![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
282 Cards in this Set
- Front
- Back
|
Define: Women's Health
|
defined currently as a multidisciplinary approach to the health and care of women patients.
Women's health focuses on conditions unique in women (pregnancy), conditions that are more common in women (breast cancer, osteoporosis, rape, and hypertension), and conditions that have different presentations, natural history, risk factors, prevention, or treatments in women and men (heart disease, urinary tract infections, sexually transmitted diseases). |
|
|
Framingham Study
|
a longitudinal prospective cohort of adults living in Framingham, Massachusetts.
The initial goal of the study was to identify risk factors for heart disease by following this large and stable cohort of men and women in their 40s. In the initial reports, men with chest pain were more likely to die of heart disease than women who reported chest pain. This supported the perception at the time that heart disease was a disease of men. It wasn't until women were observed into their 50s that women began developing symptoms and dying of heart disease. When researchers looked back and further defined chest symptoms from the earlier reports, it was found women and men with typical angina symptoms had similar outcomes. However, women were more likely to report any symptoms than men, including some type of chest pain. The Framingham data set also revealed that silent myocardial infarctions are more common in women than men. |
|
|
The Nurse's Health Study
|
a national ongoing survey of a cohort of female nurses that has provided detailed information about risk factors, disease presentation, and outcomes for decades.
Participants complete extensive questionnaires regularly and have occasionally provided specimens for analysis. Because it is a prospective cohort group, it has been possible to evaluate many risk factors. Among tobacco smokers, the adverse health effects are dose related, and those smoking one or two cigarettes daily have less health problems than those smoking a pack of cigarettes daily but more problems than nonsmokers. |
|
|
Women's Health Initiative (WHI)
|
enrolled women 50 to 79 years of age in three clinical trials and an observational arm.
The clinical trials were all randomized, double-blinded with placebo control. Two were designed to resolve questions about the impact of estrogens and estrogens plus progesterone on the risk for a variety of important health outcomes for women during the postmenopausal period. These included cardiovascular risk, maintenance of bone density, risk for breast cancer, and development of dementia. Although these pharmaceutical trials have ended, the observational study continues. The WHI clinical trials of hormonal therapy have dramatically changed the therapeutic approach to menopause |
|
|
On average how much shorter are women than men
|
5 inches
|
|
|
Who has the smaller renal mass: men or women?
|
Women
this has been acknowledged in defining normal renal function |
|
|
Difference between urethra size: men and women
|
The shorter urethral distance places women at much higher risk for urinary tract infections than men
|
|
|
What is the 2nd leading cause of death in men and women
|
Cancer
|
|
|
What is the most common newly diagnosed cancer and cause of death found in women
|
Breast
|
|
|
What is the most common newly diagnosed cancer and cause of death found in men
|
Prostate
|
|
|
What the the most common cause of death in men and women?
|
Cardiovascular disease
|
|
|
What is the third most common cause of death in men and women?
|
Stroke
|
|
|
What hormone must be released to lead to ovarian stimulation?
|
Gonadotropin-Releasing Hormone (GnRH)
|
|
|
What organ produces Gonadotropin-Releasing Hormone (GnRH)?
|
Hypothalamus
|
|
|
What hormones does the pituitary gland release?
|
the luteinizing hormone (LH) and follicular-stimulating hormone (FSH)
|
|
|
What causes regular menstrual cycles?
|
most women develop a regular menstrual cycle with associated periodic increases in estrogen and then progesterone in response to the luteinizing hormone (LH) and follicular-stimulating hormone (FSH) released by the pituitary gland.
|
|
|
Where are estrogen receptors located?
|
Increasing numbers of estrogen receptors have been identified in both reproductive and nonreproductive organs, including brain, arterial vessel wall, bone, smooth muscle, and urethra.
|
|
|
What are the three phases of the menstrual cycle?
|
follicular or proliferative phase
ovulation luteal or secretory phase |
|
|
how long does a menstrual cycle last?
|
between 21 and 35 days
|
|
|
What happens during the follicular phase of the menstrual cycle?
|
the hypothalamus secretes GnRH
this stimulates the pituitary to release FSH and LH. These hormones in turn stimulate estrogen secretion by a cohort of ovarian follicles. The estrogen secretion simultaneously facilitates proliferation of the endometrium. Eventually, one follicle becomes dominant and is destined for ovulation. |
|
|
What happens during the ovulation phase of the menstrual cycle?
|
Ovulation occurs soon after the LH surge (from the pitutary gland).
With ovulation, the oocyte leaves the dominant follicle and migrates toward the fallopian tubes. At this time, the cervical mucus covering the cervical os become less viscous, thus facilitating passage of sperm at the uterine entrance. |
|
|
What happens in the luteal phase of the menstrual cycle.
|
After the occyte leaves the dominant follicle the remaining cells in the follicle become the corpus luteum, which produces progesterone
If fertilization does not occur, progesterone is secreted for about 14 days, and then the follicle involutes. This is associated with decreasing levels of estrogen and progesterone. The endometrium sheds in response to the falling estrogen and progesterone levels and results in menstruation. If fertilization occurs, progesterone continues to be secreted to support early pregnancy. |
|
|
Preventive Health Recommendations for Women: Obesity
|
Recommendation: Blood pressure, height and weight, body mass index every 1-2 years
|
|
|
Preventive Health Recommendations for Women: Hyperlipidemia
|
Lipid Panel starting at age 45
|
|
|
Preventive Health Recommendations for Women: Cancer
|
Mammogram starting at age 40 (annual)
Pap smear every 1-3 years in women with cervix |
|
|
Preventive Health Recommendations for Women: iv. Fecal occult blood testing, sigmoidoscopy, or colonoscopy
|
Annual starting at age 50
|
|
|
Preventive Health Recommendations for Women: Chlamydia
|
Annual at age 25, then if patients remains high risk.
|
|
|
Preventive Health Recommendations for Women: Osteoporesis
|
Annual starting at age 65
|
|
|
Preventive Health Recommendations for Women: Mental health
|
All adults
|
|
|
Preventive Health Recommendations for Women: Immunizations: Influenza
|
Yearly
|
|
|
Preventive Health Recommendations for Women: Immunizations: Rubella
|
Check titer or vaccinate
|
|
|
Preventive Health Recommendations for Women: Immunization: Tetanus-diphtheria-(pertussis)
|
dT every 10 yr (TdAP booster at least once after age 11 yr)
|
|
|
Preventive Health Recommendations for Women: Immunization: Human papillomavirus
|
before age 26
|
|
|
Preventive Health Recommendations for Women: Immunization: Varicella
|
Susceptible women
|
|
|
Preventive Health Recommendations for Women: Chemoprophylaxis: Folic acid
|
400 mcg daily
|
|
|
Preventive Health Recommendations for Women: Chemoprophylaxis: Calcium intake/supplement:
|
periodically
|
|
|
Preventive Health Recommendations for Women: Additional screening and counseling during pregnancy: Rh(D) incompatibility screening, iron deficiency anemia, asymptomatic bacteriuria
|
Testing in first trimester
|
|
|
Preventive Health Recommendations for Women: Additional screening and counseling during pregnancy: Rubella
|
check titer, vaccinate postpartum if negative
|
|
|
Health Issues Across the Life Course: Adolescent: APPROACH TO THE ADOLESCENT
|
Providing health care to adolescents requires specific skills of the medical provider.
Adolescent patients are naïve health consumers and often do not express their needs clearly and often have a very limited knowledge of their own physiology Many young women are reluctant to engage in the medical encounter because of embarrassment or fear. It is incumbent on the medical provider to acknowledge these issues and engage the adolescent using developmentally appropriate language and a compassionate manner. |
|
|
Health Issues Across the Life Course: Adolescent: CONFIDENTIALITY
|
Most adolescents come to office appointments accompanied by an adult.
