![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
79 Cards in this Set
- Front
- Back
|
what is neutropenia?
|
low number of neutrophils
|
|
|
what causes neutropenia
|
bone marrow suppression: tumors, granulomoatous infection of the marrow, infeefective hematopoiesis, genetics
destruction of neutrophils: immune disorders SLE, reheumatodi arthritis drug reaction, splenomegaly(sequesters blood cells causing pancytopenia increased peripheral utilization: overwhelming infection |
|
|
what is reactive leukocytosis?
|
high white count
|
|
|
what causes reactive leukocytosis
|
infections, tissue damage, allergic disorders, malignancy, autoimmune disorders, inflammatory bowel disease
leukemoid reaction |
|
|
what is a a leukemoid reaction
|
a type of reactive leukocytosis in which there is a very high white count with circultatin immatrue white cells, simulateing a myeloid leukemia
|
|
|
how can you tell the difference btw a leukemoid reaction and a leukemia?
|
mostly matrue neutrophils in leukemoid reaction no blasts or nucleated RBCs
|
|
|
what causes a leukomoid reaction
|
perforrated abdominal viscera(peptic ulcer)
infarcted abdominal organs |
|
|
what 3 things found on peripheral smear are indicative of leukemoid reaction?
|
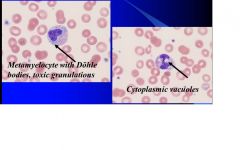
metamyelocytes
dohle bodies cytoplasmic vacuoles. |
|
|
atypical lymphocites on CBC in a young adult with sore throat and swollen lymph nodes
|
infectious mononucleosis
|
|
|
where are B cells usually
|
in the lymphnodes
|
|
|
where are T cells usually
|
circulating in peripheral blood
|
|
|
what are the nature of atypica lymphocites in a person with mononucleosis
|
reactive t cells
|
|
|
what are the two types of leukemias?
|
myeloid-contains all but the white blood cells:granulocytes, megakaryocytes, and erythroid cells
lympoid: neoplastic proliferation of lymphocytes. |
|
|
what does the white WBC count have to be in leukemia?
|
it can be anything high, normal, or even low.
|
|
|
what is the cause of neutrophilic leukocytosis
|
bacterial infection, or tissue necrosis
|
|
|
what is the cause of eosinophilic leukocytosis
|
allergy, drug reaction, parasitic infection, vascular disorder
|
|
|
what is the cause of basophilic leukocytosis
|
rare usually indicates a myloproliferative disorder
|
|
|
what is the cuase of a lymphocyctic luekocytosis
|
viral, fungal infections or bordetella pertussis (whooping cough)
|
|
|
what does the marker CD34 indicate
|
a hematopoetic stem cell
|
|
|
what does IL 5 stimulate a myloid progenitor to become?
|
eosinophil
|
|
|
what does thrombopoiten stimulate teh myloid progenitor to become?
|
basophil, megakaryocyte, erythroid.
|
|
|
what does GM CSF stimulate a myloid progenitor to become?
|
neutrophil or monocyte.
|
|
|
what is the clinical presentration of acute leukemia
|
short duration of symptoms
aggressive clinical course |
|
|
what is the clincial presentation of chronic leukemia
|
insidious onset may be discovered by cbc
hepatosplenomegally |
|
|
what are the characteristics of acute myeloid leukemia
|
mainly in adults
originates from stem cells this means there are several subtypes based on which stem cell is proliferating cytopenia can result from bonemarrow loss examples promelocytic, myelocytice, monocytic |
|
|
what are the clinical presentation of AML
|
ulceration of mucous membranes
fever DIC myeloid sarcomas:soft tissue masses of imature myeloid cells anemia, thrombocytopenia blasts in peripheral blood |
|
|
what is gum hypertrophy a symptom of
|
AML monoblastic type
|
|
|
what can be found in peripheral blood smear for AML
|
myeloblasts
auer rods nucleated RBCs |
|
|
what does auer rods do?
|
confirms blasts as myeloid
|
|
|
what is the percent myeloblasts in the the bone marrow that indicates leukemia
|
greater than 20%
|
|
|
what is cytochemistry used for?
