![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
145 Cards in this Set
- Front
- Back
|
FAT SOLUBLE VITAMINS
- absorption dependent on what parts of the body? |
- ileum
- pancreas |
|
|
Malabsorption syndromes (steatorrhea) than can cause Fat Soluble vitamin deficiencies. x2
Intake of what can cause Fat Soluble Vitamin deficiencies? x1 |
- Cystic Fibrosis
- Celiac Sprue - Mineral Oil |
|
|
WATER SOLUBLE VITAMINS
- all wash out easily from body except? |
- B12
- Folate (stored in liver) |
|
|
WATER SOLUBLE VITAMINS
- what is B1? - what is B2? - what is B3? |
- Thiamine
- Riboflavin - Niacin |
|
|
WATER SOLUBLE VITAMINS
- what is B4? - what is B5? - what is B6? |
- Lipoic acid
- Pantethenoic acid - Pyridoxine |
|
|
WATER SOLUBLE VITAMINS
- what is B9? - what is B12? |
- Folate
- Cyanocobalamin |
|
|
WATER SOLUBLE VITAMINS
- besides the B-complex vitamins, list additional water soluble vitamins. |
- Vitamin C
- Biotin |
|
|
WATER SOLUBLE VITAMINS
- B-complex vitamin deficiencies often result in what 3 general symptoms? |
- Skin: Dermatitis
- Tongue: Glossitis - Diarrhea |
|
|
WATER SOLUBLE VITAMINS
- what is Vitamin B1? - acts as a cofactor for what enzymes? |
- Thiamine (TPP)
- Pyruvate DHase - Alpha-Ketoglutarate DHase - Branched Chain AA DHase - Transketolase |
|
|
- Vitamin B1 deficiency effects Glucose in what way?
- This impairment results in? - Wrongly administering what could worsen the scenario? - What tissues are affected first? |
- Glucose Breakdown impairment
- ATP depletion - Glucose infusion (can worsen above) - Brain & Heart (these are highly aerobic tissues) |
|
|
WATER SOLUBLE VITAMINS
- B1 deficiency can cause what 2 conditions? - what type of patients are susceptible to B1 Deficiency Dz |
- Ber1 Ber1
- Wernicke-Korsakoff - Malnutrition patients - Alcoholic patients (secondary to malnutrition & malabsorption) |
|
|
DRY BERI BERI
- seen with what vitamin deficiency? - Dry Beri Beri symptoms? |
- B12
- Polyneuritis - Symmetrical Muscle Wasting |
|
|
WET BERI BERI
- seen with what vitamin deficiency? - Wet Beri Beri symptoms? |
- B12
- High Output Cardiac Failure (dilated cardiomyopathy) - Edema |
|
|
WERNICKE-KORSAKOFF
- seen with what vitamin deficiency? - most important symptoms seen - are the symptoms reversible? |
- B12
- Confabulation - Personality change - Memory loss (permanent) |
|
|
WERNICKE-KORSAKOFF
- lesion is seen where? |
- Medial Dorsal Nucleus (Thalamus)
- Mammillary bodies (Hypothalamus) (possibly in Periaqueductal Gray area) |
|
|
Wernicke-Korsakoff is a progression of what prior, preexisting disease?
Give the Triad symptoms associated. |
- Wernicke's Encephalopathy
- Confusion - Ophthalmoplegia - Ataxia |
|
|
Wernicke's Aphasia
- what type of aphasia is this? - describe speech - describe comprehension - describe repetition ability |
- Receptive (sensory) aphasia
- Fluent (word salad) - Poor - Poor |
|
|
Wernicke's Aphasia
- Lesion location? |
- Superior Temporal Gyrus
(or Posterior Temporal Lobe) |
|
|
WATER SOLUBLE VITAMINS
- What is B2? - Important B2 derivative? - Why important? |
- Riboflavin
- FAD (....FADH2 and FMN) - Cofactors for Oxidation/Reduction reactions |
|
|
WATER SOLUBLE VITAMINS
- Riboflavin is what? - what breaks it down? |
- B2
- sunlight (thats why no more milkman with glass milk jugs b/c milk is best source for B2) |
|
|
WATER SOLUBLE VITAMINS
- FAD is derived from what vitamin? - FAD provides how much ATP? |
- B2
- 2 |
|
|
WATER SOLUBLE VITAMINS
- B2 deficiency causes what conditions? |
- Cheliosis
- Corneal vascularization |
|
|
WATER SOLUBLE VITAMINS
- B3 is what? - Important B3 derivatives? - Why important? |
- Niacin
- NADH - NADPH - Cofactors for Oxidation/Reduction reactions |
|
|
WATER SOLUBLE VITAMINS
- B3 cofactors are required by what enzymes? |
- Pyruvated DHase
- Alpha-Ketoglutarate DHase - Branched Chain AA DHase |
|
|
Niacin is from vitamin _____ .