Time spent alone with the patient is critical to discovering hidden agendas. Because statutes for the care of minors vary from state to state, the medical provider must be familiar with what legal rights young patients have to accessing reproductive health services without the involvement of a parent. |
|
|
Health Issues Across the Life Course: Adolescent: SEXUAL HISTORY
|
Gender and number of past and present partners should be tactfully elicited as part of the sexual history along with history of sexual abuse, assault, date rape, or physically abusive partner.
It is also important to know whether the patient is intoxicated during sex because intercourse may not be voluntary or protected. Young women need to be encouraged to be safe and selective in their relationships and encouraged either to abstain from sex (i.e., oral, vaginal, or anal sex) or to be in a long-term, mutually monogamous relationship with an uninfected partner. Health providers may need to teach young patients strategies in self-advocacy and "how not to have sex," as well as helping young women understand what constitutes a "healthy" relationship. Risk for pregnancy and contraceptive options are also important topics for discussion. |
|
|
Why are younger women more biologically susceptible to sexually transmitted infections?
|
because of cervical ectopy
|
|
|
Health Issues Across the Life Course: Adolescent: When adolescents get sexually transmitted disease
|
Patients with confirmed disease should complete therapy, notify their partners to be treated, and abstain from sex until all partners are tested and complete treatment. Because of the risk for reinfection subsequent to treatment, patients with confirmed disease should be rescreened in 3 months.
|
|
|
How long after having a sexually transmitted disease should an adolescent be re-screened?
|
3 months
|
|
|
When to start Guardasil
|
recommended routine vaccination of females aged 11 to 12 years with three doses of the quadrivalent HPV vaccine. Catch-up vaccination is recommended for females aged 13 to 26 year
|
|
|
Pap smear recommendation
|
recommended in sexually active adolescents about 3 years after initiation of sexual intercourse regardless of HPV vaccination status.
|
|
|
Why are early menstrual cycles irregular?
|
because of a immature hypothalamic-pituitary axis.
|
|
|
Primary amenorrhea: define
|
defined as the absence of a first menses by age 16 years.
|
|
|
When is menarche seen?
|
Menarche is usually seen 2 years after the start of breast development and by the time Tanner stage 4 is reached.
Therefore, a girl who has not begun menses by age 14 years or within 2 years of obtaining Tanner stage 4 breast development should be further evaluated. |
|
|
What is the first differential for adolescents with primary amenorrhea?
|
pregnancy
|
|
|
What is the most common cause of primary amenorrhea?
|
ovarian failure, hypergonadotropic hypogonadism.
This occurs when there is a failure of the ovary to respond to the signals from the pituitary gland and can be caused by Turner syndrome or other genetic abnormalities, or be a sequelae of chemotherapy or radiation therapy received in the past. |
|
|
Why is it so important for women to receive preconception health care?
|
Because nearly half of all pregnancies in the United States are unplanned, preconception health care must be provided on an ongoing basis for all women regardless of whether they are actively planning to conceive.
|
|
|
What should be included in preconception health care?
|
This includes working with women to develop a reproductive plan, to support their efforts to implement that plan, and to identify important health risks and recommendations to improve their health and therefore improve the odds for a healthy pregnancy if and when they choose to conceive.
|
|
|
How much folic acid should women take?
|
400 mcg
|
|
|
What does folic acid prevent?
|
prevents neural tube defects should a woman conceive.
Adequate folic acid levels are critical very early in embryogenesis, and supplementation must begin during the months before conception. |
|
|
Conception and Varicella and MMR vaccine
|
women should avoid conception within 1 month of receiving an MMR or varicella vaccine.
|
|
|
What questions should be include when taking a sexual history?
|
The history should include questions about sexual practices, including number of partners, gender of partners, and steps taken to protect against transmission of infections as well as pregnancy prevention.
Prior history of STIs, as well as specific risks for HIV and hepatitis, should be elicited. Exploration about safety, especially in relation to sexual activity, should be pursued. Finally, condom use and risk reduction strategies should be discussed. |
|
|
Contraception: Always very effective (0%-1% failure)
|
Vasectomy, female sterilization, etonogestrel subdermal implant 68 mg, copper-bearing intrauterine device, levonorgestrel intrauterine device
|
|
|
Contraception: Very effective when used correctly and consistently Effective as commonly used (2%-12% failure)
|
Combined oral contraceptive pills, patches, vaginal rings, depot medroxyprogesterone acetate injection, progesterone-only pills while breastfeeding
|
|
|
Contraception: Effective when used correctly and consistently. Only somewhat effective as commonly used (15%-30% failure)
|
Condom, diaphragm, coitus interruptus, spermicide, cervical cap
|
|
|
The most common method used by women in the United States
|
oral contraceptives.
|
|
|
How do combined contraceptives work?
|
They act to prevent pregnancy through multiple mechanisms, including suppression of ovulation, as well as effects on the uterine lining, tubal function, and cervical mucus.
|
|
|
Combined Contraceptives non contraceptive benefits
|
including a reduced risk for anemia, ovarian cancer, functional ovarian cysts, endometrial cancer, and dysmenorrhea
|
|
|
When is oral contraceptives contraindicated?
|
for women older than 35 years who smoke;
women with a history of heart disease or cerebrovascular disease; women with significantly impaired liver function; women with a history of thromboembolic disorders; and those with known or suspected breast or endometrial cancer, severe hyperlipidemia, migraine with aura, uncontrolled hypertension, symptomatic gallbladder disease, undiagnosed vaginal bleeding, or known or suspected pregnancy. |
|
|
Progestin-Only Methods: name them
|
medroxyprogesterone acetate depot injection Depot-Provera and the progestin-only pill
|
|
|
How do progestin only contraceptive methods work?
|
work by inhibiting ovulation as well as impairing transport of sperm and implantation.
|
|
|
Why would women chose progestin only contraceptives?
|
Both methods can be used by most women with contraindications to estrogens.
|
|
|
How often is Depo Provera taken?
|
The long-acting Depo-Provera is administered by an intramuscular injection every 12 weeks and is a highly effective method of contraception.
|
|
|
What are the side effects of Depo Provera?
|
The major side effects and risks associated with its use are breakthrough bleeding, weight gain, and loss of bone density.
|
|
|
Who uses the progestin only pill?
|
The progestin-only "mini" pill has a lesser degree of effectiveness. This method is less popular and tends to be used in settings in which there is a lower fecundity, such as women in their 40s and women during the postpartum period.
|
|
|
How do intrauterine devices work?
|
They work by preventing fertilization and implantation, and their effects are rapidly reversible upon withdrawal of the device
|
|
|
Plan B
|
Plan B is an oral progestin-only preparation approved by the FDA to prevent pregnancy after unprotected sexual intercourse or a contraceptive failure.
|
|
|
Does Plan B effect an already established preganancy?
|
No
|
|
|
When is Plan B the most effective
|
The over-the-counter method is most effective if begun within 24 hours, but effectiveness with use within 72 hours is up to 89%.
|
|
|
Food and Drug Administration Categories of Drug Safety During Pregnancy: A
|
Adequate, well-controlled studies in pregnant women have not shown an increased risk to the fetus in any trimester of pregnancy.
|
|
|
Food and Drug Administration Categories of Drug Safety During Pregnancy: B
|
Animal studies have revealed no evidence of harm to the fetus; however, there are no adequate and well-controlled studies in pregnant women.
