinase defect
- AR - mild symptoms with Fructose found in blood & urine |
|
|
Fructose Intolerance
- etiology - inheritance pattern? |
- Aldolase B deficiency
- AR |
|
|
Fructose Intolerance
- what substrate accumulates? - thus cause what electrolyte change? - thus leading to what effects on pathways? |
- Fructose-1-Phosphate
- Decrease in Phosphate Inhibition of: - Gluconeogenesis - Glycogenolysis |
|
|
Fructose Intolerance
- Sx x4 |
- Hypoglycemia
- Jaundice - Cirrhosis - Vomiting |
|
|
Fructose Intolerance
- Tx? |
Decrease intake of:
- Fructose - Sucrose (note Sucrose = Glucose + Fructose) |
|
|
Fructose is not glucose.
Fructose metabolism bypass the glycolytic pathway by bypassing with glycolytic step? via what enzyme? |
- Rate limiting step involving PFK-1
- aldolase B |
|
|
|
|
|
|
|
|
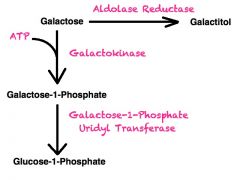
Galactokinase Deficiency results in accumulation of ________ , but only if __________ .
This occurs due to the alternative pathway involving what enzyme? |
- Galactitol
- Galactose is in the diet - Aldol Reductase |
|
|
Galactokinase Deficiency
- what changes are found in plasma? - what changes are found in urine? |
- Increased Galactose
(increased galactitol if galactose in diet) - Increased Galactose |
|
|
Galactokinase Deficiency
- most notable symptom in infants - may initially present as infant failure to do what? |
- Infantile Cataracts
- Failure to track objects - Failure to develop Social Smile |
|
|
Classic Galactosemia
- etiology? - damage is caused by accumulation of toxic substances including ____ which accumulates in _________. |
- Galactose-1-Phosphate Uridyl Transferase
- Galactitol - Lens of the eye |
|
|
Classic Galactosemia
- symptoms |
- Infantile cataracts
- MR - Jaundice - Hepatosplenomegaly - FTT |
|
|
Classic Galactosemia
- Tx |
EXCLUDE
- Galactose - Lactose Note: Lactose = Galactose + Glucose |
|
|
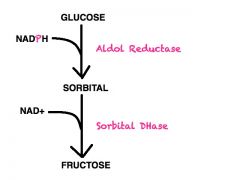
Alternative method of trapping glucose in the cell is to covert it to?
Occurs via what enzyme? |
- Sorbital
(alcohol counterpart) - Aldol Reductase |
|
|
Some cells can convert Sorbital to ______, using the enzyme __________.
|
- Fructose
- Sorbitol DHase |
|
|
ALDOL REDUCTASE
- converts what reaction? - requires what cofactor? |
Glucose ==> Sorbitol
NADPH |
|
|
ALDOL REDUCTASE
- what cells only have this enzyme, but lack Sorbital DHase? |
- Schwann cells
- Kidney cells - Retina - Lens |
|
|
SORBITAL DEHYDROGENASE
- converts what reaction? - requires what cofactor? |
Sorbital ==> Fructose
NAD+ |
|
|
SORBITAL DEHYDROGENASE
- cells lacking this enzyme are at risk for INTRACELLULAR accumulation of? - what TYPE of Damage is seen? - give examples of symptoms that can arise? |
- Sorbital
- Osmotic damage - Cataracts - Retinopathy - Peripheral Neuropathy (Sx seen in chronic hyperglycemia of DM patients) |
|
|
|
|
|
What are the Essential Amino Acids?
