![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
81 Cards in this Set
- Front
- Back
|
Long history of progressive neurological symptoms (seizures, headache focal signs)
Well defined hypodense/hypointense mass |
Oligodendrioglioma
Grade II=Olidodendroglioma Grade III=Anaplastic oligodendroglioma |
|
|
Allelic loss of chromosome 1p and 19q indicate?
|
Better prognosis/susceptibility to chemotherapy in anaplastic oligodendrogliomas
|
|
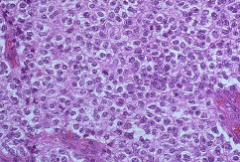
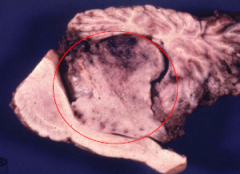
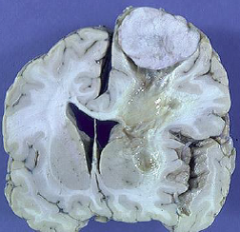
Round Fried egg cells; calcifications
Grossly firm large area |
Oligodendroglioma
|
|
|
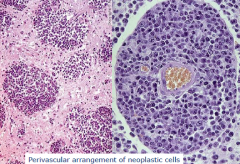
Tumor that occurs along the ventricular system; usually posterior fossa (4th ventricle)
Hydrocephalus, occasionally seizures In children and young adults; avg survival is 4 years |
Ependymona
they can invade parenchyma through subarachnoid space |
|
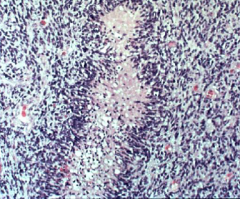
?
|
Ependymoma
|
|
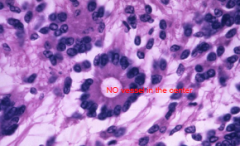
True Rossets (columnar cells arranged around a central lumen)
|
Ependymoma
|
|
|
Occurs in the 4th ventricle, lateral ventricle, 3rd ventricle, and cerebello-pontine angle
Presentation with hydrocephalus d/t overproduction of CSF and obstruction of CSF flow |
Choroid plexus papilloma
Very good prognosis with surgical resection |
|
|
Choroid plexus etiology
|
Occurs in children <10 years; Very poor prognosis
|
|
?
|
Choroid plexus papilloma
|
|
|
Presentation of colloid cyst (cuboid columnar epithelium)
|
Attached to roof of third ventricle
Intermittent obstruction of foramen of Monroe Positional headache |
|
|
Presentation of Ganglioglioma
|
Presents in first 3 decades
Long standing history of seizures Solid or cystic imaging (looks like a pilocytic astrocytoma) Surgical resection is usually curative |
|
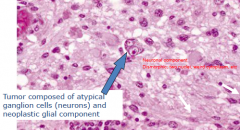
?
|
Ganglioglioma
|
|
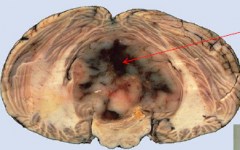
Primitive neuroectodermal neoplasm of posterior fossa; 1/3 of pediatric posterior fossa tumors
Well defined contrast enhancing mass with possible leptomeningeal spread |

Medulloblastoma
Treat with surgical resection followed by radiation |
|

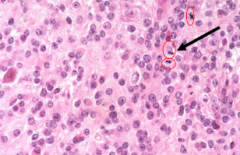
?
|
Medulloblastoma
|
|
|
Etiology of Primary CNS lyphoma
|
40-60 year olds
In Post-transplant pts, AIDS, and EBV B-Cell Poor prognosis: most die w/in one year Symptoms are non-specific, referable to mass lesion |
|
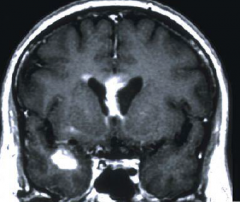
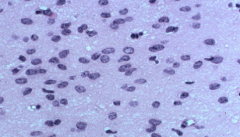
Multiple periventricular lesions
|
Primary CNS lymphoma
|
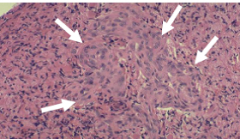
|
?
|
Primary CNS lymphoma
|
|
|
Meningioma etiology
|
women>men
Middle to late adult life Most common extraparenchymal neoplam of CNS Sx d/t enlarging mass |
|
What grade are meningiomas typically?
|
Grade I
|
|
Sheets of tumor cells with indistinct border
|
Menignioma
|
|
|
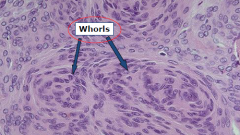
Histological features of Meningioma
|
Whorls, Psammonmma bodies, meningioma infiltrating bone
|
|
|
Most mailgnant tumors originate from?
