![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
48 Cards in this Set
- Front
- Back
|
what are the bacterial mechanisms used against phagocytes:
1. 2. 3. 4. |
1. avoid detection phagocytes
2. lyse phagocytes 3. inhibit phagocytes 4. prevent intracellular killing |
|
|
how do bacteria avoid detection by phagocytes:
|
via capsules or the enzyme coagulase
|
|
|
how do bacteria prevent engulfment by phagocytes (inhibit):
|
via their capsules and M protein
|
|
|
...(bacteria) uses both its capsule and the M protein to prevent engulfment by phagocytes
|
Streptococcus pyogenes
|
|
|
how does the following organism prevent intracellular killing:
Mycobacterium tuberculosis |
prevents fusion of the phagocyte with the lysosome
|
|
|
how does the following organism prevent intracellular killing:
Staphylococcus aureus |
uses its capsule or enzymes to make itself resistant to the lysosomal enzymes
|
|
|
how does the following organism prevent intracellular killing:
Rickettsia species |
dissolves the phagolysosome membrane and escapes
|
|
|
what are the 3 bacterial mechanisms devised against antibodies and complement:
1. 2. 3. |
1. antigenic variation
2. inactivation of antibodies 3. inactivation of complement |
|
|
how do bacteria vary their antigen:
|
change their surface proteins
|
|
|
how do bacteria inactivate antibodies:
|
by destroying antibodies
|
|
|
how do bacteria inactivate complement:
|
by masking themselves or interrupting the complement cascade
|
|
|
Capsules are one of the most important virulence factors. They can protect the cell from ...
|
complement
|
|
|
how do bacterial capsules increase virulence:
1. 2. |
1. prevent phagocyte-mediated destruction
2. promoting adherence |
|
|
The M protein is produced by ... It is a long fibril, attached at one end to the cytoplasmic membrane, and extending out through ...
The M protein is ..., allowing the cell to attach to the mucous membrane of the ... The M protein also inhibits ... activation, which prevents ... and therefore phagocytosis. |
Streptococcus pyogenes
the cell wall an adhesin oropharynx complement opsonization |
|
|
Point mutations in one region of the gene for the M protein can change the ... of the protein without altering its function. Antibodies to one form of the protein do not react with other forms of the protein. This is a form of ...
|
antigenicity
antigenic variation |
|
|
Like the capsule, the M protein works on two levels:
1. 2. |
1. promotes the colonization and invasion of the host
2. helps the bacterium avoid the host’s immune system |
|
|
Anaerobic bacteria produce ... and ... as byproducts of ... These products can damage ... and spread the ...
|
acid
gas fermentation tissue infection |
|
|
... enzymes can destroy tissue locally, providing ... for bacterial growth and helping spread the ...
|
degradative
nutruients infection |
|
|
Endotoxin is actually the ... of the LPS from ... bacteria. During infection large amounts of endotoxin can be released which causes:
1. 2. 3. 4. |
Lipid A portion
Gram-negative 1. fever 2. diarrhea 3. vomiting 4. shock |
|
|
While Gram-positive organisms do not have ..., and therefore do not produce endotoxin, they do release:
1. 2. 3. These compounds can produce symptoms similar to those produced by endotoxin, however: |
an outer membrane
1. peptidoglycan 2. teichoic acids 3. lipoteichoic acids they are much weaker toxins |
|
|
... are proteins which are secreted by bacteria and damage or kill host cells
|
Exotoxins
|
|
|
what are the 3 classes of exotoxins:
1. 2. 3. |
1. type 1
2. type 2 3. type 3 |
|
|
1. type 1 exotoxins act on what:
2. and do what: |
1. cytoplasmic membrane of host
2. bind to receptors on cytoplasmic membrane and cause changes within host cell |
|
|
type 2 exotoxins do what:
|
damage host cell cytoplasmic membrane
|
|
|
type 3 exotoxins do what:
|
enter cell and cause changes within host cell cytoplasm
|
|
|
what does Escherichia coli Heat Stable Toxin (STa) cause:
and what is its mode of action: |
diarrhea
binds to guanylate cyclase activating it leading to an increased level of cGMP. The end result of this is secretion of water and electrolytes from the cell |
|
|
Exotoxins that act on the small intestine are called ...
|
enterotoxins
|
|
|
where do superantigens bind:
|
they bind to the T cell receptor and MHC class II protein on antigen-presenting cells outside the normal antigen binding site
|
|
|
instead of activating a very small number of T-cells, superantigens activate up to ...% of all T-cells resulting in the release of large amounts of ... and causing a systemic reaction including:
1. 2. 3. 4. |
20
cytokines 1. fever 2. diarrhea 3. vomiting 4. shock |
|
|
what are examples of superantigens:
1. 2. |
1. Staphylococcus aureus TSST-1
2. Streptococcus pyogenes SPEs (Streptococcal pyrogenic exotoxins) |
|
|
There are two classes of Type 2 exotoxins:
1. 2. |
1. Pore-forming Type 2 Exotoxins
2. phospholipases (they destroy the cytoplasmic membrane) |
|
|
... of ... makes pores in cytoplasmic membranes in erythrocytes and endothelial cells.
|
α-toxin
Staphylococcus aureus |
|
|
... are pore-forming exotoxins made by species of four genera of Gram-positive bacteria: Streptococcus, Listeria, Clostridium and Bacillus. These toxins bind to cholesterol in membranes and cause cell death
|
Cholesterol-binding cytolysins
|
|
|
... have a sequence of nine amino acids which is repeated multiple times within the toxin and are found in several Gram-negative species such as E. coli. The toxins form pores which cause cell death either by osmotic lysis or by inducing apoptosis
|
RTX toxins
|
|
|
Several bacterial species, both Gram-positive and Gram-negative, produce ... that disrupts the phospholipid portion of the membrane.
|
phospholipase C
|
|
|
what are the three sub-classes of Type 3 AB exotoxins:
1. 2. 3. |
1. protein inhibitors which inhibit translation
2. neurotoxins that inhibit the release of various neurotransmitters 3. cAMP inducers increase the activity of adenylate cyclase, resulting in increased cAMP levels |
|
fill in the above chart:
|
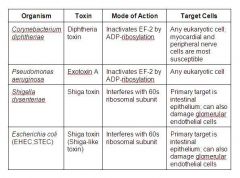
(see figure)
|
|