Niacin can also be converted from ________ , but that requires the cofactor _______. |
- B3
- Tryptophan - B6 (PP) |
|
|
WATER SOLUBLE VITAMINS
- B3 deficiency can lead to what condition? - What are the Triad of symptoms? |
- Pellegra
(the 3 D's) - Dementia - Diarrhea - Dermatitis |
|
|
PELLEGRA
- caused by deficiency of? - can also be caused by what 2 other conditions (and describe why)? |
- Vitamin B3
- Hartnup's disease (decreased Trp absorption) - Malignant Carcinoid Syndrome (increased Trp metabolism) |
|
|
PELLEGRA
- use of what drug can cause Pellegra? - explain how? |
- Isoniazid (INH)
- INH induces B6 deficiency. B6 is a needed cofactor for the conversion of Trp to Niacin. |
|
|
WATER SOLUBLE VITAMINS
- Niacin is used in pharmacological doses to treat what? - side effects? |
- Hyperlipidemia
- Facial flushing |
|
|
WATER SOLUBLE VITAMINS
- what is B4? - what enzymes require it? |
- Lipoic acid
- Pyruvate DHase - Alpha Ketoglutarate DHase - Branched chain AA DHase |
|
|
WATER SOLUBLE VITAMINS
- Lipoic acid is what vitamin? - What inhibits Lipoic acid? |
- B4
- ARSENIC !!!!!!! |
|
|
TRYPTOPHAN
- this amino acid what kind of charge? - can be converted into what important products? |
- Neutral charge
(MSN) - Melatonin - Serotonin - Niacin (req. B6/PP) |
|
|
WATER SOLUBLE VITAMINS
- B5 is what? - is an essential component of what? |
(think 5 = "penta" "A"cid w/ Co"A")
- Pantothenoic acid - CoA |
|
|
WATER SOLUBLE VITAMINS
- Pantothenoic acid is what vitamin? - Pantothenoic acid is an essential part of what cofactor? - Above cofactor is required in reactions of what enzymes? |
- B5
- CoA - Pyruvate DHase - Alpha Ketoglutarate - Branched Chain AA DHase |
|
|
WATER SOLUBLE VITAMINS
- which vitamins are necessary for a group of important DHase enzymes? - list the DHase enzymes |
B1 to B5
Pyruvate DHase Alpha Ketoglutarate DHase Branched Chain AA DHase |
|
|
WATER SOLUBLE VITAMINS
- What is B6? - What is an important B6 derivative? |
- Pyridoxine
- Pyridoxine Phosphate (PP) |
|
|
Pyridoxine Phosphate (PP)
- comes from what vitamin? - PP is a required cofactor for? |
- B6
(my 6" PP = Nice Hemi Trans-am for the DG Sista's) - Niacin synthesis - Heme synthesis - Transaminases (all of them) - Decarboxylase (all of them) - Glycogen phosphorylase - Cystathione synthesis |
|
|
WATER SOLUBLE VITAMINS
- Vitamin cofactor required for all Tranaminase enzymes? |
- B6
(PP) |
|
|
WATER SOLUBLE VITAMINS
- Vitamin cofactor required for all Decarboxylase enzymes? |
- B6
(PP) |
|
|
GLYCOGENOLYSIS
- what is the rate limiting enzyme? - enzyme requires what cofactor? - cofactor comes from what vitamin? |
- Glycogen Phosphorylase
- Pyridoxine Phosphate (PP) - Vitamin B6 |
|
|
WATER SOLUBLE VITAMINS
- B6 is what? - B6 deficiency resulting in what signs and symptoms? x2 |
- Pyridoxine (PP)
- Sideroblastic Anemia - Peripheral Neuropathy (also ==> irritability & convulsions) |
|
|
WATER SOLUBLE VITAMINS
- B6 deficiency can also be caused by what medications? |
- INH
- some Oral Contraceptives |
|
|
TRANSKETOLASE
- important enzyme for what pathway? - requires what cofactor? - cofactor comes from what vitamin |
- HMP shunt
- Thiamine - B1 |
|
|
WATER SOLUBLE VITAMINS
- B9 is what? - Converted into what important cofactor? - Cofactor important for what reactions? |