(x10) |
(PVT TIM HALL)
- Phenylalanine - Valine - Threonine - Tryptophan - Isoleucine - Methionine - Histidine - Alanine - Lycine - Leucine |
|
|
Which Essential Amino acids are purely Ketogenic? (x2)
Which Essential Amino acids are both Ketogenic & Glucogenic? (x4) Which Essential Amino acids are purely Glucogenic? (x4) |
- Lysine & Leucine
(PITT) - Phenylalanine - Isoleucine - Threonine - Tryptophan - Histidine - Alanine - Methionine - Valine |
|
|
- Which amino acids are Acidic?
- Which amino acid is negatively charged at body pH) |
- Aspartate (Aspartic acid)
- Glutamate (Glutamic acid) - Glutamate |
|
|
- Which amino acids are Basic?
- Which amino acid is most basic? - Which amino acid has no charge at body pH? |
- Lysine
- Arginine - Histidine - Arginine - Histidine |
|
|
Which amino acids are required during periods of growth?
|
- Histidine
- Arginine |
|
|
Which amino acid is NEGATIVELY CHARGED at body pH?
|
- Glutamate
|
|
|
Which amino acid is NEUTRAL at body pH?
|
- Histidine
|
|
|
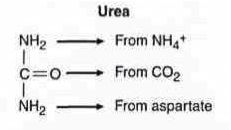
UREA CYCLE
- rate-limiting step reaction? - rate-limiting enzyme? - additionally required reactants? - occurs in what organelle? - occurs in what cell? |
NH4 + CO2 ==> Carbomoyl Phosphate
Carbamoyl Phosphate Synthetase I 2 ATP Mitochondria Liver |
|
|
UREA CYCLE
- what compound leaves the liver mitochondria and goes to the liver cytoplasm? |
- Citrulline
|
|
|
UREA CYCLE
- what compound leaves the liver cytoplasm and goes into the liver mitochondria? |
- Ornithine
|
|
|
UREA CYCLE
- what intermediate leaves the mitochondria? - what is the reaction that forms it? - what is the enzyme involved? |
- Citrulline
Carbamoyl-P + Ornithine ==> Citrulline - Ornithine Transcarbamoylase |
|
|
UREA CYCLE
- excess nitrogen (NH4+) is finally converted into what? - which then goes where? - for what? |
- Urea
- Kidney - Excretion |
|
|
AMMONIUM
- Ammonia (NH3) from muscle comes from what? - Ammonia (NH3) from muscle is transported to what organ? - Ammonia (NH3) from muscle is transported in blood via what intermediate? |
- Amino acids
- Liver - Alanine |
|
|
AMMONIUM
- Ammonium (NH3) from muscle is transported to the Liver as what intermediate? - In the Liver, the Ammonium (NH3) is finally incorporated into what chemical compound? |
- Alanine
- Urea |
|
|
HYPERAMMONEMIA
- excess NH4+ causes depletion of what intermediate? - this leads to inhibition of what pathway? |
- Alpha-Ketoglutarate
- TCA |
|
|
HYPERAMMONEMIA
- Ammonia intoxication causes what symptoms. |
- Blurry vision
- Cerebral edema - Tremor - Vomiting - Slurring speech - Somnelence |
|
|
HYPERAMMONEMIA
- First Tx option? - In order to decrease Ammonia levels, what medications can be given? |
- Limit Protein in Diet
- Benzoic acid - Phenylbutyrate |
|
|
OTC DEFICIENCY
- inheritance pattern - excess intermediate? - excess intermediate is converted into what? |
- XLR
- Carbamoyl Phosphate - Orotic acid (part of pyrimidine synthesis pathway) |
|
|
OTC DEFICIENCY
- what is elevated in blood? - what is decreased in blood? |
- Orotic acid
(also in urine) - BUN |
|
|
OTC DEFICIENCY
- what are the symptoms of OTC Deficiency? |
Symptoms of Hyperammonemia
- Blurry vision - Cerebral edema - Tremors - Vomiting - Slurring speech - Somnelence |
|
|
OTC DEFICIENCY
- interferes with the body's ability to do what? |
- eliminate ammonia
|
|
|
|