Or: Animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester. |
|
|
Food and Drug Administration Categories of Drug Safety During Pregnancy: C
|
Animal studies have shown an adverse effect, and there are no adequate and well-controlled studies in pregnant women.
Or: No animal studies have been conducted, and there are no adequate and well-controlled studies in pregnant women. |
|
|
Food and Drug Administration Categories of Drug Safety During Pregnancy: D
|
Adequate, well-controlled or observational studies in pregnant women have demonstrated a risk to the fetus. However, the benefits of therapy may outweigh the potential risk.
|
|
|
Food and Drug Administration Categories of Drug Safety During Pregnancy: X
|
Adequate, well-controlled or observational studies in animals or pregnant women have demonstrated positive evidence of fetal abnormalities or risks, and the use of the product is contraindicated in women who are or may become pregnant.
|
|
|
PREGNANCY COMPLICATIONS AND POSTPARTUM CARE: GESTATIONAL DIABETES
|
Women with a history of gestational diabetes are at increased risk for developing adult-onset diabetes later in life.
It is recommended that these women have an oral glucose tolerance or fasting plasma glucose testing at the 6-week postpartum visit and then be followed with periodic testing if this test is normal. Because gestational diabetes identifies women who are at high risk for later diabetes, advice should focus on lifestyle changes, including exercise and weight loss. |
|
|
PREGNANCY COMPLICATIONS AND POSTPARTUM CARE: GESTATIONAL HYPERTENSIVE DISORDER
|
Women whose pregnancies were complicated by a gestational hypertensive disorder, such as preeclampsia or gestational hypertension, are at increased risk for hypertension later in life and should have their cardiovascular risk evaluated, lifestyle modification recommended, and blood pressure followed
|
|
|
PREGNANCY COMPLICATIONS AND POSTPARTUM CARE: POSTPARTUM DEPRESSION
|
Although most mothers experience mood fluctuations after delivery, these symptoms do not interfere with their ability to care for themselves or their infants.
Women whose symptoms persist for 2 weeks or more should be screened for postpartum depression. The two greatest risk factors for postpartum depression are a history of depression before pregnancy and depression during the current pregnancy. There are several tools that can be used to screen for depression, including the CES-D and PHQ-9. |
|
|
PREGNANCY COMPLICATIONS AND POSTPARTUM CARE: POST PARTUM THYROIDITIS
|
an autoimmune thyroiditis that can be seen in 5% to 10% of women during the first postpartum year.
The syndrome presents most often 6 months postpartum and is characterized by transient, often unrecognized, thyroiditis followed by hypothyroidism, and ending with resolution. About 20% to 30% of women will remain hypothyroid. Management focuses on management of symptoms during the hyperthyroid stage, often with β blockers, as well as support with thyroid replacement hormone during the hypothyroid phase. Those women who do return to a euthyroid state are at increased risk for postpartum hypothyroidism during a subsequent pregnancy and at increased risk for hypothyroidism over time. All women will require long-term follow-up with annual thyroid testing. |
|
|
Menstrual disorders are common and generally fall into two main categories:
|
Amenorrhea
Abnormal Uterine Bleeding |
|
|
Abnormalities in menstruation may indicate...
|
problems related to the reproductive system, such as premature ovarian failure,
or may be an early sign of an important underlying systemic illness |
|
|
Define: amenorrhea
|
Defined as the absence of menses for at least 3 to 6 months outside of the setting of pregnancy or lactation.
|
|
|
Primary Amenorrhea
|
generally recognized during the teenage years when menses fail to begin by age 16 years
|
|
|
secondary amenorrhea: define
|
Defined as the absence of menses for at least 3 to 6 months outside of the setting of pregnancy or lactation when they already had a defined menstrual cycle.
|
|
|
Oligomenorrhea: define
|
occurs when menses are irregular or infrequent, with cycle length usually greater than 35 to 40 days, and is often associated with chronic anovulation or oligo-ovulation.
|
|
|
Differential diagnosis for amenorrhea
|
(1) ovarian failure,
(2) anovulation, (3) medication induced, (4) uterine outflow tract abnormalities, and (5) physiologic |
|
|
What is the most common cause of secondary amenorrhea
|
pregnancy
|
|
|
Secondary Amenorrhea : Physiologic causes
|
Pregnancy, lactation, menopause
|
|
|
Secondary Amenorrhea : Ovarian causes
|
Radiation- or chemotherapy-induced ovarian failure, chromosomal abnormalities, autoimmune or idiopathic premature ovarian failure
|
|
|
Secondary Amenorrhea : Anovulation causes
|
Hyperandrogenism (polycystic ovary syndrome, congenital adrenal hyperplasia),
hyperprolactinemia (prolactinoma, phenothiazines, narcotics, and other medications), hyperthyroidism, hypothyroidism, hypopituitarism, pituitary adenoma, Cushing syndrome, hypothalamic hypogonadism (eating disorder, athletic triad, stress) |
|
|
Secondary Amenorrhea : Medications causes
|
Hormonal, cytotoxic, others
|
|
|
Secondary Amenorrhea : Uterine outflow tract abnormalities causes
|
Surgery
|
|
|
Abnormal Bleeding: Structural: causes
|
Uterine fibroids
endometrial or endocervical polyp, cervical cancer, endometrial hyperplasia, endometrial cancer |
|
|
Abnormal Bleeding: Hormonal: causes
|
Chronic anovulation,
hypothyroidism, waning ovarian function, estrogen secreting tumors |
|
|
Abnormal Bleeding: Coagulopathies: causes
|
Thrombocytopenia, platelet dysfunction
|
|
|
Define: progesterone challenge
|
involves administration of oral medroxyprogesterone for 10 days and watching for the expected "withdrawal bleed" after completion.
Women who bleed have normal estrogen levels and are likely to have chronic anovulation, most often due to PCOS. Women who fail to have a withdrawal bleed are suspected to have low levels of estrogen, and amenorrhea may be due to anovulation and failure of the hypothalamic-pituitary axis. |
|
|
Women with chronic anovulation are at risk for what?
|
Women with chronic anovulation are at risk for endometrial hyperplasia because of the unopposed estrogens and should be cycled using oral progesterone to induce a monthly withdrawal bleed.
|
|
|
How long is the cycle in a women with polymenorrhea?
|
cycle less than 21 days in length
|
|
|
How long is the interval between cycles in women with oligmenorrhea
|
have an interval greater than 40 days.
|
|
|
menorrhagia: define
|
Women with excessive bleeding in duration or quantity
|
|
|
menometrorrhagia: define
|
Women with bleeding between menses
|
|
|
Define: infertility
|
generally considered when a couple fails to conceive after 1 year of intercourse without contraception
|
|
|
What is the most common cause of infertility?
|
anovulation, which is often related to metabolic abnormalities
|
|
|
Low-risk strains of HPV are associated with
|
genital warts
|
|
|
high-risk strains are associated with
|
cervical cancer
|
|
|
When should pap smears start
|
within 3 years of sexual debut and should continue annually.
|
|
|
Women who are considered to be at low risk for cervical cancer and have had three consecutive normal findings can be screened every
|
2-3 years
|
|
|
who does not require a pap smear?
|
Women who have had a hysterectomy with removal of the cervix for benign disease do not require screening for cervical cancer.
|
|
|
define menopause
|
when a woman has not had a menstrual cycle for 12 consecutive months or when her ovaries have been removed
|
|
|
how long can menopause take?
|
the transition toward menopause can be erratic and prolonged over a 5- to 10-year period.
|
|
|
what is menopause characterized by?
|
characterized by ovarian and endocrine changes that ultimately result in the depletion of primordial oocyte stores and the cessation of ovarian estrogen production.
|
|
|
The average age for menopause in the Western world
|
51.4 years, with a range of 40 to 58 years.
|
|
|
When is estrogen therapy appropriate?
|
estrogen and estrogen-progestin therapy are appropriate for the treatment of vasomotor symptoms and for urogenital atrophy in women who have been appropriately counseled.
|
|
|
When should hormone therapy not be used?
|
Hormone therapy should not be used for the prevention of cardiovascular disease.
|
|
|
What does estrogen therapy increase the risk for in post menopausal women
|
Stroke
|
|
|
What was estrogen therapy decrease the risk for?
|
Estrogen therapy and estrogen-progestin therapy significantly reduce the risk for osteoporotic fractures in postmenopausal women; however, other medications are also effective in this regard.
|
|
|
What is a women most at risk for during menopausal years?
|
The risk for cardiovascular disease increases for women at the time of menopause.
