![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
49 Cards in this Set
- Front
- Back
|
What are the 3 categories of carbohydrate metabolic disorders?
|
1. underproduction/utilization of glucose (disorders of glycogenolysis and gluconeogenesis)
2. overutlization of glucose (hyperinsulinsm) 3. defective insulin action (diabetes) |
|
|
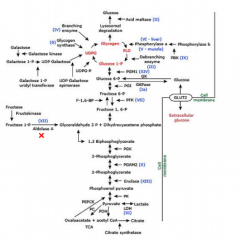
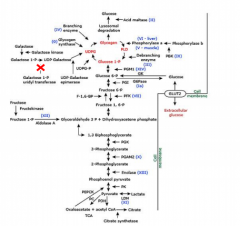
Underproduction of glucose disorders (4 categories)
|
1. glycogenolysis
2. gluconeogenesis 3. inhibition of gluconeogenesis 4. ketotic hypoglycemia |
|
|
Disorders of glycogenolysis
|
glycogen storage diseases (GSDs)
|
|
|
GSD 1
|
von Gierke's disease
1:100,000 incidence no G6Pase from glucose-6-P to glucose Tx: IV dextrose, correct acidosis, frequent 3 hr feeds avoiding lactose/fructose. NG feeds with only glucose formula |
|
|
GSD II
|
Pompe's disease
deficiency of alpha-1,4-glucosidase enzyme (lysosomal acid maltase) -glycogen accumulation in lysosome due to this deficiency, damage to heart, skeletal, muscle (hypotonia), liver, nervous system -1:14,000 - 1:50,000 -Tx: high protein, low carbohydrate, synthetic alpha glucosidase |
|
|
GSD III
|
IIa, c- affect liver, muscles
IIIb, d affect only liver GSD III- deficiency of amylo-1,6 glucosidase or debrancher enzyme -infancy, early childhood- hepatomegally, elevated liver enzymes, ketotic hypoglycemia, hyperlipidemia -adolescent, adult- less prominent liver disease, hypertrophic cardiomyopathy -1:100,000 -myopathy -Tx: discouraging prolonged exercise, high protein diet. synthetic ketone bodies |
|
|
Disorders of gluconeogenesis
|
-fructose 1,6-biphosphatase deficiency
-pyruvate carboxylase deficiency -phosphoenolpyruvate carboxykinase (PEPCK) deficiency -pyruvate dehydrogenase deficiency |
|
|
F 1,6-biphosphatase deficiency
|

-present with irritability, poor feeding neonate, fasting hypoglycemia evolves, lethargy/poor tone, irritability, poor milestones developmental delay, prolonged- abd distension
- fatty liver, 3 carbon molecules cannot be used, shunted to make pyruvate, lactic acid, lactic acidosis, ketoacidosis -Tx: eat frequently, avoid gluconeogenesis, not fasting for long periods, high carb foods, NG feeds, avoid fructose |
|
|
Inhibition of gluconeogenesis by accumulation of metabolic products
|
-galactosemia
-galactokinase deficiency -UDPgalactose epimerase deficiency -hereditary fructose intolerance |
|
|
Hereditary fructose intolerance
|
-aldolase B def- AR
-hepatomegaly, failure to thrive, emesis -avoid fructose. not as severe/deadly as other GSDs |
|
|
Galactosemia
|
-galactose-1-phosphate uridyltransferase (GALT) deficiency. 1:30 to 1:60,000. neonatal screen
-infants develop feeding difficulties, lethargy, hypoglycemia, failure to thrive, jaundice, bleeding, sepsis, shock from infections, delayed development, cataract, ovarian failure Tx: avoid lactose |
|
|
Ketotic hypoglycemia
|
-substrate limited gluconeogenesis, "accelerated starvation"
-0.5-1.0% incidence -dominant in apperance, 1-5 year olds, due to low alanine availability for GN |
|
|
Underproduction of glucose
|
- endocrine hormone deficiencies
-drugs: ethanol, salicylates, beta blockers, pentamidine -other: fatty acid oxidation defects, disorders of ketogenesis, mitochondrial disorders |
|
|
what endocrine deficiencies can lead to underproduction of glucose
|
-GH def
-cortisol, primary addisons, primary adrenal and secondary adrenal -glucagon def (very rare) -insulin deficiency- diabetes |
|
|
How do endocrine hormones respond to hypoglycemia
|
-decr insulin
-incr glucagon -incr epinephrine -incr cortisol -incr GH |
|
|
insulin
|
-insulin decr--> glycogenolysis to produce glucose.
-decreased insuli--> glycagon secretion by direct stimulation in pancreatic alpha cells- further increases hepatic glucose production -insulin normally restrains glucagon secretion |
|
|
glucagon
|
-increased in hypoglycemia
-falling below 65-70 mg/dl -glucagon acts only on liver, increasing glucose production via glycogenolysis, gluconeogenesis from alanine, amino acids, glycerol |
|
|
epinephrine
|
-b-2-adrenergic receptors, stimulates hepatic glycogen breakdown. increases delivery of gluconeogenic substrates from periphery
-inhibits glucose utilization by tissues -via a-2receptors, inhibits insulin secretion -65-70 threshold |
|
|
cortisol and GH
|
last line defenses following insulin decline and increases in glucagon and epinephrine
-limit glucose utilization, enhance hepatic glucose production via gluconeogensis, require intact HPA |
|
|
What are some drugs and substances that cause hypoglycemia?
