![]()
![]()
![]()
Use LEFT and RIGHT arrow keys to navigate between flashcards;
Use UP and DOWN arrow keys to flip the card;
H to show hint;
A reads text to speech;
28 Cards in this Set
- Front
- Back
|
Different causes of hypoxia
|
Low level of oxygen of blood (CO poisoning, drowning)
Low blood flow (aka ischemia) Oxygen utilization by tissue is impaired (cyanide poisoning) |
|
|
Low blood flow
|
Ischemia; causes more damage than hypoxia; no outflow of metabolites
|
|
|
Global ischemia is defined as?
Where is brain damage most severe? |
systolic pressure <50 mmHg (d/t shock, heart attack, shock)
Brain damage is most severe in watershed areas; if severe enough vegetative state or brain death may occur |
|
|
Focal ischemia is typically d/t?
|
arterial stenosis, thrombosis, atheroemboli, or thromboemboli
|
|
|
Where are the watershed areas?
|
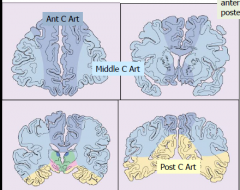
Between ACA and MCA
Between MCA and PCA |
|
|
What are the selective vulnerable regions Cells and regions?
|
Cells: Neurons>Oligodendroytes>astrocytes
Regions: Hippocampus (CA1 sector)>lamina 3 and 5 of cortex>Purkinje cells in cerebellum |
|
|
What determines the selective vulnerability?
|
Variable oxygen/energy requirements of different neurons and neuronal populations
Glutamate receptor densities-->glutamate is neurotoxic when present in excess, as occurs in hypoxic/ischemic brain damage |
|
|
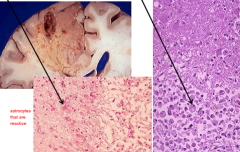
Acutely hypoxic/ischemic neurons histological appearance?
|

"red is dead"
shrunked and dark nucleus, no nucleolus visible Red cytoplasm (no Nissl substance) |
|
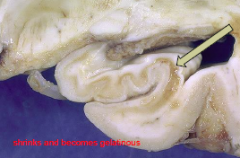
Pathology?
|
Hippocampal infarct; loss of neurons in the CA1 sector of the hippocampus d/t selective vulnerability
|
|
|
Most common sites of thrombosis (atherosclerosis)
|
Carotid bifurcation
Origin of MCA origin or end of basilar artery |
|
|
Common sources of Emboli?
|
Cardiac: Mural thrombus-->left atrium or ventricle (d/t afib, MI, valve disease)
Non-Cardiac Source-->Atheroma (plaques in carotid aa.) Fat, neoplasm, air |
|
|
What is the most frequent vessel affected by emboli?
|
Middle cerebral artery is most frequent vessel affected by emboli
|
|
|
Hyaline arhteriolosclerosis caused by hypertension and diabetes mellitus?
|
Lacunar infarcts/slit hemorrhages
|
|
|
Chronic inflammation, fibrinoid necrosis of the wall; multinucleated giant cells and wall destruction
|
Primary angiitis (vasculitis) of CNS
|
|
|
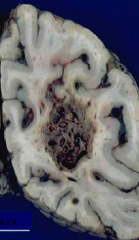
Acute, subacute, and chronic gross morphology of infarct
|
Actue-->up to 48 hours: soft, swollen, gray white distinction blurred
Subacute: up to 2-3 weeks: liquefactive necrosis Chronic: several months: CAVITATED, all dead tissue removed |
|
|
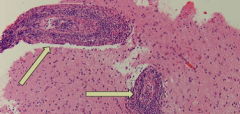
Acute, subacute, and chronic microscopic morphology of infarct
|
Acute: red neurons pallor, up to 48 hours-->neutrophils
Subacute: macrophages, necrotic tissue, reactive astrocytes, vascular proliferation (picture) Chronic: several months: cavity with GLIAL SCAR |
|
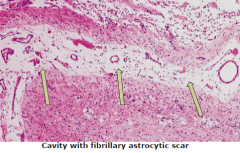
Pathology?
|
Chronic infarct
|
|
|
Typical locations of venous thrombosis?
D/t? |
Usually superior sagittal sinus or lateral sinuses
Results in parasaggital hemorrhagic infarct Infection, injury, neoplasm, surgery Pregnancy, oral contraceptives, hematologic abnormalities, dehydration and malignancy |
|
|
Most common cause of intracerebral hemorrhage (ICH)
Common locations? |
Hypertension
Putamen, thalamus, pons, cerebellum |
|
|
Weakens the arteriole and predisposes to rupture?
|
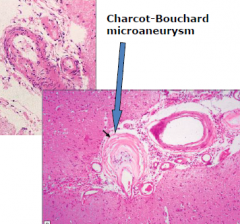
Hyaline arteriolosclerosis
|
|
What age group presents with arteriovenous malformations? (Tangled network of vessels with arteriovenous shunt)
|
M>F
Presentation between 10-30 years Most often distribution of MCA |
|
|
Capillary telangectasia: location? bleed? Intervening brain tissue?
|
Pons
DONT usually bleed Capillary telangiectasia |
|
|
Cavernous angioma: location? bleed? Intervening brain tissue?
|
Cerebellum, pons, white matter
Evidence of prior bleeding (greatly enlarged blood vessels are evidence of prior hemorrhage) NO intervening brain tissue |
|
|
Lobar hemorrhage causes (closer to the surface of the brain)
|
Neoplasms, drug abuse, vasculitis, hemorrhagic diathesis, amyloid angiopathy
|
|
|
The work headache ever!
|
Saccular (Berry) aneurysims-->subarachnoid hemorrhage; mosly by the ACA/ant comm artery
Increased risk with HTN, smoking, AVM DEFECT in media is CONGENITAL |
|
|
Strokes that are in large vessels or at the end branches
|
"pump" Cardioembolism stroke
|
|
|
Hypoperfusion if no flow?
Low flow? |
NO flow=cortical laminar necrosis
Low flow=watershed injury |
|
|
Sites for lacunes and hemorrhages
|
Basal Ganglia, pons, thalamus, cerebellum
|

