![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
32 Cards in this Set
- Front
- Back
|
what are the common routes of entry for pathogens:
1. 2. 3. 4. |
1. skin
2. respiratory system 3. digestive system 4. urogenital system |
|
|
once inside the body, microorganisms can reside in several key locations:
|
intracellular
-vesicular -cytoplasm extracellular -interstitial spaces (blood, lymph -epithelial cell surfaces |
|
|
what are the components of the immune system:
1. 2. 3. 4. what are the other key players: 1. 2. 3. 4. 5. |
1. lymph nodes
2. thymus 3. spleen 4. long bones 1. skin 2. mucous membranes 3. chemical factors 4. leukocytes 5. commensal bacteria |
|
|
innate immunity is our 1st line of defense, what are its general features:
1. 2. 3. 4. 5. |
1. non-specific
2. constitutively present/immediate response 3. phylogenetically ancient (found in almost every living organism) 4. limited repertoire of recognition molecules 5. no memory or lasting immunity |
|
|
innate vs. adaptive immunity, what are the key differences:
1. 2. 3. 4. 5. |
1. speed of response
2. cellular mediators differ 3. protective mechanisms vary greatly 4. adaptive response is more specific 5. adaptive response allows for immunologic memory |
|
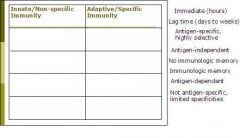
place the descriptions in the correct box:
|
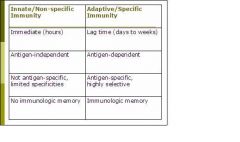
(see figure)
|
|
|
which branch of the immune system is more imperative to the survival of an organism:
|
innate immunity
|
|
|
what are the types of innate immune barriers:
1. 2. 3. 4. |
1. anatomical
2. chemical 3. humoral 4. celluar |
|
|
what are the anatomical barriers to infection:
1. 2. |
1. skin (epithelia)
2. mucous membranes |
|
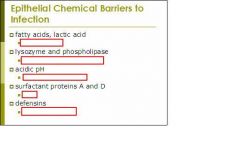
fill in the sources of the chemical barriers:
|
(see figure)
|
|
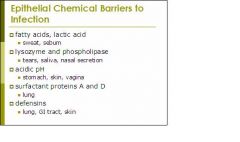
fill in the chemical barriers for the sources listed:
|
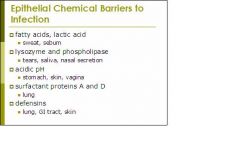
(see figure)
|
|
|
epithelia of the skin and GI tract also has an additional layer of protection--- provided by ... bacteria
|
commensal
|
|
|
what are the humoral barriers to infection:
1. 2. 3. 4. 5. 6. 7. |
1. complement system
2. coagulation 3. protease inhibitors 4. lysozyme 5. interferons 6. lactoferrin and transferrin 7. cytokines |
|
|
Lectoferrin and transferrin possess antimicrobial activity by sequestering free ... that is needed for microbial function
|
iron
|
|
|
... and ... are protease inhibitors that work by “tricking” the bacterial protease to cleave them, forming an inactive ... bound intermediate in the process
|
serpin
alpha 2-macroglobulin covalently |
|
|
what does the following describe:
Produced by virus-infected cells Inhibit viral replication Signal neighboring uninfected cells to prepare for viral infection Alerts other cells of immune system Makes virus-infected cells more vulnerable to attack by killer lymphocytes |
type I interferons (alpha, beta, gamma)
|
|
|
what are the 3 main effects of IFN secretion
1. 2. 3. |
1. alert neighboring cells
2. increases expression of antigen-presenting cell surface molecule MHC class I 3. activates nature killer (NK) cells that kill virally infected cells |
|
|
what are the 2 main types of interferons:
1. 2. |
1. alpha
2. beta |
|
|
what is the function of complement activation:
|
complement or augment the immune response
|
|
|
what are the 3 pathways that lead to activation of complement:
1. 2. 3. |
1. classical pathway
2. lectin pathway 3. alternative pathway |
|
|
1. what activates the classical complement pathway:
2. what activates the alternative complement pathway |
1. antibody-antigen complex
2. molecules on pathogens surface |
|
|
what are the results of complement activation:
1. 2. 3. |
1. recruitment of inflammatory cells
2. opsonization of pathogens 3. killing of pathogens by effector cells |
|
|
what is opsonization:
|
when pathogens are tagged for destruction
|
|
|
in the classical pathway, complement components ..., ..., and ... must be activated prior to activation of C3. In the alternative pathway, these components are replaced by ..., ..., and ... The remainder of the pathway is the same for each mechanism.
|
C1
C4 C2 factor D factor B properdin |
|
|
what are the basic steps of complement starting with cleavage of C3:
1. 2. 3. 4. |
1. C3 is cleaved into C3a and C3b
2. C3b covalently attaches itself to bacterium 3. C3a attracts effector cells (i.e. phagocytes) to the site of infection 4. the newly arrived effector cells bind to complement "tag" on the pathogen, signaling phagocytosis and destruction |
|
|
C3 is hydrolyzed into ... and ... fragments. ... is the smaller, soluble fragment that recruits phagocytes to the site of infection while ... is the larger fragment that attaches to the surface of the pathogen, tagging it for destruction. This molecular tag is also called an ..., and ... is the process of “tagging” a pathogen.
|
C3a
C3b C3a C3b opsonin opsonization |
|
|
rate of hydrolysis of C3 to C3a and C3b can be increased through formation of ...
|
C3 convertase
|
|
|
initial product of spontaneous hydrolysis of C3 is called ... which binds to ... in the blood or extracellular fluid, making that factor susceptible to cleavage by ... this cleavage produces a complex called ... or ... which then activates more ... molecules. The C3b fragments attach to the microbial surface and can be used either (1) ... or (2) ...
|
iC3
factor B factor D C3 convertase iC3Bb C3 (1) to make more C3 convertase (2) as an opsonin |
|
|
..., also known as ... binds to ... on the microbial surface, stabilizing and protecting it from inhibition by factor H.
|
Properdin
Factor P C3 convertase |
|
|
... activates C5 and ..., forming pores in the microbial membrane and ... This is also referred to as the ...
|
C5 convertase
C6-C9 cell lysis “membrane-attack complex” (MAC) |
|
|
The activation and cleavage of C5 also produces soluble ..., the most potent of the ..., causing significant recruitment of neutrophils and inflammation.
|
C5a
anaphylatoxins |
|
|
Initiation of the alternative complement pathway on the surface of human cells is stopped at an early stage by:
1. 2. 3. |
1. decay-accelerating factor (DAF)
2. membrane co-factor protein (MCP) 3. plasma protein factor H |