|
-alcohol
-bactrim (ABx) -beta blockers -haloperidol -insulin -MAO inhibitors -metformin when used with sulfonylureas -pentamidine -quinidine -quinine -sulfonylureas |
|
|
Non ketotic hypoglycemias
|
-fatty acid oxidation disorders
-hyperinsulinism (too much insulin, forced caloric ingestion/infusion, hospital acquired) |
|
|
MCAD
|
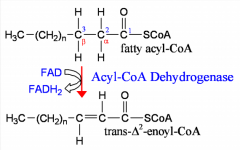
-medium chain acyl CoA dehydrogenase deficiency
-acyl-CoA dehydrogenase catalyzes oxidation of fatty acid moiety of acyl-CoA to produce double bond between carbons 2 & 3. -in mitochondrial matrix -MCAD most potent for inducing hypoglycemia |
|
|
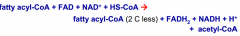
B oxidation
|
|
|
|
What happens during fasting (chemical pathway)
|
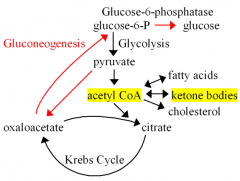
Fasting: oxaloacetate depleted in lever due to gluconeogenesis. This impedes acetyl-CoA entry into Krebs. Then this acetyl CoA in liver mitochondria converted to ketone bodies, acetoacetate, B-hydrobutyrate
|
|
|
MCAD treatment
|
MCAD is AR, prevealent in individuals of northern european caucasian descent.
-treatment is frequent feeds, avoidance of fasting-carnitine supplementation |
|
|
What tumors can lead to hyperinsulinism?
|
1. insulin-secreting tumors-pancreatic
2. non-islet cell, IGF-II secreting tumors 3. myeloma, lymphoma, leukemia 4. metastatic cancers |
|
|
PHHI- pathogenesis
|
persistent hyperinsulinemic hypoglycemia of infancy
-AR mutation in gene encoding K-ATP channel -inactivating mutations reduce open channels, depolarization of beta cells and hypersecretion of insulin -aberrant secretion is diffuse |
|
|
PHHI presenting symptoms
|
-pallor
-hypothermia -tremors/seizures -rapid breathing (tachypnea) -rapid heart rate (tachycardia) |
|
|
PHHI lab findings
|
hypoglycemia
decreased free fatty acids no ketones elevated cortisol and growth hormone elevated insuln, c-peptide |
|
|
PHHI treatment
|
IV glucose to maintain levels >80
diazoxide-block sulfonylurea receptors on beta cells, opening KATP channels and decreasing insulin release IV glucagon somatostatic analogues (octreotide) CCBs |
|
|
PHHI - when surgical treatment
|
-diazoxide unresponsive patients or those who have complications of treatment
-90% pancreatectemy |
|
|
PHHI- complications
|
-heart failure, poor nutrition, liver enlargement, obesity, hirsutism
-long term: seizures, neurological delay, diabetes post op |
|
|
Types of diabetes
|
Type I
Type II Gestational diabetes steroid induced diabetes other types of diabetes |
|
|
caused by autoimmune destruction,
of the pancreatic beta cell, leading to decreased insulin secretion. |
Type I diabetes
|
|
|
caused by insulin resistance due to
ineffective insulin cellular action; beta cell insulin secretion is usually preserved. |
Type II diabetes
|
|
|
Autoimmunity in diabetes?
|
-associated with Type I
-MHC-chr 6- >90% pts carry HLA DR3, DQB1*0201, HLA DR4,DQB1*0302 -anti-islet cell Ab, anti-GAD Ab |
|
|
typical incidence of diabetes, age of presentation
|
8-16 yrs
|
|
|
What happens in absence of insulin?
|
increased FFA, glycerol production (fat cell) leading to ketogenesis and gluconeogenesis (liver) and proteolysis (muscle)
-increased glucagon, glycogenolysis -increased cortisol, gluconeogenesis -incrs epinephrine, FFA and glycogenolysis, gluconeogenesis |
|
|
COMMON SIGNS OF DIABETES?
|
-incr thirst, urination
-weight loss (due to catabolic state) -vomiting (episodic, continuous) -fatigue and irritability -rapid breathing in absence of pulmonary disease |
|
|
How does diabetes affect kidney
|
-elevated serum glucose is filtered, much of which does not get reabsorbed and is excreted. this causes incr water excretion (polyuria), Na and K losses, promotes incr thirst (polydypsia) and dehydration
|
|
|
acute presentation diabetes
|
-Vomiting, dehydrated, air hunger, abd pain, rapid breathing (kussmaul), cyanosis.
-symptoms can mimic appendicitis, stomach virus, asthma -acidosis, hyperglycemia -treatment is ICU for fluids, IV insulin, close monitoring |
|
|
sub-acute presentation diabetes
|
-incr thirst, urination about 2-3 weeks duration. weight loss, incr or decr appetite, intermittent nausea, appear nearly well
-ketosis maay be present, no acidosis, mild hyperglycemia. -positive anti-islet cell and anti GAD Ab -treatment is insulin and education |
|
|
What is the best regimen of insulin
|
combination of long acting to cover basal needs, short acting to cover meal needs
|
|
|
Each meal insulin dose=
|
carb factor + premeal glucose factor
|
|
|
How do we monitor the long term glucose control of a patient?
|
-Hemoglobin A1C- irreversible non enzymatic association of glucose on the A1C subset of hemoglobin
|
|
|
Ideal HgA1C
|
5.5-6.9%
|
|
|
Acute diabetic complications
|
cerebral edema/thrombosis, arrhythmias/arrest
|
|
|
Chronic diabetic complications
|
1.retinopathy
2. nephropathy 3. neuropathy 4. psychological 5. cardiovascular 6. economic |
|
|
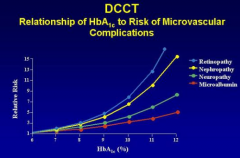
Relationship of HbA1C to risk of microvascular complications
|
|

