![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
51 Cards in this Set
- Front
- Back
|
Bradycardia is often secondary to what type of MI?
|
Inferior wall MI
|
|
|
By what means does morphine work in the tx of ACS and/or CHF pts?
|
Morphine:
• Calms the pt --> • Decr catecholamine levels --> • Reduces myocardial O2 consumption --> • Reduces incidence of fatal dysrhythmias Morphine also directly reduces preload and afterload (mildly) |
|
|
By what mechanism does cocaine cause MI?
Why are ß-blockers (relatively) contraindicated? |
Mechanism of MI:
• Hyperaggretory platelets • Vasospasm ß-Blockers contraindication: • Theoretic risk of reducing cardiac output in face of increased peripheral vascular resistance (unopposed alpha) |
|
|
Cardiac Enzymes: State the time to rise, peak and remain elevated for CK and Troponin
|
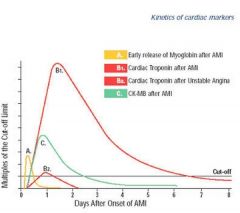
CK:
• Rise; 6 hrs • Peak: 12-24 hrs • Remains Elevated: 3-4 days Troponin: • Rise: 6 hrs • Peak: 12-18 hrs • Remains Elevated: 7-10 days |
|
|
Compare and contrast post-MI pericarditis with Dressler's syndrome.
• Etiology • When seen • EKG changes |
Post MI pericarditis:
• Due to pericardial inflammation • Seen 2-4 days post-MI • EKG changes are MASKED by the evolving EKG changes of the MI Dressler Syndrome: • Autoimmune • Seen 1 week to months post-MI • EKG findings typical of pericarditis |
|
|
Describe the beneficial physiologic effects of ß-blockers
|
• Decr HR & contractility --> decr myocardial O2 demand
• Incr time of diastole --> decr myocardial wall tension --> incr coronary blood flow • Decreases the rate of myocardial RUPTURE • Decreases rate of fatal DYSRHYTHMIAS, including Vfib |
|
|
Describe the EKG changes in POSTERIOR MI and the associated arterial occlusion.
Isolated posterior MIs are rare. With which other MI is it typically associated? |
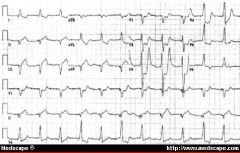
Left circumflex occlusion, OR
RCA • ST elevation in V8 and V9 • ST depression and tall R in I, aVL, V1 - V4 (especially V1 and V2) • UPRIGHT T waves (opposite of T wave inversion seen with other infarcts) Posterior MIs typically occur in conjunction with ANTERIOR or LATERAL MIs. |
|
|
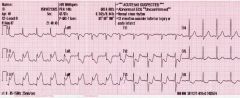
Describe the EKG findings in an ANTERIOR MI and the associated artery that is occluded.
Blocks? Pacing? |
LAD occlusion
• ST elevation in I, aVL, V1-V4 • Reciprocal ST depression in II, III and aVF Blocks LAD supplies blood to the right bundle and the left anterior fascicle. 1. NEW RBBB 2. NEW LEFT ANT FASCICLE block 2. Mobitz Type II Block TEMPORARY PACING may be required. |
|
|
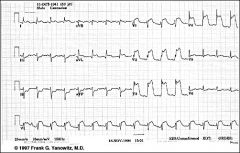
Describe the EKG findings in INFERIOR MI and the associated arterial occlusion.
Blocks/ dysrhythmias? |
RCA occlusion
• ST elevation in II, III, aVF • ST depression in I, aVL, V5, V6 Inferior MI predisposes to vagal dysrhythmias (sinus bradycardia and AVB) Note: The EKG changes are exactly reciprocal to anterior MI. |
|
|
Describe the EKG findings in LATERAL MI and the associated arterial occlusion
|
LAD/ Left circumflex occlusion
• ST elevation I, aVL, V5, V6 • ST depression in V1, V3R, V4R Lateral MI pts are at risk for developing LV dysfunction |
|
|
Describe the EKG findings in RV MI and the associated arterial occlusion.
What are the typical CV sequalae? |
RCA occlusion
• ST elevation in V3R and V4R RV MI pts are at great risk of developing HoTN and cardiogenic shock. HoTN in this setting will likely respond to IVF; morphine, nitrates and diuretics will further compound the HoTN Note: most RV MIs occur in association with an inferior MI |
|
|
How does the ST elevation of pericarditis differ from AMI?
|
Pericarditis -- CONCAVE ST elevation (Smiley face)
Diffuse ST elevation AMI -- Convex ST elevation |
|
|
In MI pts presenting to a non-PCI hospital, transfer to a PCI-capable hospital within how many hours of presentation improves outcome over thrombolysis alone?
|
2 hours
|
|
|
In the setting of ACS, which thrombolytic drugs should not be given w/ heparin?
|
Contraindications:
• Do not give with APSAC • Do not give with streptokinase |
|
|
State the ABSOLUTE contraindications to thrombolysis.