- Folic acid
- THF - 1-carbon Transfer reactions (aka - Methylation reactions) |
|
|
TETRAHYDROFOLATE
- comes from what vitamin? - cofactor for what reactions? - important for synthesis of what? |
- B9
- 1C Transfer reactions (aka - Methylation reactions) - Nitrogenous Bases (nucleotide) synthesis (for DNA & RNA) |
|
|
What is the first vitamin to run out whenever you have rapidly dividing cells?
|
- B9 (Folic acid)
|
|
|
WATER SOLUBLE VITAMINS
- Folic acid comes from what vitamin? - Folic acid deficiency results in what signs and symptoms? x2 |
- B9
- Macrocytic, Megaoblastic Anemia - Neural Tube Defects |
|
|
WATER SOLUBLE VITAMINS
- Folic Acid Deficiency seen in what patients? - Folic Acid Deficiency can occur with what medications? |
- Alcoholics
- Pregnant patients - Phenytoin - MTX - Sulfonamides |
|
|
WATER SOLUBLE VITAMINS
- A small reserve pool of folate can be stored primarily where? - Folate can be found in what foods? |
- Liver
- Green, Leafy vegetables (don't overcook) |
|
|
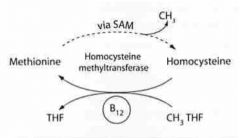
WATER SOLUBLE VITAMINS
- what is B12? - B12 derivative? - B12 derivative is important for what enzymes? |
- Cyanocobalamin
- Cobalamin - Homocysteine Methyltransferase - Methylmalonyl-CoA Mutase |
|
|
WATER SOLUBLE VITAMINS
- What are the 2 reactions requiring B12? |
Homocysteine + N-MTHF ==(B12)==> Methionine + THF
Methylmalonyl-CoA ==(B12)==> Succinyl-CoA |
|
|
WATER SOLUBLE VITAMINS
- Cobalamin cofactor comes from? - Cobalamin cofactor needed to make? - Cobalamin cofactor needed to recycle? |
- B12 (cyanocobalamin)
- THF - Odd-numbered carbon Fatty Acids |
|
|
WATER SOLUBLE VITAMINS
- B12 is needed to recycle what? - why is this important? |
- Odd-numbered carbon Fatty acids
- required for Myelin production |
|
|
WATER SOLUBLE VITAMINS
- B12 is found in what foods? - B12 is synthesized by? - B12 has a large reserve pool in? |
- Animal products
- Microorganisms ONLY. - Liver |
|
|
WATER SOLUBLE VITAMINS
- B12 deficiency causes what signs and symptoms? x2 |
- Macrocytic, Megaloblastic anemia
- Neuropathy (parethesia & SCD) |
|
|
WATER SOLUBLE VITAMINS
- B12 Deficiency causes neurologic symptoms due to abnormal ______ . |
Myelin
|
|
|
WATER SOLUBLE VITAMINS
- Malabsorption induced B12 deficiency can be caused by what 2 conditions? - can also be caused by what organism? |
(CGD)
- Celiac Sprue - Gastroenteritis - Diphyllobothrium latum |
|
|
WATER SOLUBLE VITAMINS
- B12 Deficiency can also be caused by a lack of what important protein? - what conditions would cause the lack of the above protein? |
- Intrinsic Factor
- Gastric Bypass Surgery - Pernicious anemia (Gastritis A) |
|
|
WATER SOLUBLE VITAMINS
- B12 Deficiency can also be caused by the absence of what anatomical structure? - what conditions would cause the absence of the above anatomical structure? |
- Terminal Ileum
- Crohn's Dz |
|
|
SUBACUTE COMBINED DEGENERATION
- is caused by what deficiency? - refers to degeneration of what? x2 - degeneration occurs due to loss of what tissue? |
- B12 deficiency
- DCML - Lateral Corticospinal Tracts - Myelin |
|
|
SUBACUTE COMBINED DEGENERATION
- usually accompanied by what type of anemia? |
- Pernicious anemia
|
|
|
PERNICIOUS ANEMIA
- is a subclass of what? - is caused by what Dz? - Dz causes what effect on what cells? - Cell effects lead to what? |