It is estimated that one in eight women aged 45 to 65 years has some form of heart disease. This increases to one in three above the age of 65 years. A woman who has gone through menopause is twice as likely to develop heart disease as a woman of the same age who has not gone through menopause. An early, surgical menopause carries the most risk. |
|
|
Why are women at increased risk for cardiovascular disease during menopausal years?
|
During the premenopausal years, it is thought that estrogen increases levels of high-density lipoprotein (HDL), which promotes the removal of cholesterol from the arteries.
Estrogen also appears to exert a vasodilatory effect on blood vessels. Although women enjoy a protection against cardiovascular disease compared with men during their premenopausal years, with diabetes or increasing age, this protection disappears. |
|
|
A clear link exists between the loss of estrogen production at the time of menopause and the development of _________
|
osteoporesis
|
|
|
With the onset of menopause, bone loss temporarily _________
|
accelerates
women may lose up to 5% of their bone mass per year over the next 5 years. About 20% of white women aged 50 years or older have osteoporosis; this number increases to 52% over the age of 80 years. Up to 90% of all hip and spine fractures in white women aged 65 to 84 years can be attributed to osteoporosis. |
|
|
Estrogen therapy is FDA approved for the ________ but not the ________ of osteoporosis
|
Estrogen therapy is FDA approved for the prevention but not the treatment of osteoporosis
Alternate therapies have become more popular since the results of the WHI. These include bisphonates, calcium, and vitamin |
|
|
What does cardiovascular disease include
|
hypertension, coronary artery disease (CAD), cardiomyopathy, stroke, and sudden death
|
|
|
what is the most common cardiovascular disease
|
HTN
|
|
|
what is the greatest risk factor for cardiovascular disease?
|
increasing age
|
|
|
what is usually the first symptom of coronary artery disease in women
|
angina
|
|
|
what is usually the first symptom of coronary artery disease in women
|
myocardial infarction
|
|
|
who is more likely to have congestive heart failure
|
women
|
|
|
what is the 3rd common common cause of death in the US
|
vii. Stroke is the third most common cause of death in the United States (after heart disease and cancer)
|
|
|
Who has strokes more at younger ages?
|
Men
|
|
|
Who has stroke more at older ages?
|
Women
|
|
|
What weight distribution in women is associated with more cardiac events?
|
The pattern of weight distribution is also predictive of coronary events, with more events among women with the apple shape, with a greater central or abdominal girth, than among those with the pear shape, with more weight on the hips and buttocks
|
|
|
What does weight gain do you insulin resistance
|
Greater weight increases insulin resistance and the incidence of diabetes and hypertension.
|
|
|
Define Metabolic Syndrome
|
A subset of obese individuals have the metabolic syndrome, defined in the to include obesity, glucose intolerance, hypertension, and lipid abnormalities.
|
|
|
Define Polycystic Ovary Disease
|
it is characterized by oligo-ovulation or anovulation, evidence of androgen excess, and polycystic ovaries on ultrasound.
Reproductive symptoms include irregular menses, acne, hirsutism, infertility, and increased risk for uterine cancer. Metabolic complications are associated with PCOS, including insulin resistance, diabetes, hypertension, and hyperlipidemia, as are higher rates of CAD. Pharmacologic and lifestyle interventions may improve prognosis, including aggressive management of tobacco use, lipoprotein abnormalities, and hypertension. Regular exercise can also improve glucose and blood pressure control as well as insulin resistance. |
|
|
Breast complaints can include a variety of symptoms, including
|
pain, nipple discharge, and palpable mass.
|
|
|
A solid lesion may be
|
a benign fibroadenoma or a malignant lesion, but again the characteristics of the physical examination cannot reliably distinguish the two.
|
|
|
define: mastalgia
|
Breast pain, mastalgia, is a common complaint but often leads to concern and anxiety about an underlying malignancy.
Although it rarely results from cancer, this must be carefully ruled out by physical examination and mammography as well as a careful follow-up after one or two menstrual cycles to ensure a stable examination. |
|
|
Breast pain is usually
|
cyclic in nature and is thought to be associated with hormonal changes
|
|
|
What is breast pain usually triggered by?
|
It may be triggered by the use of combined hormonal contraceptives or the initiation of estrogen replacement therapy for the treatment of menopausal symptoms. There is some evidence that reducing intake of caffeine can improve symptoms
|
|
|
Nipple Discharge
|
viii. Nipple discharge may be expressed from most women, but spontaneous nipple discharge always requires a further evaluation. Bilateral, guaiac-negative, milky discharge, or galactorrhea, is typically the result of a hormonal abnormality, most often a prolactinoma.
|
|
|
prolactinoma
|
hormonal abnormality that causes spontaneous nipple discharge
Women with a prolactinoma will typically present with amenorrhea. Galactorrhea can also be seen with other pituitary tumors, caused by a hypothalamic or pituitary stalk lesion, chest wall trauma, hypothyroidism, and host of medications. Evaluation should include serum TSH and prolactin levels followed by magnetic resonance imaging of the head if the prolactin level is elevated. |
|
|
papiloma
|
benign lesion
usually unilateral blood discharge malignancy must be carefully excluded |
|
|
mastitis
|
is a breast infection that can occur in the postpartum setting as the result of bacterial infection. It will present as the acute onset of a localized pain and erythema and is associated with fever and influenza-like symptoms.
Mastitis is most often unilateral and is generally caused by Staphylococcus species or Escherichia coli and is treated with oral antibiotics and continued breastfeeding to empty the involved breast. It may be complicated by recurrent mastitis or formation of a breast abscess. Nonlactational infection may also occur as a chronic subareolar infection known as periductal mastitis. This is treated with oral antibiotics and warm soaks. |
|
|
Acute pelvic pain can present over hours or days and may be the result of
|
gynecologic, gastrointestinal, or urinary pathology.
|
|
|
gynecological problems that can cause pelvic pain
|
Gynecologic causes will include complications of pregnancy, acute pelvic infection, or pain related to ovarian processes, including cyst and torsion. The possibility of a ruptured ectopic pregnancy must be quickly assessed by history and pregnancy testing because of its potentially life-threatening course.
|
|
|
Benign prostatic hyperplasia (BPH): define
|
a nonmalignant enlargement of the prostate gland, is a common condition in the aging male patient.
|
|
|
lower urinary tract symptoms can be divided into two categories
|
obstructive voiding symptoms and irritative voiding symptoms
|
|
|
lower urinary tract symptoms: obstructive voiding symptoms
|
1. Hesitancy
2. Slow stream 3. Stop-and-start voiding 4. Sensation of incomplete emptying |
|
|
lower urinary tract symptoms irritative voiding symptoms
|
1. Frequency
2. Nocturia 3. Urgency 4. Urge incontinence |
|
|
Nonurologic causes of lower urinary tract symptoms
|
neurologic disease (MS)
systemic disease (DM) medications excessive fluid intake |
|
|
Prostate growth and the subsequent development of BPH occur under the influence of
|
testosterone and the more metabolically active dihydrotestosterone
|
|
|
Where is testosterone produced
|
testes
|
|
|
What is testosterone converted to?
|
converted to dihydrotestosterone by the action of the enzyme 5α-reductase.
|
|
|
Dihydrotestosterone
|
major intracellular androgen and is believed to be responsible for the development and maintenance of the hyperplastic cell growth characteristic of BPH.
|
|
|
The development of BPH occurs predominantly in the
|
the periurethral prostatic tissue referred to as the transition zone.