|
to separate AML and ALL
positive in AML negative in ALL |
|
|
what does a myeloperoxidase(MPO) stain indicate
|
neutrophilic lineage
|
|
|
what does a sudan black B(SBB) stain indicate
|
neutrophilic liineage
|
|
|
what does a nonspecific esterase (NSE) stain indicate
|
monocytic lineage
|
|
|
what are the three main genetic findings found in AML with recurrent cytogentetic abnormality
|
t(8:21) good response to treatment
t(15;17)all trans retinoic acids works inv(16) better remmision with cytarabine |
|
|
what does myeloid sarcoma indicate
|
AML
|
|
|
what are some characteristics of acute promyelocytic leukemia
|
numerous Auer rods
best treated with all trans retinoic acid strong association with DIC associated with t(15;17) and (q22;q21) |
|
|
what are the characteristics of Acute lymphoblastic leukemia
|
more common in children
more common in whites pallor, weakness, anemia petechiae, mucosal bleeding bone pain fever(50%) lymphadenopathy or hepatosplenomegaly anterior mediastinal mass blasts in the periperal blood. |
|
|
what is the diagnostic percentage of blasts in ALL
|
25%
|
|
|
what is an easy and accurate way to diagnose ALL
|
the use of TdT assay and panel of monoclonal antibodies for T and B cell antigens
|
|
|
what are the catagoies in ALL
|
T cell
B cell |
|
|
what is the differecne btw leukemia and lymphoma
|
leukemia has malignacy circulating
lympha no blasts in peripheral blood |
|
|
what are the characteristics of chronic lymphocycitc leukemia
|
most common leukemia
mainly in older people 20% asymptomatic 50% splenomegaly lymphadenopathy Elevated WBC |
|
|
how is CLL staged
|
absence of anemia and thrombocytopenia is stage 1 or 2
presence of anemia only is stage 3 presence of both is stage 4 |
|
|
what is an implication of B cell neoplasms in CLL
|
anemai can be brought on by hemolysis caused by antibodies.
B cell neoplasms can make a variety of antibodies that could cause conditions that bring the patient in looking like an autoimmune issue. |
|
|
what does CLL look like
|
cracked earth or soccer ball
hyperdense nuclear pattern |
|
|
how is CLL diagnosed
|
lymphocytes express both CD5(tcell marker) and CD 20 and 23 (bcell marker) along with low level expression of surface IG(usually IgM)
|
|
|
when sequenced what does unmutated CLL mean for prognosis
|
unmuated CLL is more aggressive
|
|
|
what are the markers in CLL
|
ZAP-70:positive in unmuated CLL
CD 38: if greater than 30% poor prognosis Del 17p or 11q22.3: poorer survival del 13q: good prognosis trisomy 12: responsive to anti-CD20 medications |
|
|
what are the two most common transformation in CLL that make it more aggressive
|
prolymphcytic
Richter syndrome |
|
|
what is the presentation of prolymphocitic transformation in CLL
|
gradual increase in circulating prolymphocytes seen in peripheral blood
|
|
|
what is the presentatino of richter syndrome
|
development of rapidly progressive lymphoma
|
|
|
what are the characteristics of hairy cell leukemia
|
rare
memory b cell neoplasm middle aged male pancytopenia, enlarged spleen, dry tap on bone marrow aspiration hairy cells seen on periperal blood smear. |
|
|
what is the marker for hairy cell
|
pos CD19, CD20, 11c
red cell lakes |
|
|
what are some key differences btw myelodysplasia and myeloproliferative
|
myelodysplasia:hypercellular bone marrow, periperal cytropenia, ineffective hematopoiesis, dysplasia, no splenomegaly
myeloproliferative: hyerpcellular bone marrow with peripheral hypercellularity., effective hematopoiesis, no dyspolasia, splenomegally may be massive |
|
|
what are some characteristics of myelodysplasia
|
idiopthic or primary: age 50+ develps insidiously
therapy related MDS(secondary): complication of previous drug or radiation therapy, arising 2-8 years after treatment. all can progress to AML |
|
|
what is refractory anemia?