- Megaloblastic anemia
- Gastritis Type A (Autoimmune) - Atrophic loss of Parietal Cells - Leads to loss of Intrinsic Factor |
|
|
PERNICIOUS ANEMIA
- must include what 3 things in the etiology? - causes what vitamin disorder? |
- caused by Gastritis Type A (Autoimmune)
- Loss of gastric Parietal cells - Loss of Intrinsic Factor - causes Vitamin B12 deficiency |
|
|
WATER SOLUBLE VITAMINS
- Schilling Test is used for testing what? |
- Etiology of Vitamin B12 deficiency
(B12 deficiency vs. Malabsorption vs. Pernicious anemia) |
|
|
NEUROPATHY
- seen in Vitamin B6 Deficiency - seen in Vitamin B9 Deficiency - seen in Vitamin B12 Deficiency |
- REVERSIBLE
Peripheral Neuropathy (+ irritability & convulsions) - NONE - IRREVERSIBLE Neuropathy (involving DCML & Lat. Corticospinal Tracts) |
|
|
Vitamin deficiency associated with Subacute Combined Degeneration (myelin loss of DCML & Lat. Corticospinal tracts)?
|
- B12
|
|
|
Vitamin Deficiency which can cause possible irreversible neuropathy
|
- B12
|
|
|
Vitamin Deficiency associated with Crohn's Dz?
How does Crohn's Dz cause the deficiency? |
- B12
- Absence of Terminal Ileum |
|
|
Gastric Bypass Surgery
- may cause what vitamin deficiency? - how so? |
- B12
- Intrinsic Factor Deficiency |
|
|
WATER SOLUBLE VITAMINS
- vitamins with SMALL reserve in the Liver - vitamins with LARGE reserve in the Liver |
- B9 (Folic acid)
- B12 (Cyanocobalamin) |
|
|
ANEMIA
- seen in B6 deficiency - seen in B9 deficiency - seen in B12 deficiency - seen in Vitamin E deficiency |
- Sideroblastic Anemia
- Macrocytic, Megaloblastic Anemia - Macrocytic, Megaloblastic Anemia - Pernicious Anemia - Hemolytic Anemia |
|
|
WATER SOLUBLE VITAMINS
- which vitamin deficiencies manifest Hypersegmented Neutrophils? |
- B9
- B12 |
|
|
SIDEROBLASTIC ANEMIA
- Associated vitamin deficiency - Microcytic or Macrocytic? - why does anemia occur? |
- B6 deficiency
- Microcytic - available IRON can not incorporate into Hb |
|
|
SIDEROBLASTIC ANEMIA
- what are sideroblasts? |
- Nucleated, immature RBC with Iron accumulation seen in perinuclear mitochondria
|
|
|
B12 Vitamin Deficiency
- can be confused with? - why? - what should you do? - why? |
- B9 deficiency
- both have Macrocytic, Megaloblastic anemia with hypersegmented neutrophils - Tx for B12 deficiency - b/c prolonged B12 def. causes irreversible neuropathy |
|
|
1st line of Tx in Trigeminal Neuralgia
|
- Carbamezapine
|
|
|
TETRAHYDROFOLATE (THF)
- vitamin that's converted into THF? - required COFACTOR for THF synthesis - enzyme associated with cofactor |
- B9 (Folate)
- B12 (Cyanocobalamin) - Homocysteine-Methyltransferase |
|
|
S- ADENOSYL-METHIONINE (SAM)
- what reaction froms SAM? |
(SAM backwards)
Methionine + ATP ==> SAM |
|
|
S- ADENOSYL-METHIONINE (SAM)
- function? |
- transfers Methyl units
|
|
|
S- ADENOSYL-METHIONINE (SAM)
- in order regenerate SAM, what reactant must be regenerated? - regeneration of the above reactant (thus SAM) requires what vitamins? |
- Methionine
- B9 (Folate) - B12 (Cyanocobalamin) |
|
|
S- ADENOSYL-METHIONINE (SAM)
- the conversion of what neurotransmitter requires SAM? |
Conversion of NE to Epinephrine
|
|
|
B9 (Folate) & B12 (Cyanocobalamin) are both required in the formation/regeneration of what methyl donors?