Suspicion of...? |
• Any h/o prior brain bleed
• Known structural CNS lesion (eg, AVM, tumor...) • Ischemic CVA w/in 3 mos (unless TIA < 3 hr) • Suspicion of AORTIC DISSECTION • Active bleeding or bleeding disorders |
|
|
State the AHA Class I (ie, tx benefit positively established) criteria for thrombolysis
|
• ST elevation > 0.1 in 2 or more contiguous leads
• Time to tx </= 12 hrs • Age < 75 •Old BBB obscuring ST segment analysis with hx suggesting AMI |
|
|
State the AHA Class IIa (ie, likely benefit) criteria for thrombolysis
|
• ST elevation > 0.1 in 2 or more contiguous leads
• Age > 75 |
|
|
State the AHA Class IIb (ie, may be beneficial) criteria for thrombolysis
|
• ST elevation > 0.1 in 2 or more contiguous leads
• Time to tx between 12 - 24 hrs • SP > 180 or DP > 110 associated with high risk of MI |
|
|
State the AHA Class III (ie, tx NOT indicated, may be harmful) criteria for thrombolysis
|
• ST elevation with time to tx > 24 hrs
• ST depression only • No ST elevation • POSTERIOR MI • Presumed NEW BBB |
|
|
State the beneficial effects of NTG in the setting of AMI
|
• Dilates collateral coronary vessels
• Has antiplatelet effects Decreases myocardial O2 demand by: • Decreasing preload • Decreasing LV end diastolic volume • Decreasing afterload (which makes it the drug of choice in pts with LV failure) |
|
|
State the blocks associated w/ INFERIOR MI. How are they treated?
|
• 1st degree AVB
• Mobitz Type I These blocks are associated with increased vagal tone. They respond to ATROPINE. |
|
|
State the blocks associated with ANTERIOR MI. Cause? Tx?
|
Mobitz Type II:
• Generally due to destruction of the infranodal conduction tissue. Sudden progression to complete block may occur • Tx with prophylactic pacemaker LAFB RBBB • RBBB + acute anterior MI = higher risk of developing complete heart block and cardiogenic shock |
|
|
State the cardiovascular benefits and mechanism of action of ASA
|
Benefits:
• Reduces the risk of AMI • Decreases mortality • Decreases infarct size • Decreases rate of reinfarction Mechanism: irreversibly acetylates platelet cyclo-oxygenase |
|
|
State the contraindications to ß-blockers in the setting of ACS
|
• Moderate to severe LV dysfxn (CHF)
• HR < 60 • SP < 100 • Active bronchospasm • 2nd or 3rd degree AVB • PR > 0.24 |
|
|
State the mechanism of action, INDICATIONS for, and contra-I to Glycoprotein IIb/IIIa receptor antagonists
|
Mechanism: Block the final common pathway of platelet aggregation in the presence of platelet activation
Indications: • In pts about to go to cath, give prior to the cath • ACS + refractory sxs • Confirmed NSTEMI • Elevated troponin level G IIa/IIIb antagonists are contraindicated post-cath! |
|
|
State the RELATIVE contraindications to thrombolysis
|
• Severe HTN on admission > 185/110
• Traumatic/ prolonged CPR (> 10 min) • Major SURGERY or internal bleeding w/in 3-4 WEEKS • Pregnancy • Coumadin use • PUD (active) |
|
|
State the temporal sequence of EKG changes in STEMI
|
1 Hyperacute T waves
2 ST elevation 3 T-wave inversion 4 Q waves |
|
|
State the timing of, and contraindictions to, ACE-I in ACS
|
ACE-I, when given w/in the 1st 24 hrs, decrease the incidence of ventricular dysfxn and death. ACE-I should not be given until 6 hrs after initial ACS tx has begun; may potentiate HoTN.
Contraindications: • Class III or IV heart failure • HoTN • Cr > 2.5 • Renal artery stenosis |
|
|
What are the Sgarbossa criteria for the diagnosis of AMI in the setting of LBBB?
|
Score of 3 or greater = high likelihood of AMI
5 Points: • Concordant ST elevation > 1 mm in 2 contiguous leads (ie, ST elevation in the same direction as the terminal portion of the QRS) 3 Points: • ST depression > 1 mm in V1-V3 2 Points: • Discordant ST elevation > 5 mm in 2 contiguous leads |
|
|
What is Dressler's Syndrome?
|
Late post-MI pericarditis
|
|
|
What is Prinzmetal's (variant) Angina?