Tissue growth in this area leads to the phenomenon of bladder outlet obstruction (BOO), which leads to LUTS. |
|
|
Bladder outlet obstruction occurs as a result of two mechanisms
|
(1) mechanical obstruction, resulting from an increased tissue volume in the periurethral zone of the prostate; and
(2) dynamic obstruction, which is the result of decreased bladder neck relaxation during voiding and increased smooth muscle tone in the bladder neck and prostate gland. |
|
|
What should be included in the history and physical for someone presenting with BPH
|
should include
a detailed medical history, focusing on the patient's urinary symptoms, as well as the patient's past medical history, including comorbid conditions and any previous surgical procedures, general health conditions, and history of alcohol and tobacco use. The assessment of a patient's symptoms can be facilitated with the use of the American Urological Association (AUA) symptom index A general physical examination should also be performed that includes a digital rectal examination (DRE) and a focused neurologic examination Urinalysis, either by dipstick or microscopic examination of urine sediment, is also mandatory to rule out hematuria or evidence of urinary tract infection. |
|
|
What are considered optional exams when assessing for BPH
|
vi. measurement of prostate-specific antigen (PSA) is optional during the initial evaluation. PSA can function as a surrogate for prostate volume measurement in addition to being a screening test for prostate cancer. The National Institutes of Health (NIH)-sponsored study, MTOPS, demonstrated that PSA increases linearly with prostate volume and that PSA greater than 4 ng/mL conveys a 9% risk for requiring surgical therapy for benign disease over a 4.5-year period.
1. Uroflowmetry 2. Measurement of postvoid residual (PVR) 3. Urodynamic evaluation 4. Routine cystoscopic examination |
|
|
What is the first line treatment for BPH?
|
medical management with a combination of a long-acting α blocker and a 5α-reductase inhibitor
|
|
|
when does medical management of BPH begin
|
In general, medical management is initiated for patients with moderate to severe AUA symptom scores.
However, it is important to note that, in the absence of indications for surgery (refractory urinary retention, hydronephrosis with or without renal impairment, recurrent urinary tract infections, recurrent gross hematuria, or bladder calculi), the decision to embark on any course of therapy, medical or otherwise, is principally driven by the degree of bother caused by the patient's symptoms. |
|
|
What class of medication is the most commonly prescribed for BPH
|
α-adrenergic Antagonists
|
|
|
How do α-adrenergic Antagonists work
|
ii. The bladder neck and prostate are richly innervated with α-adrenergic receptors, specifically α1a receptors, which constitute about 70% to 80% of the total number of α receptors in these areas. α1b receptors modulate vascular smooth muscle contraction and are located in the bladder neck and prostate to a lesser degree
|
|
|
what are examples of α-adrenergic Antagonists
|
Doxazosin, terazosin, tamsulosin, and extended-release alfuzosin
|
|
|
What is a major side effect of α-adrenergic Antagonists
|
orthostatic hypotension, therefore they are given at night.
|
|
|
How much and how long of Doxazosin do you need to reach maximal effect
|
4 mg within 1-2 weeks
|
|
|
How much and how long of terazosin do you need to reach maximal effect
|
5 mg within 3-6 weeks
|
|
|
Tamsulosin
|
selective α1a receptor antagonist with a long half-life. It has a significantly lower degree of nonspecific α-receptor binding compared with other α-receptor antagonists. Therefore, side effects such as postural hypotension and dizziness are less common. This drug does not appreciably affect blood pressure in hypertensive or normotensive patients. Maximal response is usually seen within 1 to 2 weeks of the initiation of therapy
|
|
|
5α-reductase Inhibition: two types
|
(Finasteride and Dutasteride)
|
|
|
5α-reductase Inhibition: how does it work
|
Finasteride and dutasteride block the intracellular conversion of testosterone to 5-dihydrotestosterone by inhibiting the action of the enzyme 5α-reductase.
This results in an approximate 18% to 25% reduction in prostate gland size over 6 to 12 months. It is most effective in reducing symptoms and preventing disease progression in patients with large prostate glands (>40 mL), although recent evidence suggests that symptomatic improvement and stabilization of disease progression may occur in treated men with prostatic size down to 30 mL. |
|
|
5α-reductase Inhibition: works best with prostates that are ______ ML
|
> 40 ML, large prostates
|
|
|
When is the initial response of 5α-reductase Inhibition seen?
|
6 months with maximal results seen in 12-18 months
|
|
|
5α-reductase Inhibitors (Finasteride and dutasteride) reduce serum PSA by
|
50%
This must be taken into consideration when interpreting PSA values in men taking these agents. After 6 months of therapy, the effective PSA level in a patient taking finasteride or dutasteride may be calculated by multiplying the measured PSA by 2. |
|
|
What is the gold standard surgical treatment for BPH
|
transurethral resection of the prostate (TURP)
|
|
|
Transurethral microwave thermotherapy (TUMT)
|
one of the most widely studied minimally invasive methods of treating patients with symptomatic BPH. Catheter-mounted transducers use microwave energy (30 to 300 Hz) to heat prostatic tissue, resulting in coagulative necrosis and shrinkage of the prostate gland.
The subsequent reduction in prostate transition zone volume results in an improvement in flow rates and symptom scores. |
|
|
Transurethral needle ablation (TUNA)
|
uses low-level radio frequency energy to effect similar changes within the prostate gland. Other therapies currently available or in development include interstitial lasers and high-intensity focused ultrasound.
|
|
|
DEFINE: TURP
|
TURP remains the gold standard for the surgical management of symptomatic BPH. This procedure involves endoscopic removal of periurethral prostate tissue.
|
|
|
DEFINE: Transurethral incision of the prostate (TUIP)
|
another more limited surgical procedure consisting of incision of the bladder neck and proximal prostatic urethra. Although more invasive than the heat-based therapies, in properly selected patients (i.e., those with prostate glands less than 30 g in size), success rates approach those seen following TURP. Morbidity following TUIP is significantly less than that following TURP, but long-term durability of symptom relief is less than that seen with TURP.
|
|
|
Open surgical enucleation
|
simple prostatectomy, is reserved for patients with very large glands. Success rates are high following this approach; however, the rate of complications following open surgical resection is highest of all the traditional surgical approaches
|
|
|
what is the most common urologic diagnosis in men less than 50 years old
|
prostatitis
|
|
|
Acute Bacterial Prostatitis
|
Acute bacterial prostatitis is a relatively uncommon serious systemic illness requiring aggressive treatment with intravenous antibiotics.
|
|
|
Acute Bacterial Prostatitis: presentation
|
Patients typically present with fevers, chills, dysuria, and perineal and low back pain.
|
|
|
Acute Bacterial Prostatitis: examination
|
Physical examination may reveal a distended bladder, and DRE usually reveals a warm, boggy, and tender prostate.
|
|
|
Acute Bacterial Prostatitis: rectal examination
|
Rectal examination should be performed with caution to minimize the risk for inducing bacteremia as a result of overaggressive manipulation of the gland.