fill in the above chart:
|

(see figure)
|
|

fill in the above chart:
|

(see figure)
|
|
|
identify the subclass of the following groups of bacteria:
A: Corynebacterium diphtheriae Pseudomonas aeruginosa Shigella dysenteriae Escherichia coli (EHEC;STEC) B: Escherichia coli (ETEC) Vibrio cholerae Bacillus anthracis Bordetella pertussis C: Clostridium tetani Clostridium botulinum |
A. Protein Inhibitors
B. cAMP Inducers C. Neurotoxins |
|
|
Corynebacterium diphtheriae infects a person and if the bacterium carries the ... with the toxin gene, it starts producing ... The toxin binds to a receptor on the cell surface and enters the cytoplasm of the host cell and adds an ADP-ribose molecule to ... and kills the ribosomes, stopping ...
|
phage
diphtheria toxin EF-2 protein synthesis |
|
|
Exotoxin A is produced by ... It inhibits translation elongation in host cells in the region of the infection, leading to cell death. The genes for the toxin are located on a (phage/chromosome)
|
Pseudomonas aeruginosa
chromosome |
|
|
Escherichia coli produces two types of ... toxin, Stx1 and Stx2. These toxins are produced by ... E. coli strains and are
|
Shiga
enterohemorrhagic |
|
|
Stx2 is associated with ..., which can result in acute renal failure
|
hemolytic uremic syndrome (HUS)
|
|
|
Tetanus toxin is a neurotoxin produced by ... Spores of this organism are commonly found in ... They can contaminate wounds and germinate there. Since the organism is ..., it grows best in deep puncture wounds. The toxin gene is located on a ... and so can be transferred by ...
|
Clostridium tetani
soil anaerobic plasmid conjugation |
|
|
Tetanus toxin is a ... which prevents neurotransmitter ... release. This causes muscle ...
|
protease
GABA contraction |
|
|
... produces a toxin called botulinum toxin. Remember that this is a ... poisoning.
the toxin prevents the release of ... from the neuron. Therefore, the muscle cell never ... |
Clostridium botulinum
food acetylcholine contracts |
|
|
... is produced by ETEC strains of E. coli. The toxin stimulates ... activity of the intestinal epithelial cells causing an increase in cAMP. This causes the cells to secrete chloride and reduces sodium absorption, resulting in ... The genes are on a ... and can therefore be moved by ...
|
heat labile toxin (LT)
adenylate cyclase diarrhea plasmid conjugation |