|
- THF
- SAM |
|
|
|
|
|
BIOTIN
- required for what type of enzymes? - list 3 important enzymes that require Biotin |
- Carboxylation enzymes which add 1C
(PAP) - Pyruvate Carboxylase - Acetyl-CoA Carboxylase - Propionyl-CoA Carboxylase |
|
|
BIOTIN
- give 3 important reactions involving Biotin as a cofactor (include the change in Carbon #) |
Pyruvate Carboxylase:
Pyruvate (3C) ==> Oxaloacetate (4C) Acetyl-CoA Carboxylase: Acetyl-CoA (2C) ==> Malonyl-CoA (3C) Propionyl-CoA Carboxylase: Propionyl-CoA (3C) ==> Methylmalonyl-CoA (4C) |
|
|
BIOTIN
- Biotin Deficiency causes what symptoms. x3 |
(Biotin = Bald)
- Alopecia - Dermatitis - Enteritis |
|
|
BIOTIN
- Biotin Deficiency can be caused by? x2 |
- Antibiotic use
- Ingestion of Raw Eggs |
|
|
Excessively ingesting Raw Eggs will lead to what vitamin deficiency?
What protein in the Raw Eggs is responsible for causing the deficiency? |
- Biotin deficiency
- Avidin (Avidin in eggs Avidly bind Biotin) |
|
|
VITAMIN A
- cofactor for what hormone? - necessary for production of? - used in maturation of what cells? |
- PTH
- CSF - Epithelial cells (hair, skin, eyes, pancreas, mucus-secreting cells) |
|
|
VITAMIN A
- Deficiency symptoms? |
- Night blindness
(and dry skin) |
|
|
VITAMIN A
- contraindicated in what patients? - why? |
- pregnant patients
- Teratogenic (cleft palate, cardiac abnormalities,...) |
|
|
VITAMIN A
- Vitamin A is the basis of what meds? - used to treat what? - what precaution should be made? |
- Isotretinoin
- Severe Acne - Pregnancy test (b/c it is a teratogen) |
|
|
VITAMIN A
- Deficiency causes what changes in plasma levels? |
- PTH decrease
- Calcium decrease - Phosphorous increase (note: Ca+ & Phos. in "A"nti - directions) |
|
|
VITAMIN D
- Deficiency causes what plasma level changes? |
- Calcium decrease
- Phosphorous decrease (note: both go "D"own) |
|
|
VITAMIN D
- effects on Skeletomuscle system - this effect causes what electrolyte changes & where? |
- Increases Bone Resorption
(thus to Mineralize bone) - Increases [Ca2+] & [Phosphorous] in the ECF (to provide Ca2+ & Phos. from old bone to new bone) |
|
|
VITAMIN D
- effects on GI system - how is this effect different from the effects of PTH? |
- Increases Ca2+ & Phosphorous absorption
- PTH does not increase Phosphorous absorption from gut. (PTH = Phosphorous Trashing Hormone) |
|
|
VITAMIN D
- effects on the Renal System |
- Increases Ca2+ & Phosphorous Reabsorption
|
|
|
VITAMIN D
- what is the active form of Vitamin D? - aka? |
1,25 - Dihydroxycholecalciferol
(or 1,25-OH D3) Calcitriol |
|
|
VITAMIN D
- what enzyme activates inactive Vitamin D into it's active form? - under what condition would this enzyme become active? |
1-alpha hydroxylase
- Decreased Ca2+ - Decreased Phosphorous - Increased PTH |
|
|
VITAMIN D