Some urologists recommend deferring a rectal examination if the clinical presentation is highly suggestive of acute prostatitis. |
|
|
how long should patients with acute bacterial prostatis be treated
|
30 days
|
|
|
what class of antibiotics should be used with acute bacterial prostatitis
|
Fluoroquinolones are recommended because they achieve excellent tissue levels within prostate tissue. Although bacterial persistence or conversion to chronic bacterial prostatitis is low, follow-up urine cultures should be obtained to document clearance of the infection.
|
|
|
Define: Chronic Bacterial Prostatitis
|
Chronic bacterial prostatitis is associated with inflammation of the prostate gland and recurrent urinary tract infections with bacteria localized to the prostate through standardized localization testing.
|
|
|
Chronic bacterial prostatis: physical examination
|
Physical examination may reveal abdominal tenderness, testicular or epididymal tenderness, prostate tenderness, or tenderness associated with DRE. The prostate is often normal to palpation, although it may be enlarged secondary to concomitant BPH.
|
|
|
Testing for chronic bacterial prostatis
|
Traditional testing of the urine in this patient population is accomplished by evaluation of urine in the following manner.
The first voided urine (VB-1) is collected, followed by collection of midstream urine (VB-2). Following this, a DRE is performed, and the prostate is massaged. Expressed prostatic secretions (EPS) are then collected. The patient is then asked to void again, and the post-prostatic massage urine (VB-3) is collected. |
|
|
How is chronic prostatis diagnosed
|
Chronic bacterial prostatitis is diagnosed when there are 10 times the number of white blood cells in the EPS or VB-3 relative to the VB-1 or VB-2.
Alternatively, culture of the EPS or VB-3 must grow 10-fold more organisms than the VB-1 or VB-2. One may also compare preprostatic and post-prostatic massage urine for the presence of white blood cells and uropathogenic organisms. Although these measures are commonly described for the accurate diagnosis of prostatitis, a presumptive diagnosis is often made based on clinical symptoms, EPS, and urinalysis findings. |
|
|
Chronic prostatis treatment
|
Treatment involves a 4- to 8-week course of antimicrobial therapy.
Broad-spectrum antibiotics such as trimethoprim-sulfamethoxazole (TMP-SMX) or a fluoroquinolone are indicated for the treatment of chronic bacterial prostatitis and must be tailored to the suspected pathogen. Studies have shown excellent tissue levels of these drugs within the prostate. For patients who have relapsing infections, long-term suppressive therapy may be indicated, whereas patients who have recurrent infections with different organisms are best treated with low-dose prophylactic antibiotics. |
|
|
Define: impotence
|
a condition defined by inability to attain or maintain adequate penile rigidity sufficient for intercourse.
|
|
|
What is the most common cause or erectile dysfunction in the united states
|
impotence
|
|
|
What are important predictors of the onset of erectile dysfunction
|
Age and physical health are the most important predictors of the onset of ED
|
|
|
What is an important lifestyle variable in controlling erectile dysfunction
|
smoking
|
|
|
Does hormones correlate with erectile dysfunction
|
ED did not correlate with male hormone levels.
|
|
|
What is the most common cause for erectile dysfunction?
|
The anatomic site now believed to be the most common cause of ED is the neuromuscular junction, where the cavernosal nerves meet the smooth muscle and endothelium of the deep cavernous penile arteries.
This is where NO and cGMP play a critical role in regulating penile blood flow. This so-called endothelial dysfunction may be an early tipoff of evolving systemic arterial disease. |
|
|
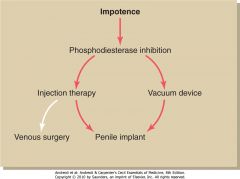
available therapies for ED include
|
oral PDE-5 inhibitors,
intraurethral alprostadil, intracavernous vasoactive injection therapy, vacuum constriction devices, and penile prosthesis implantation. |
|
|
A stepwise treatment approach is adopted, starting with oral agents and progressing to more invasive therapeutic interventions as indicated
|
|
|
|
When is patient referral necessary for erectile dysfunction
|
Patient referral is primarily based on failure of specific medical therapy as well as the need or desire for specialized diagnostic testing and management.
v. As a result, most prescriptions for oral PDE-5 inhibitors are written by primary care providers, and specialized diagnostics such as Doppler ultrasound of the penile arteries and nocturnal penile tumescence (NPT) testing are used by urologists to work up select cases. |
|
|
Current medical therapy of erectile dysfunction is based on inhibition of
|
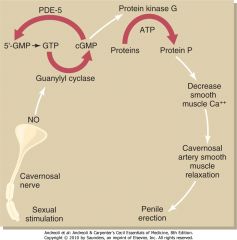
PDE-5.
|
|
|
What medications competitively inhibit PDE-5 breakdown of cGMP by binding to the catalytic domain of PDE-5 to aid in erectile dysfunction
|
Sildenafil, vardenafil, and tadalafil
|
|
|
What is the first line therapy for erectile dysfunction?
|
PDE-5 inhibition
|
|
|
How are PDE-5 inhibitors metabolized
|
hepatically
|
|
|
What medications should phosphodiesterase inhibitors should not be used concurrently with
|
nitrate medications because a large (>25 mm Hg) synergistic drop in blood pressure is observed in many patients.
|
|
|
PHARMACOLOGIC INJECTION THERAPY for erectile dysfunction
|
Several vasoactive agents can be safely injected directly into the corpora cavernosa to produce penile erection.
|
|
|
Commonly used vasoactive agent injectable for erectile dysfunction
|
Commonly used agents include PGE1, papaverine, and phentolamine
|
|
|
Risks for injection therapy for erectile dysfunction
|
Injection therapy has two principal risks, priapism and corporal scarring causing penile curvature.
Priapism has been reported to occur in 1% to 4% of patients. |
|
|
INTRAURETHRAL DRUG THERAPY: erectile dysfunction
|
i. PGE1 can be inserted into the urethra using a pellet applicator. This method of delivery assumes substantial venous communications between the corpus spongiosum surrounding the urethra and the corpus cavernosum. As a consequence, the technique is considerably less effective than intracavernous injection.
|
|
|
VACUUM CONSTRICTION DEVICES: erectile dysfunction
|
i. These devices enclose the penis in a plastic tube with an airtight seal at the penile base. Air is pumped out of the cylinder, creating a vacuum. Blood flows into the corporal bodies, leading to penile erection. A constriction band remains on the base of the penis to maintain erection. Simultaneous use of a vacuum device and a phosphodiesterase inhibitor is safe. Many patients couple the two techniques to achieve satisfactory results.
|
|
|
PENILE PROSTHESIS: erectile dysfunction
|
i. A penile prosthesis is implanted in the operating room. Two general types of devices can be implanted: semirigid and inflatable. Most patients prefer the inflatable devices because they provide a more natural erection when inflated and a flaccid penis when deflated. Although more invasive than the other techniques, a penile prosthesis is the most effective long-term option for impotence treatment. Ninety percent of patients and partners are satisfied with the result.
|
|
|
What is the most common cancer in men?
|
Prostate cancer
|
|
|
What age period is it unusual to diagnosis prostate cancer?
|
Clinical diagnosis of prostate cancer is unusual before the latter half of the fifth decade of life but increases progressively thereafter.
|
|
|
What tests have play a role in the early diagnosis of prostate cancer?
|
Both the DRE and serum PSA determination have a role in the early diagnosis of prostate cancer.
|
|
|
Where does prostate cancer typically develop first?
|
Prostate cancer typically arises from the peripheral portion of the prostate, which can be palpated on DRE.