|
does not respond to iron suppliments
|
|
|
what is the diagnositc percentage of myeloblasts in the bonemarrow for MDS
|
less than 20% because greater than 20% would be AML
|
|
|
what is the worst MDS other than therapy related
|
Refactory anemia with excess blasts
RAEB type II |
|
|
what abnormalites can be used to help diagnose MDS
|
clonal chromosomal abnormaliteis:
monosomy 5, monosomy 7, deletions 5q and 7q, trisomy 8 and deletions of 20q |
|
|
what are the worst prognostic indicators in MDS
|
RAEB II
2-3 cytopenias or pancytopenia cytogenetics with three or more abnormalities or a single abnormality on chromosome 7. |
|
|
what are the various classifications that fall under myeloproliferative neoplasms
|
chronic myelogenous leukemia(CM), BCR-ABL1 positive
chronic neutrophilic leukemia polycythemia vera primary myelofibrosis essential thrombocytosis chronic eosinophilic leukemia mastocytosis |
|
|
what is the definition of MPN
|
clonal stem cell disorder
proliferation in the BM of nonlympohid lineages all the following the in the peripheral blood: myelocytes metamyelocytes bands promyelocytes nucleated reds less than 20% masts classified by periperal blood findings |
|
|
what is characteristic of chronic myelgenous leukemia
|
bone marrow in the blood(excess cells in the periperal blood)
demonstration of philadelphia chromosome t(9:22), (q34;q11) if found can be treated with gleeveck hepatosplenomegally |
|
|
what is the philidelphia chromosome
|
translocation between chromosome 9 and 22 which creates BCR-ABL which is a fusion protien with tyrosine kinase acitvitiy which activates cell division and inhibits apoptosos
|
|
|
what is polycythemia vera
|
marked increase of red blood cells
which causes intense itching espeacially after bathing high risk for bleeding or thrombosis headache diziness, HTN, GI distress red face red hands can lead to splenomegaly can lead to AML but less common |
|
|
what is a normal amount of RBCs in the peripheral blood of a person with Polycemia vers
|
6 million
|
|
|
what is found on CBC of a person with polycemia vera
|
high WBC
high RBCs high platelets high hemoglobin and hematocrit anemia with low MCV due to iron deficiency secondary to chronic GI blood loss |
|
|
how is polycemia vera treated
|
phlebotomy
|
|
|
what is primary myelofibrosis
|
megakaryocyte proliferation
marrow is obliterated and fibrosed |
|
|
how is primary myelofibrosis diagnosed
|
CBC-anemia with elevated WBC and platelet count
leukoerythroblastosis seen on peripheral blood imature RBC and granulocytes tear drop shaped RBCs white bonemarrow |
|
|
what is leukoerythroblastosis?
|
indicates space occupying lesion:fibrosis, metastaic carcinoma, TB granulomas,
aka myelophthisic anemia most commin in primary myelofibrosis |
|
|
what is essential thrombocytosis
|
neplastic proliferation of megakaryocyts and platelets
very high platelt counts 600,000 excess platelets leads to bleeding and thrombosis erythromelalgia=throbbinga nd burning hands and feed due to small vessel occlusion by platelets. |
|
|
how is essential thrombocytosis diagnosed
|
peripheral blood shows a lot of platelets and those platelets are abnormal
|
|
|
what is the most vital thing to know about diagnosis for CML
|
must rule our reactive leukocytosis first and verify philadelphia chromosome
|
|
|
what is the most vital thing to konw about diagnossis for Polycythemia vera
|
rule out secndonary polycythemia
can be caused by smoking, chronic tissue hyposia, high O2, affinity hemoglobinopahty, high erythropoiten level |
|
|
what is needed to know about diagnosis of essential thrombocytosis?
|
must rule out reactive thrombocytosis
|
|
|
what is the jak2 study
|
lab test that detects myeloproliferative disorders
|
|
|
what myeloproliferative disorder is most likely to progress to AML if untreated
|
CML
|