|
Lung or breast carcinomas
Poor prognosis, most die within a few months |
|
|
Metastasis to vertebral bodies usually originates from
|
Prostatic adenocarcinoma
presents with spinal cord compression |
|
|
Tumor that involves peripheral nerves in the head and neck and flexor surfaces of extremities
contrast enhancing mass Associated with neurofibromatosis type 2 Compact spindle cells (Antoni A tissue) Antoni B tissue-->loose spongy areas, small cells with round nuclei Include sx |
Schwannomas
Spinal-->radicular pain tumor in cerebellopontine angle-8th nerve-->Hearing loss, tinnitis, and facial numbness |
|
|
Benign tumor composed of Schwann cells, fibroblasts, and perineural cells
Associated with Neurofibromatosis type 1 |
Neurofibroma
|
|
|
Cutaneous or Peripheral Neurofibroma associated with Neurofibromatosis type I
|
Peripheral (particullary type 1)
Cutaneous is more common |
|
|
Does Neurofibroma or Schwannoma compress the nerves?
|
Schwannoma
Neurofibroma make the nerves swell and push apart the axons |
|
|
Cutaneous or Peripheral Neurofibroma associated with malignant transformation?
|
Peripheral Plexiform Neurofibroma
Infiltrative, non-encapsulated fleshy masses; Highly cellular, moderate to marked nuclear pleomorphism |
|
|
Presentation of Neurofibromatosis 1
|
Autosomal dominant
Cafe-au-lait spots, Lisch nodules (pigmented hamartomas in iris), optic glioma, osseous lesions, axillary freckling, family history NF1 gene on Chromosome 17; product is neurofibromin |
|
|
Gene for Neurofibromatisis II
|
Chromosome 22; product is merlin
Autosomal dominant Bilateral vestibular schwannomas, menigiomasa, schwannomas, gliomas, neurofibromas, lens opacity, cerebral calcifications |
|
|
Hemangioblastomas of CNS and retina
Renal cell carcinoma Pheochromocytoma Visceral Cysts |
Von Hippl Lindau Disease
on Chromosome 3 |
|
|
40 year olds
in Cerebellum sx relate to incr. intracranial pressure MRI shows well difined contrast enhancing cystic mass with mural nodule |
Hemangioblastoma
|
|
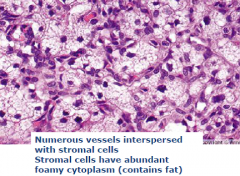
?
|
Hemangioblastoma
|
|
|
Tuberous sclerosis is associated with?
|
Cardiac rhabdomyomas and cutaneous angiofibromas
Tubers (firm areas in cortex; collection of neurons) |
|
|
Large pleomorphic multinucleated tumor cells with eosinophilic cytoplasm
|
Subependymal giant cell astrocytoma
|
|
|
A clinical syndrome with remote effect on the nervous system without direct invasion
Initial screening may be negative; Subacute worsening over weeks to months |
Paraneoplastic syndrome
Small cell carcinoma and gynecologic malignancies most common Related to ectopic hormone production: SIADH, ACTH Present with subacute cerebellar ataxi and Lambert-Eaton myasthenic syndrome |
|
|
Subacute cerebellar ataxia
|
Paraneoplastic neurologic syndromes
Progressive ataxia, dysarthia, nystagmus, vertigo, diplopia, titubation Antibody to Purkinje cells |
|
|
Lambert Eaton Myasthenic Syndrome
|
Paraneoplastic neurologic syndromes; muscle weakness (legs) that improves with testing on exam
Antibodies to voltage-gated calcium channels Commonly associated with Small cell lung cancer |
|
|
What are some red flags for headache presentation?
|
A very low chance of having significant intracranial pathology
First or worst, abrupt onset New headache whem <5 or >50 Cancer, HIV, pregnancy Abnormal physical exam Onset with seizure, sex or Valsalva |
|
|
Headache is a symptom reflecting underlying pathology
|
Secondary headache
|
|
|
What are the types of primary headaches?
|
Migraine, Cluster, and Tension-Type
|
|
|
What are the pain sensitive intracranial structures?
|
Meningeal arteries, proximal portions of the cerebral arteries, dura at the base of the brain, CN 5,7,9 and cranial nerves 1-3, venous sinuses
|
|
|
CT or MRI is warranted in?
|
Recent change in headache pattern
New onset seizures Focal neurologic signs or symptoms |
|
|
What is the most common headache seen in primary care practices?
|
MIgraine
|
|
|
Cluster headache?
|
Frequency: one every other day to 8/day; occurs during winter and summer solstice
Severe, Unilateral (orbital, supraorbital or temporal) Lasts 15 to 180 minutes Need one of the following (autonomic problems): Lacrimation, rhinorrhea, miosis, ptosis, nasal congestion, forehead sweating |
|
|
Migraine?
|
Frequency: lasts 4 to 72 hours (longer than cluster)
Need 2: Unilateral, Pulsating, Moderate or severe intensity, physical activity makes worse Need 1: Nausea, vomiting, photophobia, phonophobia |
|
|
What are the best predictors of migraine?
|
Nausea, disability, photophobia
|
|
|
Tension-Type Headache?