- Vitamin D deficiency causes what diseases? |
- Rickets (in kids)
- Osteomalacia (adults) |
|
|
VITAMIN D
- Vitamin D deficiency causes what change in plasma levels? - this change causes what manifesting symptom? |
- Hypocalcemia
- Tetany |
|
|
VITAMIN D
- Vitamin D excess causes what changes in plasma levels? |
- Hypercalcemia
(also hypercalciuria) |
|
|
VITAMIN D
- Excess levels of activated Vitamin D in the plasma is associated with what disease? - what causes the massive activation of Vitamin D? |
- Sarcoidosis
- Epithelioid Macrophages |
|
|
Hypercalcemia & Hypercalciuria associated with what vitamin disorder?
|
Excess Vitamin D
|
|
|
VITAMIN D
- Excess Vitamin D causes what symptoms? x2 |
- Loss of Appetite (leads to weight loss)
- Stupor |
|
|
VITAMIN D
- discuss amounts seen in Drinking Milk - discuss amounts seen in Breast Milk |
- Fortified with Vitamin D
- Decreased amounts of Vitamin D |
|
|
OsteoBLASTIC activity is stimulated by?
OsteoCLASTIC activity is stimulated by? |
- Vitamin D
- PTH |
|
|
VITAMIN D
- Associated Dz where Father gives to ALL his daughters. - Inheritance pattern |
- Vitamin D Resistant Rickets
- X-Linked Dominant |
|
|
Vitamin D deficiency does not improve with administration of Vitamin D. What is the diagnosis?
|
- Vitamin D Resistant Rickets
|
|
|
Dz associated with LATERAL Bowing of Legs
Dz associated with ANTERIOR Bowing of Legs |
- Rickets
(Vitamin D Deficiency) - Syphillis |
|
|
VITAMIN E
- primary function - functional benefits for what cells? |
- Antioxidant for your blood
- Protects RBC membranes (from free radicals) |
|
|
VITAMIN E
- Deficiency causes what effects on what cells? |
( E is for Erythrocytes)
- Increased Fragility of RBC membranes |
|
|
VITAMIN E
- causes what type of Anemia? |
- Hemolytic Anemia
|
|
|
VITAMIN K
- primary function is to Katalyze what what reaction? - Katalyze what residues? |
- gamma-carboxylation
- glutamate residues (concerned with blood clotting) |
|
|
VITAMIN K
- is necessary for the synthesis of what clotting factors? x6 |
Factors
- II - VII - IX - X Protein C Protein S |
|
|
VITAMIN K
- synthesized by what? - clinical correlation? |
- intestinal flora
- Neonates have sterile intestines, so can not synthesize Vitamin K. Thus give Vitamin K injection |
|
|
VITAMIN K
- Deficiency causes what Dz? - Lab results for clotting time? |
- Neonatal Hemorrhage
- Prolonged PT - Prolonged aPTT - Normal Bleeding Time |
|
|
VITAMIN K
- Deficiency can occur in adults after prolonged period of what? |
- usage of Broad Spectrum Antibiotics
|
|
|
Vitamin Requirements
- Carboxylation - Decarboxylation |
- Biotin
- B6 (PP) |
|
|
PT tests what clotting factor pathway?
Follow with what anti-coagulant? |
Extrinsic
Warfarin (WE - HI) |
|
|
aPTT tests what clotting factor pathway?