Induration or nodularity of the prostate on DRE should be considered suspicious for prostate cancer. |
|
|
What is PSA
|
is a protein produced by both benign and malignant prostate cells.
|
|
|
Serum PSA may be elevated in the face of
|
prostate enlargement, inflammation, or cancer.
|
|
|
Causes of Increased Prostate-Specific Antigen
|
Benign prostatic hyperplasia
Prostatitis Urinary tract infection Prostatic trauma (urethral catheterization or prostatic massage) Carcinoma |
|
|
What happens to PSA with age?
|
Probably because of progressive enlargement in prostate size, serum PSA values increase as men age.
|
|
|
Normal value of PSA
|
The historical view of a value of less than 4 ng/mL as a "normal" PSA has been abandoned with the recognition that PSA represents a continuum of risk with no lower threshold.
|
|
|
PSA velocity
|
The comparative rate of change for PSA over time, sometimes termed PSA velocity, can be informative. In general, a change in PSA of greater than 0.75 ng/mL is considered worrisome and may prompt a prostate biopsy.
|
|
|
A change in PSA of greater than ______ is considered worrisome
|
In general, a change in PSA of greater than 0.75 ng/mL is considered worrisome and may prompt a prostate biopsy.
|
|
|
Whenever prostate cancer is suspected, either because of an abnormality in DRE or PSA rise what is performed?
|
A biopsy
|
|
|
What is used to guide prostate biopsy?
|
TRUS imaging of the prostate is used to guide prostate biopsy
|
|
|
Transrectal cores of prostate tissue
|
Office based prostate biopsy method
This is an office-based procedure, and local infiltration of lidocaine (Xylocaine) around the prostate minimizes discomfort. Usually 12 or more tissue cores are taken systematically from the entire prostate. |
|
|
In patients with high-grade tumors or a substantially elevated PSA what imaging is likely to be ordered?
|
a bone scan is indicated because bone is the most common site of distant spread. Soft tissue metastasis is unusual in the face of a normal bone scan.
|
|
|
Treatment Options for Localized Prostate Cancer
|
Radical prostatectomy (robotic or open)
Brachytherapy (iodine-125, etc., seeds) External-beam irradiation Cryotherapy Hormonal therapy Active surveillance |
|
|
Localized prostate cancer and surveillance (who)
|
In men with less than 10-year life expectancy otherwise, active treatment often is unnecessary.
The risk for progression and death within 10 years is sufficiently low that observation alone is appropriate. Increasingly, some men with a greater than 10-year life expectancy but a tumor with apparently favorable features pursue a program of active surveillance. |
|
|
Localized prostate cancer surveillance guidelines
|
In general, active surveillance should be restricted to men with a PSA of less than 10 ng/mL, no palpable prostate nodules, a Gleason sum of 6 or less, and fewer than 2 or 3 positive biopsy cores.
Typically, repeat prostate biopsy is recommended every 1 to 3 years in men on active surveillance to ensure that higher-volume or higher-grade tumor is not evident. PSA and DRE are performed every 6 months. The underlying premise of active surveillance (i.e., that treatment can be safely deferred until there is some evidence of disease progression) is unproved, but it is known that many men with favorable features of the primary tumor do not develop progressive disease in their lifetime. |
|
|
For men with a greater than 10-year life expectancy otherwise, curative therapy usually is indicated, this is a ______________
|
radical prostatectomy
|
|
|
Radical prostatectomy
|
Surgical removal of the prostate (radical prostatectomy) is the treatment with the most proven ability for long-term cure of prostate cancer.
|
|
|
What are the drawbacks of a radical prostatectomy?
|
Significant incontinence occurs in only around 2% of men, but up to 10% may have at least some degree of mild stress incontinence
ii. The cavernosal nerves, which are responsible for dilation of the blood vessels that lead to penile tumescence, lie immediately adjacent to the prostate. Dissection of these nerves from the prostate (nerve-sparing radical prostatectomy) is appropriate in patients with tumors localized to the prostate. The success of nerve-sparing prostatectomy is related to patient age and preoperative erectile function. Preservation of potency can be achieved in up to 60% to 80% of patients. |
|
|
PSA after a radical prostatectomy
|
No measurable PSA is produced from any source other than prostate cells.
Metastatic foci of cancer continue to produce PSA, so an undetectable value is an excellent prognostic sign. Furthermore, an increase in PSA to a detectable range precedes other signs or symptoms of prostate cancer recurrence after radical prostatectomy almost 99% of the time. Thus, PSA is an extremely sensitive and specific marker for following men after radical prostatectomy. PSA values greater than 0.2 ng/mL are considered diagnostic of tumor recurrence after radical prostatectomy. |
|
|
Radiation therapy for prostate cancer
|
Radiation therapy is the primary alternative to surgery for localized prostate cancer.
Radiation can be administered by external-beam therapy using intensity-modulated radiation treatment (IMRT) or using proton-beam therapy. No significant difference in outcomes has been shown between proton-beam treatment and conventional radiation. Each is delivered over a 7- to 8-week time frame. |
|
|
Side effects of prostate cancer
|
Side effects of radiation treatment occur most commonly because of radiation damage to the bladder or rectum. Patients may experience frequency of voiding or bowel movements or blood in the urine or stool. ED appears to occur at about the same frequency as after surgical treatments
|
|
|
What is the primary form of treatment for patients with advanced or metastatic carcinoma of the prostate.
|
endocrine manipulation
|
|
|
what is the goal of endocrine manipulation in the treatment of advanced or metastatic prostate cancer?
|
The goal of therapy is to deprive the prostate cancer cells of serum androgens. This can be accomplished by either surgical or medical castration
|
|
|
Surgical orchiectomy
|
surgical removal of both testes, the source of testosterone production.
|
|
|
Luteinizing hormone-releasing hormone (LHRH) analogues for the treatment of advanced or metastatic prostate cancer
|
administered by a slow-release depot injection, with formulations lasting from 3 to 12 months.
These drugs have the paradoxical effect of decreasing serum luteinizing hormone release from the pituitary gland and, consequently, diminishing testosterone production from the testis. |
|
|
Effect of decreased testosterone levels as an effect of Surgical orchiectomy and Luteinizing hormone-releasing hormone (LHRH) analogue injection for the treatment of advanced or metastatic prostate cancer.
|
Testosterone declines to castrate values within a few days after surgical orchiectomy and a few weeks after administration of an LHRH analogue.
In response to androgen deprivation, prostate cancer typically undergoes rapid regression. This is manifested by a decrease in prostate size, improvement in any disease symptoms such as bone pain, and a rapid decline in serum PSA. The duration of response varies but is usually on the order of a couple of years for patients who present with metastatic disease. |
|
|
Long-Term Side Effects of Androgen Deprivation Therapy
|
Hot flashes
Loss of libido Impotence Osteoporosis Decreased facial hair Loss of muscle mass Weight gain |
|
|
Antiandrogens for the treatment of advanced or metastatic prostate cancer
|
Antiandrogens may also be used in hormonal therapy of patients with prostate cancer.
These oral medications exert their effect by blocking the metabolism of androgens at the cellular level rather than by decreasing serum values. |
|
|
Squamous cell carcinoma of the penis: prevalance
|
uncommon tumor in the United States and the rest of the developed world, with a rate of less than 1 case per 100,000 men and an estimated 1470 cases in the United States for 2005.
|
|
|
Penile carcinoma, who is it diagnosed mostly in?
|
It is diagnosed almost exclusively in uncircumcised men
Chronic irritation and inflammation are key etiologic factors because most men have poor hygiene leading to phimosis of the foreskin. |
|
|
How does penile carcinoma present?
|
Squamous cell carcinoma typically presents as a painless, nonindurated, ulcerated mass involving the glans penis and coronal sulcus.