What is it's relationship with excercise/ exertion? |
CP caused by coronary artery VASOSPASM
Prinzmetal's angina has NO ASSOCIATION with exercise -- the pain may increase, decrease or stay the same |
|
|
What is the approximate proportion of MIs that occur WITHOUT chest pain?
|
50%
|
|
|
What is the ddx of hyperacute T waves?
|
• Hyperkalemia
• Acute PERICARDITIS • Initial EKG change in STEMI • LVH • Benign early REPOLARIZATION |
|
|
What is the dose of SLNTG given to pts in severe pulmonary edema?
|
0.8 - 1.2 mg q 5 - 10 minutes
Note: use higher doses if BP is moderately or severely elevated |
|
|
What is the effect, if any, of thrombolytics on the incidence of post-MI pericarditis?
|
LOWER incidence
|
|
|
What is the incidence of post-MI pericarditis and:
• Transmural MI • Subendocardial MI? When is it typically seen? |
Transmural -- 20% + (b/c the cardiac injury extends TO the pericardium)
Subendocardial -- rare Seen 2-4 days post-MI |
|
|
What is the relative sensitivity and specificity of serum myoglobin as an indicator of cardiac injury?
Time to rise and peak? |
Very SENSITIVE --> good 'rule out' test (SNOUT)
Poorly specific Time to rise: 1-2 hours Time to peak: 6 hours |
|
|
What is the risk/consequence of hypokalemia in patients with acute or recent MI?
|
There is a 5 x greater risk of VFIB in hypokalemic pts with MI (if K < 3.9)
K should be maintained > 4.5 in MI pts to reduce risk of vfib |
|
|
What is the significance of T wave inversion without ST or Q wave changes?
|
Ischemia, not acute infarct
|
|
|
What percent of acute MIs are due to coronary vasospasm alone?
|
10%
|
|
|
What percent of pts with MI have initially normal EKGs?
Of this group, what is the rate of combined death and serious morbidity? |
Initially normal EKG -- 8%
Death/morbidity -- Nearly 20% |
|
|
What percent of women with acute MI experience atypical sx such as fatigue and insomnia one month prior to the event?
|
75%
|
|
|
Which artery supplies the AVN in 80% of the population?
|
RIGHT coronary artery
Left circumflex artery supplies the AVN in the remaining 20% |
|
|
Which leads are reciprocal to the inferior leads?
|
aVL, V2, V3
|
|
|
What is the treatment protocol for hypertensive emergency + acute pulmonary edema?
|
IV Nitroglycerine
Other agents: • Nipride IV -- use if BP remains elevated |
|
|
What is the treatment protocol for hypertensive emergency + acute renal insufficiency?
|
Drug of choice:
• Nipride Other agents: • Nifedipine • Labetolol Note: must monitor carefully for THIOCYANATE toxicity |
|
|
What is the treatment protocol for hypertensive emergency + AMI/ ischemia?
|
Nitroglycerine -- preferentially dilates coronary vasculature --> increases coronary perfusion
ß-Blockers -- Decrease myocardial O2 demand Other BP agents: • Nipride -- use if BP still remains elevated. Can increase myocardial ischemia via CORONARY STEAL syndrome |
|
|
What is the treatment protocol for hypertensive emergency + hemorrhagic CVA?
|
Mild to moderate BP reduction is generally well-tolerated (as opposed to ischemic CVA).
Severe HTN (> 220/120) should be judiciously controlled Drug of choice -- TITRATABLE agents: • Labetalol • Also, esmolol, enalapril, nicardipine |
|
|
What is the treatment protocol for hypertensive emergency + subarachnoid hemorrhage?
|
Drugs of choice -- Ca Ch Bls:
• Nimodipine • Nicardipine These agents lower BP but also DECREASE cerebral VASOSPASM that occurs following SAH. Goal of tx is to reduce BP to pre-hemorrhagic levels. |
|
|
What location of MI is typically associated with the following blocks:
• Mobitz I • Mobitz II • 3rd Degree AVB? |
Mobitz Type I: Inferior wall MI
Mobitz Type II: Anteroseptal MI 3rd Degree AVB (NARROW Complex): Inferior wall MI. Usually transient. 3rd Degree AVB (WIDE Complex): Anterior wall MI. Implies significant structural damage. |
|
|
Which location of infarct is most susceptible to HoTN after administration of NTG?
|
Inferior wall MI with associated RV infarct
|