Follow with what anticoagulant? |
Intrinsic
Heparin (WE - HI) |
|
|
ZINC
- Zinc deficiency causes what unique symptoms x3 |
- dyguisia
- anosmia - hypogonadism (also hair loss everywhere) |
|
|
SARCOIDOSIS
- Plasma electrolyte changes? - Urine electrolyte changes? - what accounts for these changes? |
- Hypercalcemia
- Hypercalciuria - Increased activated Vitamin D |
|
|
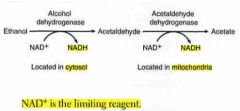
ETHANOL METABOLISM
- occurs in what 2 locations? - what are the enzymes in those locations? |
1st) Cytosol
2nd) Mitochondria - Alcohol DHase (in cytosol) - Acetaldehyde DHase (in mito) |
|
|
ETHANOL METABOLISM
- what is the limiting reagent? |
NAD+
|
|
|
ETHANOL METABOLISM
- which enzyme operates at Zero-order kinetics? - where is this enzyme located? |
- Acetaldehyde DHase
- Mitochondria |
|
|
ETHANOL METABOLISM
- causes what ratio change? - where? |
- increases NADH/NAD+ ratio
- Liver |
|
|
ETHANOL METABOLISM
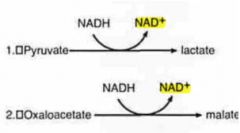
- Increased NADH/NAD+ ratio will drive what 2 reactions? |
(PL OM wine)
Pyruvate ==> Lactate Oxaloacetate ==> Malate |
|
|
ETHANOL METABOLISM
- what 2 amino acids are driven to formation? - this stimulates what process? - also inhibits what process? |
- Lactate
- Malate - Fatty acid synthesis - Gluconeogenesis |
|
|
ETHANOL METABOLISM
- In chronic alcoholism, what process is stimulated continuously? - thus leading to what sign/symptom? |
- Fatty acid synthesis
(from increased lactate & malate) - Fatty Liver (hepatocellular steatosis) |
|
|
ETHANOL METABOLISM
- In chronic alcoholism, what process is inhibited continuously? - thus leading to what sign/symptom? |
- Gluconeogenesis
(from increased lactate & malate) - Hypoglycemia |
|

|
|
|
|
|
|
|
Kwashiorkor is malnutrition of?
Marasmus is malnutrition of? |
- Protein
- Energy |
|
|
Kwashiorkor signs/symptoms
|
(Kwashiorkor results from Protein-deficient MEAL)
- Malnutrition - Edema - Anemia - Liver (fatty) |
|
|
Marasmus signs/symptoms
|
- Muscle wasting
|
|
|
Small skinny child with swollen belly. What is the Dx?
|
- Kwashiorkor
|
|
|
What metabolism processes occur in the Mitochondria?
|
(Mighty BOAT)
- Beta oxidation of FA - Oxidative Phosphorylation - Acetyl-CoA production - TCA |
|
|
What metabolism processes occur in the Cytoplasm?
|
(Sight-O-GPS)
Glycolysis Pentose Phosphate Shunt (HMP) Synthesis of: ==> Fatty acids ==> Proteins ==> Steroids |
|
|
What metabolism processes occur in both the mitochondria and cytoplasm?
|
(it takes 2 to HUG)
- Heme synthesis - Urea cycle - Gluconeogenesis |
|
|
What is the difference in function between a Kinase vs. Phosphorylase?
|
- Kinase uses ATP to add phosphate group
- Phosphorylase does NOT use ATP |
|
|
Dehydrogenase enzymes oxidize or reduce substrates?
|
Oxidizes
|
|
|
RATE LIMITING ENZYME
- Fatty acid synthesis? - Fatty acid oxidation? |
("Fat Ass Cat")
- Acetyl-CoA Carboxylase (ACC) - Carnitine Acyltransferaes I (CAT I) |
|
|
RATE LIMITING ENZYME
- which one requires B6? |
- Glycogen phosphorylase
(Glycogenolysis) |
|
|
RATE LIMITING ENZYME
- which one requires Biotin (B7)? |
- Acetyl-CoA Carboxylase
(Fatty Acid Synthesis) |