|
Frequency: lasts hours or may be continuous; lasts 15 days/month for >3 months
Need 2: BILATERAL, Pressure quality (not pulsating), Mild or moderate intensity (can still do activities) Cant have more than one of Nausea, photophobia, etc |
|
|
What are the causes of tension headache
|
Stress, can lead to neck pain
|
|
|
What is the proposed mechanism of migraines?
|
Activation of trigeminovascular system leads to headache
Abnormal brainstem function Both from cortical neuronal hyperexcitability (mutations or elevate glutamate, low Mg+2. Altered brain energy metabolism) |
|
|
Cortical spreading depression
|
Cortical activity-->increase rCBF-->neuronal suppression-->decrease in rCBF (headache onset)
|
|
|
Activation of trigeminovascular system is d/t
|
Aracadonic acid, NO, H+, and K+
|
|
|
Dysfunction in Periaquductal gray region can lead to?
|
Headache/migraine
|
|
|
Serotonin is derived from and what is the RLS in formation?
|
Tryptophan; Tryptophan hydroxylase
|
|
|
What is the metabolism and termination of serotonin?
|
Monoamine oxidase metabolizes to 5-hydroxyindole acetic acid
Termination by high affinity active uptake (SERT) |
|
|
Serotonin is converted to melatonin where?
|
Pineal Gland
|
|
|
Where is serotonin primarily?
|
In the GI system
|
|
|
Where is serotonin in the CNS located?
|
Raphae Nuclei
|
|
|
5-HT1 receptor action
|
Inhibition of adenylate cyclase; also opens K+ channel (Gi)
|
|
|
5-HT2 receptor action
|
PI hydrolysis (Gq)
|
|
|
5-HT3 receptor action
|
NOT a G-protein coupled receptor; Ligand-gated cation channel
|
|
|
5-HT4-7 receptor action
|
Activation of adenylate cyclase (Gs)
|
|
|
CV effects of serotonin
|
Vasoconstriction of large vessels
Vasodilation in coronary, sk muscle, and cutaneous blood vessels Bezold-Jarisch reflexbradycardia, hypotension, hypoventilation Platelet aggregation |
|
|
CNS effects of serotonin
|
Sensory perception, sleep, temperature reg, neuroendocrine regulation (release hormones) short term memory, Pain perception
|
|
|
Odansteron is used to treat?
|
Nausea and vomiting
|
|
|
Cyproheptadine is used to treat?
|
Itch
|
|
|
Sumatriptan?
|
5-HT1B/D receptors on cerebral blood vessels; treatment of migraine headaches; constricts vessels
|
|
|
Major class of drugs to stop existing headaches
|
Triptans
Frova and Nara have long halflife Suma is in combo with naproxen Promote vasoconstriction, block brainstem pain pathways, inhibit trigeminal nucleus caudalis |
|
|
Side effects of triptans
|
Vasoconstriction
Nausea and vomiting Angina Dizzines Flushing |
|
|
Ergots stimulate what receptors?
|
Serotonin, Dopamine, and Norepi receptors
|
|
|
Level A migrane prophylaxis drugs
|
Divalproex Sodium and Topiramate (both antiseizure agents)
Beta blockers-Propranolol and Atenolol (decrease blood flow) Trycyclic antidepressants |
|
|
Where do adult CNS tumors most often occur?
|
Frontal lobes
|
|
|
Where do most kid CNS tumors occur?
|
Posterior fossa
|
|
|
Most common glial tumor
|
Astrocytomasdiffuse astrocytoms have a tendency to become anaplastic over time
S/S include seizures, focal deficits, headache |
|
|
Mean age for Astrocytoma, Anaplastic astrocytoma, and glioblastoma multiforme
|
35, 45, and 61; grades 2-4 respectively
|
|
|
Astrocytoma: cellularity is moderately increased and occasional nuclear atypia
|
Grade 2 diffuse astrocytoma; Gross is diffuse enlargement, can have herniation
|
|
Astrocytoma: Increased cellularity, distinct nuclear atypia, marked mitotic activity
|
Grade 3 anaplastic astrocytoma
|
|
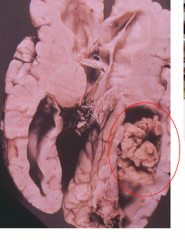
Astrocytoma: Pleomorphic astrocytic cells, brisk mitotic activity, PROMINENT microvascular proliferation and necrosis
|
Grade 4 Glioblastoma multiforme; A lot of necrosis and hemorrhage grossly; Pseudopalisading (tumor cells align with central area of necrosis
|
|
|
Pilocytic astrocytoma-location and etiology
|
Presents in first two decades; most commonly in cerebellum (also optic nerve, 3rd ventricle, hypothalamus and brainstem); Slow growing good prognosis
|
|

|
Pilocytic astrocytoma
|
|
|
Histology of Pilocytic astrocytoma
|
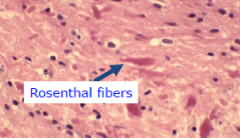
Hair like (elongated fibrillary cells); Rosenthal fibers
|