Infection of the primary lesion is common and may produce foul-smelling, purulent discharge and reactive inguinal lymphadenopathy. Delay in diagnosis is common because patients often do not seek immediate treatment secondary to fear and embarrassment, whereas prolonged treatment with antibiotics may delay confirmatory biopsy of the lesion. |
|
|
imaging studies and penile cancer
|
Imaging studies are not routinely recommended because physical examination has proved the most accurate predictor of tumor stage.
|
|
|
How to diagnose penile cancer
|
A diagnosis of carcinoma of the penis is confirmed by histologic evaluation of an excisional biopsy.
|
|
|
partial penectomy
|
The classic operation for squamous cell carcinoma of the penis is partial penectomy with a 2-cm negative margin.
If the tumor is confined to the distal penis, a sufficient length of proximal penile shaft can be preserved so that the patient can still void in a standing position. Larger tumors that invade the more proximal penile shaft require total penectomy. The entire corpora cavernosa are excised back to the ischial tuberosity. A perineal urethrostomy is created that allows voiding in a sitting position. |
|
|
what is the most common solid malignancy in men
|
Testicular tumors are the most common solid malignancy in men aged 15 to 34 years. The incidence of testis cancer appears to be increasing over the past 25 years.
|
|
|
what is one well accepted risk factor for testicular cancer
|
Cryptorchidism (undescended testicle) is a well-accepted risk factor for subsequent development of carcinoma
|
|
|
what is the most common presenting symptom of testicular cancer?
|
The most common presenting sign or symptom of testis cancer is a firm, painless mass arising from the testis.
|
|
|
what is the diagnostic test of testicular cancer
|
Scrotal ultrasonography is diagnostic because testis cancer is usually distinguishable from benign scrotal disease because of the clear involvement of the testicular parenchyma rather than the paratesticular tissues.
|
|
|
what are signs and symptoms of advanced testicular cancer
|
Signs and symptoms of advanced disease include cough, gastrointestinal symptoms (mass), back pain (retroperitoneal metastasis), neurologic symptoms (brain metastasis), lower extremity swelling (iliac or inferior vena cava thrombus), and supraclavicular lymphadenopathy.
|
|
|
define: varicocele
|
Varicoceles are classically described as abnormal dilation of the veins of the pampiniform plexus.
|
|
|
what does physical examination of a Varicocele show
|
Physical examination can reveal the classic "bag of worms": testicular atrophy and tender scrotal contents.
|
|
|
what does semen analysis in a man with a varicocele show?
|
Semen analysis reveals multiple abnormalities reflecting a characteristic "stress pattern," although this is not pathognomonic
|
|
|
how can you diagnose a varicocele?
|
The diagnosis of varicocele remains a clinical one, although scrotal ultrasound with Doppler is helpful in certain situations.
The presence of two or three veins with diameter larger than 3 mm and retrograde flow with Valsalva maneuver is consistent with clinical varicocele. |
|
|
pathophysiology with a varicocele
|
Regardless, there is dilation of the internal spermatic vein and transmission of increased hydrostatic pressure across dysfunctional venous valves.
Stasis of blood in the venous system disturbs countercurrent heat exchange responsible for maintaining testicular temperature and results in testicular parenchymal damage and impaired spermatogenesis. Because of anatomic considerations, varicoceles are more commonly left sided. |
|
|
What are some indications of surgical correction of a varicocele
|
Indications for surgical correction of a clinical varicocele include male factor infertility, testicular atrophy in adolescents with ipsilateral varicocele, and intractable pain attributed to the varicocele.
|
|
|
Acute epididymitis
|
clinical syndrome that presents with fever, acute scrotal pain, and swelling as a result of inflammation and infection of the epididymis.
Pathophysiologically, epididymitis is caused by retrograde bacterial spread from the bladder or urethra. |
|
|
cause of epididymitis in men younger than 35
|
the most common causes are organisms associated with urethritis, namely gonococcus and Chlamydia trachomatis.
|
|
|
most common cause of epididymitis in older men
|
Escherichia coli and other coliform bacteria are the causative organisms, usually in association with lower urinary tract infection associated with symptoms of bladder outlet obstruction.
|
|
|
what is the most important consideration in diagnosing acute epididymitis
|
The most important consideration in diagnosing acute epididymitis is differentiating this disease from acute testicular torsion.
|
|
|
physical exam on acute epididymitis
|
Physical examination can be nonspecific, although focal epididymal swelling and tenderness are suggestive, and the presence of white cells in the urine or urethral swab is indicative of an infectious etiology.
|
|
|
how to differentiate between epididymitis and testicular torsion
|
Scrotal ultrasound with Doppler flow can be extremely helpful in differentiating acute epididymitis from torsion in difficult cases
|
|
|
treatment for epididymitis
|
Treatment is generally supportive, including narcotic analgesics, NSAIDs, scrotal support with an athletic supporter, cold ice packs, and targeted antimicrobial therapy.
In general, patients younger than 35 years should be treated with ceftriaxone (Rocephin) and doxycycline, or a single dose of azithromycin (Zithromax). Older patients are empirically treated with a fluoroquinolone or TMP-SMX for 2 to 4 weeks. |
|
|
define: hydrocele
|
a serous fluid collection within the parietal and visceral layers of the tunica vaginalis of the scrotum.
Hydroceles may surround the testicle or the testicle and spermatic cord, or communicate with the peritoneal cavity through a patent processus vaginalis. These communicating hydroceles are uncommon in the adult population and are more commonly identified in the pediatric age group in association with an indirect hernia. |
|
|
patients with hydroceles will present with
|
Patients usually present to the physician with complaints of heaviness in the scrotum, scrotal pain, and an enlarging scrotal mass
|
|
|
hydrocele: diagnosis
|
Diagnosis is easily made with physical examination and transillumination of the hydrocele
|
|
|
hydrocele: pathophysiology
|
Hydroceles are caused by increased secretion or decreased reabsorption of serous fluid by the tunica vaginalis.
|
|
|
hydrocele: causes
|
Infection, trauma, neoplastic disease, and lymphatic disease are causative in most adults, whereas the remainder of cases are idiopathic.
|
|
|
hydrocele: treatment
|
surgery
|
|
|
what is considered a true urologic emergency
|
testicular torsion
|
|
|
define testicular torsion
|
The testicular blood supply is through the testicular artery (aorta), the vasal artery (inferior vesicle artery), and the cremasteric artery (inferior epigastric artery).
All three vessels are transmitted to the testicle through the spermatic cord. Torsion of the spermatic cord impairs arterial inflow as well as venous outflow producing the characteristic symptoms of acute scrotal pain, swelling, and nausea and vomiting. |
|
|
If detorsion of testicular torsion is not performed within __________________, testicular infarction and hemorrhagic necrosis are likely to occur.
|
6 to 8 hours
|
|
|
age range for testicular torsion
|
Typically, patients are younger than 21 years, although testicular torsion can occur into early adulthood
|
|
|
symptoms of testicular torsion
|
Symptoms usually include the acute onset of testicular and scrotal pain, scrotal swelling, and nausea and vomiting.
Ecchymosis and involvement of the scrotal skin occur in more advanced cases, but the testis has infracted by that point. |
|
|
what imaging study is helpful in differentiating testicular torsion from other cases of acute scrotom
|
Doppler ultrasonography is extremely useful in differentiating testicular torsion from other causes of the acute scrotum, such as acute epididymitis, torsion of the appendix testis, and trauma.
|
|
|
testicular torsion: treatment
|
surgery
|

